Suspected Deep Tissue Injury: Depth Unknown
Purple or maroon localised area of discoloured intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue.
Deep tissue injury may be difficult to detect in individuals with dark skin tones. Evolution may include a thin blister over a dark wound bed. The wound may further evolve and become covered by thin eschar. Evolution may be rapid exposing additional layers of tissue even with optimal treatment.
Source: Prevention and Treatment of Pressure Ulcers: Quick Reference Guide
When To Get Medical Advice
If you’re in hospital or a care home, tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer. It’ll probably continue to get worse if nothing is done about it.
You should be regularly monitored and offered advice and treatment to reduce the risk of pressure ulcers, but sometimes they can develop even with the highest standards of care.
If you’re recovering from illness or surgery at home, or you’re caring for someone confined to bed or a wheelchair, contact your GP surgery if you think you or the person you’re caring for might have a pressure ulcer.
Get medical advice immediately if there is:
- red, swollen skin
- pus coming from the pressure ulcer or wound
- cold skin and a fast heartbeat
- severe or worsening pain
- a high temperature
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
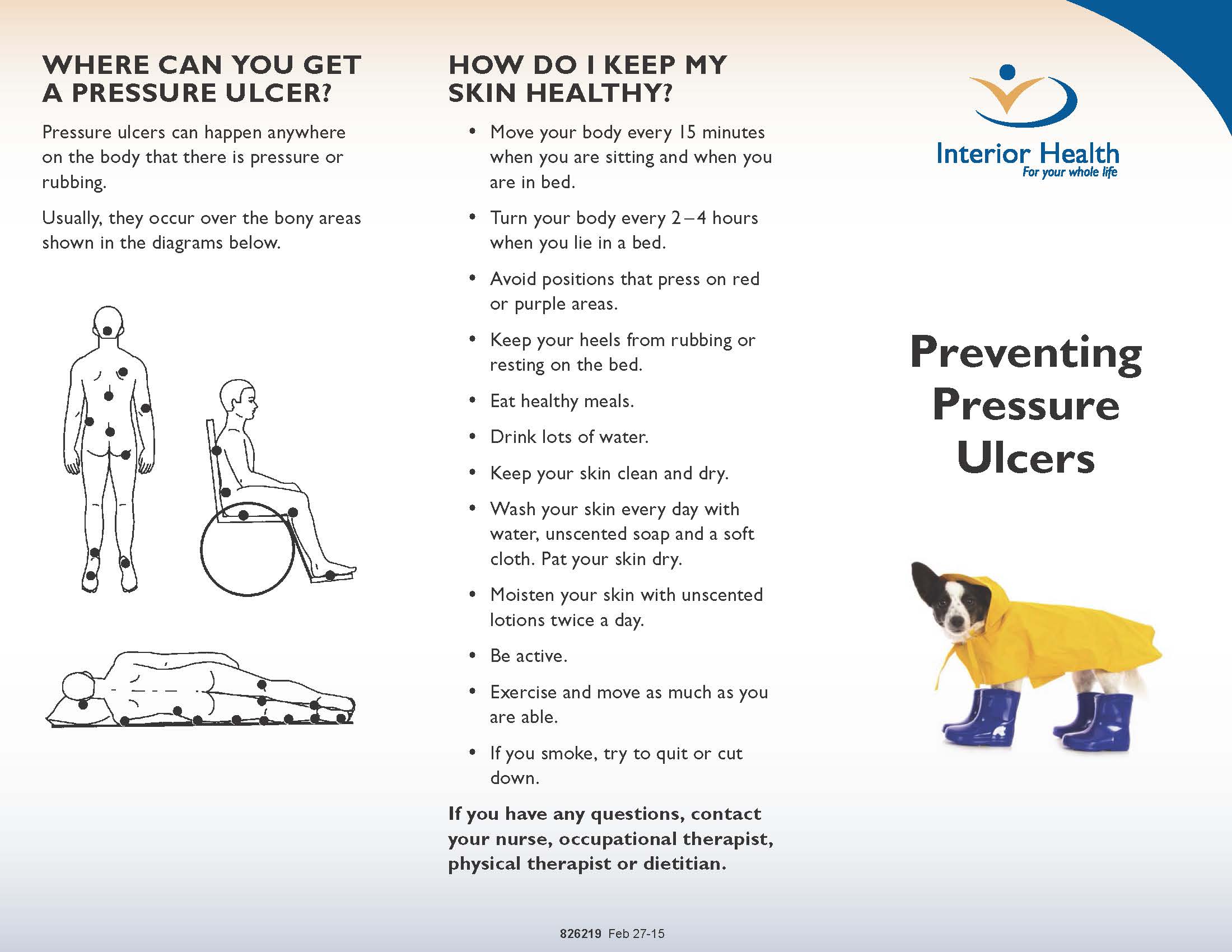
What Are Pressure Sores
Pressure sores are sores on your skin. Theyre caused by being in a bed or wheelchair nearly all the time. Sometimes theyre called bedsores or pressure ulcers. The sores usually develop over the bony parts of your body. Those are places with little padding from fat. Sores are common on heels and hips. Other areas include the base of the spine , shoulder blades, the backs and sides of the knees, and the back of the head.
People who need to stay in bed or in a wheelchair for a long time are at greater risk of developing pressure sores. This can include people who are paralyzed and those who arent able to get up on their own. But even some people with short-term illness and injuries can get pressure sores. Sores can happen if they have to stay in bed or a wheelchair while they heal. Lastly, some chronic diseases make it hard for pressure sores to heal. Those include diabetes and hardening of the arteries.
You May Like: Is Soy Sauce Ok For Ulcerative Colitis
Stage 2 Pressure Injury: Partial
In stage 2 pressure injuries there is a partial-thickness loss of skin with exposed dermis. The wound bed is pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Fat and deeper tissues are not visible. Connective granulation tissue and eschar are also not present. Stage 2 injuries are a common result of an adverse microclimate and shear in the skin. For visual reference, see illustrations of pressure injuries from the NPUAP here.
What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Also Check: How To Prevent Pressure Ulcers In Wheelchairs
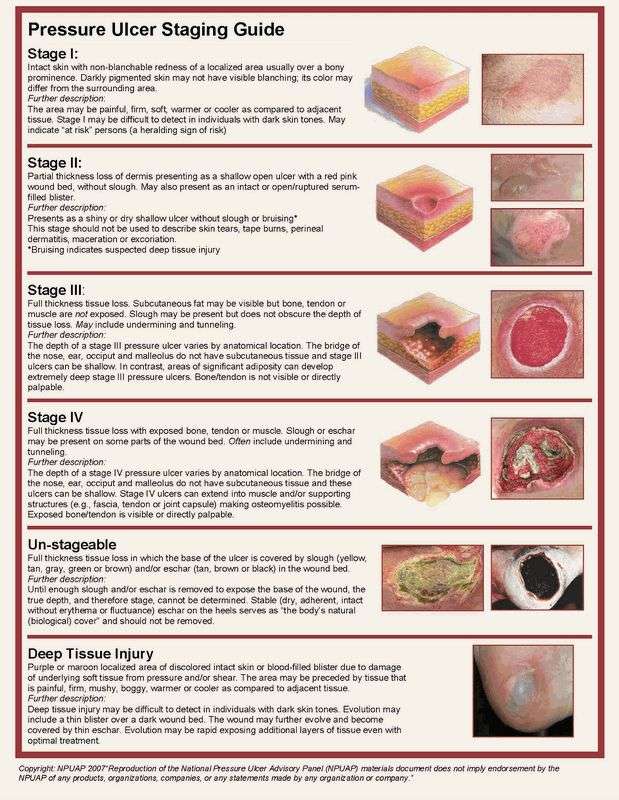
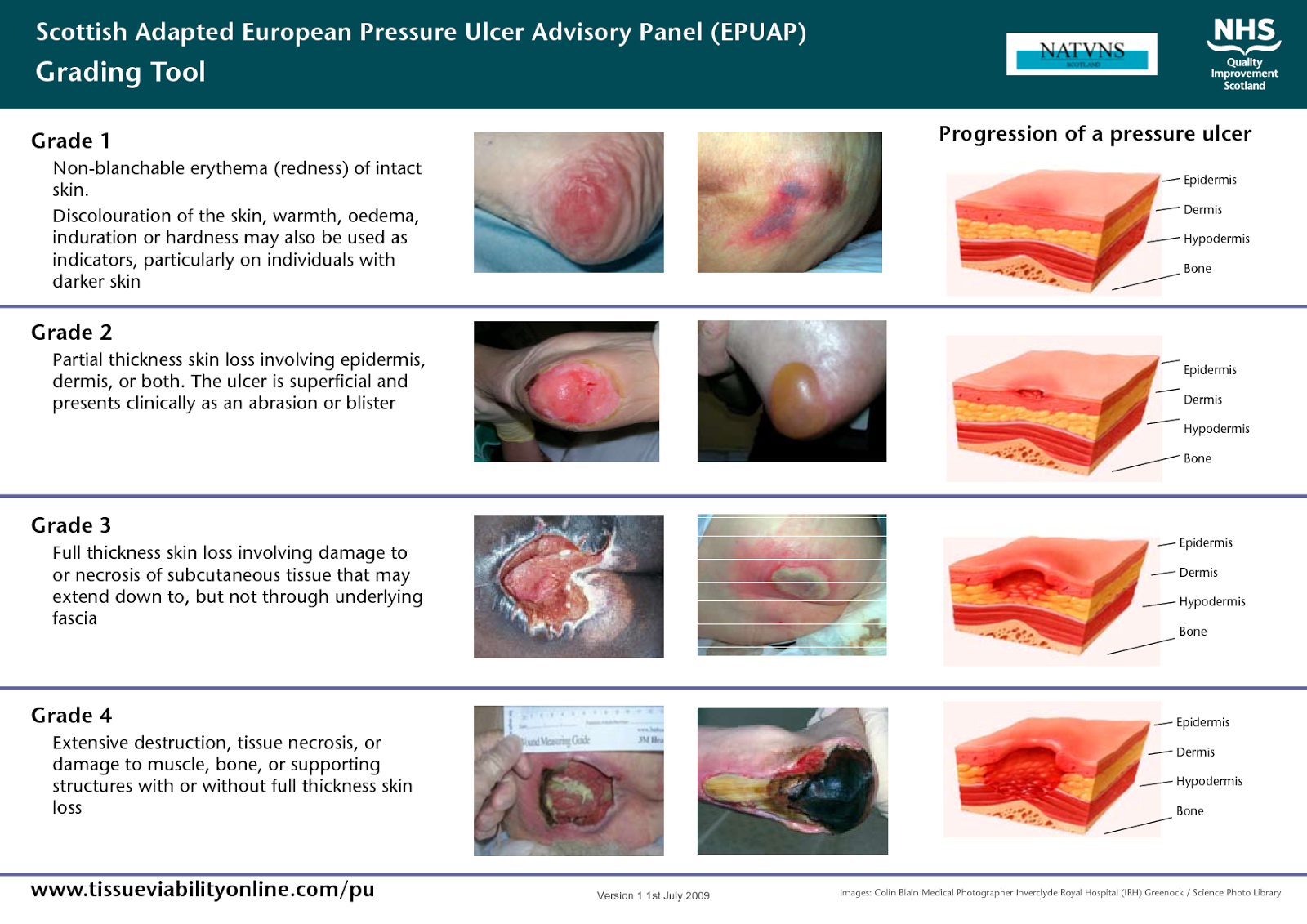
Stage Iii: Full Thickness Skin Loss
Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunnelling.
The depth of a Category/Stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and Category/Stage III ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep Category/Stage III pressure ulcers. Bone/tendon is not visible or directly palpable.
Stage Iv: Full Thickness Tissue Loss
Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunnelling.
The depth of a Category/Stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and these ulcers can be shallow.
Category/Stage IV ulcers can extend into muscle and/or supporting structures making osteomyelitis possible. Exposed bone/tendon is visible or directly palpable.
Also Check: Align Probiotic For Ulcerative Colitis
Key Points About Bed Sores
- Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period.
- Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile.
- Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas.
Risk Factors For Pressure Ulcer
There are several types of risk factors for developing pressure ulcers. If a person is suffering from any of these conditions, the risk of developing bed sores get even higher. Here they are:
Poor Mobility/Immobility – People who are unable to change their position independently or completely immobile are at greater risk of developing pressure ulcers. Poor health, spinal cord injury, and other causes can lead to immobility.
Lack Of Sensory Perception – People with loss of sensation due to spinal cord injury, or neurological diseases are more prone to an increased risk of developing a pressure ulcer. The person with sensory loss is unable to feel pain and discomfort after lying or sitting in a position for a long period.
Changes In Mental Status – If a person is suffering from dementia or other cognitive disorders may be unable to understand the given instructions helpful in preventing pressure ulcers. They may also be unable to sense discomfort as a necessary signal to change position.
Incontinence – It can lead to skin damage which can further increase the risks of developing pressure ulcers. Due to the skin damage, it can be more complex for wound care experts to recognize the signs of pressure ulcers.
You May Like: Mouth Ulcer On Tongue Remedies
Suspected Deep Tissue Injury
This is formed as a result of the damage to the soft tissue underlying the affected skin due to pressure and/or shear. The result is a maroon or purple-colored or discolored skin, or the formation of a blister filled with blood on the skin above that tissue. Before such formation, the patient may experience pain, bogginess, warmness or coolness, firmness or mushiness compared to the tissue next to it.
It is not easy to detect this deep-tissue injury if the person has a dark complexion. This patch on the skin may eventually evolve into a thin blister. Further, it may evolve into a wound and be covered by a thin eschar. Irrespective of the efficiency of the treatment, the evolution of the wound will be rapid exposing more and more layers of the tissue.
What Are The Symptoms Of Bedsores
Bedsores are divided into 4 stages, from least severe to most severe. These are:
- Stage 1. The area looks red and feels warm to the touch. With darker skin, the area may have a blue or purple tint. The person may also complain that it burns, hurts, or itches.
- Stage 2. The area looks more damaged and may have an open sore, scrape, or blister. The person complains of significant pain and the skin around the wound may be discolored.
- Stage 3. The area has a crater-like appearance due to damage below the skin’s surface.
- Stage 4. The area is severely damaged and a large wound is present. Muscles, tendons, bones, and joints can be involved. Infection is a significant risk at this stage.
A wound is not assigned a stage when there is full-thickness tissue loss and the base of the ulcer is covered by slough or eschar is found in the wound bed. Slough may be tan, grey, green, brown, or yellow in color. Eschar is usually tan, brown or black.
You May Like: Low Residue Diet For Ulcerative Colitis
Stages Of Pressure Ulcers
Casey Gallagher, MD, is board-certified in dermatology and works as a practicing dermatologist and clinical professor.
If a loved one has been severely injured or is extremely ill, they may need to spend a significant amount of time in bed. Prolonged immobility, while beneficial to recovery, can become problematic if it places persistent pressure on vulnerable skin. Unless preventive steps are taken, pressure ulcers, also known as decubitus ulcers or bedsores, can develop.
Does The Assessment Of Risk Factors Prevent The Development Of Pressure Ulcers In Hospitalised Patients
clinical question, which I formulated. My clinical question is based upon Does the assessment of risk factors prevent the development of pressure ulcers in hospitalised patients. I will be discussing and analysing my questions and findings from reliable, current, valid and trustworthy sources found within five articles based on the subject of pressure ulcers. All articles are based on quantitative research undertaken. From the findings of a good, current, reliable, valid or trustworthy research
You May Like: Over The Counter Medication For Ulcerative Colitis
The Prevalence Of Pressure Ulcers
The prevalence of pressure ulcers in elderly patients is of an epidemic proportion . The annual cost of treating pressure ulcers in the United States is estimated at more than $20 billion and is increasing . Pressure ulcers occur when an injury is caused to the skin and underlying tissue at the pressure points resulting in transient or permanent damage to the underlying tissue . The prevalence is seen in patients who
Link Cause Effect And Prevention Of Pressure Ulcers
A pressure ulcer is an area of skin with unrelieved pressure resulting in ischemia, cell death, and necrotic tissue. The constant external pressure or rubbing that exceeds the arterial capillary pressure and impairs local normal blood flow to tissue for an extended period, results in pressure ulcer . According to National Pressure Ulcer Advisory Panel, 2014, pressure ulcers are a major burden to the society, as it approaches $11 billion annually, with a cost
Read Also: Ulcerative Colitis Left Side Pain
The Four Stages Of Pressure Injuries
We know pressure injuries are dangerous for our patients and costly for our medical system, so the question becomes, how can we recognize them in order to guard against them? Pressure injuries are broken into four stages, where the stage indicates the extent of tissue damage. Following are the key indicators for each stage.
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Also Check: Things To Eat When You Have An Ulcer
Symptoms Of Stage 3 And Stage 4 Pressure Ulcers
Stages 3 and 4 pressure ulcers have deeper involvement of underlying tissue with more extensive destruction. Stage 3 involves the full thickness of the skin and may extend into the subcutaneous tissue layer granulation tissue and epibole are often present. At this stage, there may be undermining and/or tunneling that makes the wound much larger than it may seem on the surface. Stage 4 pressure ulcers are the deepest, extending into the muscle, tendon, ligament, cartilage or even bone.
Figure 1: Stage 4 sacral pressure ulcerFigure 2: Stage 3 pressure ulcer on hip
Stage Ii: Partial Thickness Skin Loss
Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough.
May also present as an intact or open/ruptured serum-filled blister. Presents as a shiny or dry shallow ulcer without slough or bruising.*
This Category/Stage should not be used to describe skin tears, tape burns, perineal dermatitis, maceration or excoriation.
*Bruising indicates suspected deep tissue injury
Also Check: What Is An Ulcer Diet
What Are The Different Stages Of Pressure Ulcers
4.9/5Pressure injuries are described in four stages:
- Stage 1 sores are not open wounds.
- At stage 2, the skin breaks open, wears away, or forms an ulcer, which is usually tender and painful.
- During stage 3, the sore gets worse and extends into the tissue beneath the skin, forming a small crater.
Pressure ulcers can progress in four stages based on the level of tissue damage.
Subsequently, question is, what is a Stage 1 pressure ulcer? Stage 1 pressure injuries are characterized by superficial reddening of the skin that when pressed does not turn white . If the cause of the injury is not relieved, these will progress and form proper ulcers.
Subsequently, one may also ask, what is a Stage 3 pressure ulcer?
Pressure ulcers are localized areas of tissue necrosis that typically develop when soft tissue is compressed between a bony prominence and an external surface for a long period of time. Stage 3 pressure ulcers involve full-thickness skin loss potentially extending into the subcutaneous tissue layer.
What does a Stage 4 bedsore look like?
Symptoms of stage 4 bedsores include:Exposed tissue or bone. Blackened skin. Drainage and pus. Hot skin.
Selection Of Studies And Data Extraction
At first, all articles in which the incidence of pressure ulcer was noted among were collected by two independent researchers. The inclusion criteria were: observational studies that reported a pressure ulcer, access to full text of articles, and publication of articles in English. To minimize the risk of bias assessment, searching for articles, selecting studies, evaluating the methodological quality of articles, and extracting data independently were done by two researchers, and any disagreement was resolved by discussion. Exclusion criteria included lack of addressing the risk factors for the incidence of pressure ulcers, being a duplicate, and review articles. A form was used to record the selected information, including the name of the first author, year of publication, geographical location of the study, ward, type of scale, sample size, and the mean age of patients. We assessed the methodological quality of articles based on the ten selected items of the Strengthening the Reporting of Observational Studies in Epidemiology checklist .
Read Also: Whey Protein And Ulcerative Colitis
Symptoms And Treatment Of A Pressure Ulcer
A pressure ulcer is defined as a localized injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure, or pressure in combination with shear, according to the National Pressure Ulcer Advisory Panel, abbreviated NPAUP . NPUAP redefined the definition and classification of a pressure ulcer in 2007. As a result of the modification, stages I-IV, the four original stages, underwent alterations to their existing classifications and definitions. In
If A Pressure Ulcer Develops
If a pressure ulcer develops, the earlier its caught, the better. Keeping all pressure off the area will help the skin heal. If the skin breaks, speak to your doctor or healthcare team about how best to treat the sore. Generally, it should be cleaned well and protected from pressure and moisture. Stage 3 or 4 ulcers will need medical care.
Don’t Miss: Cbd Oil For Stomach Ulcers
Why Is It Important To Recognize Pressure Injuries
Certainly, the primary reason for wanting to recognize and treat pressure injuries when they occur is for optimal patient care, but there is a secondary reason that should reinforce vigilance for all medical practitioners. In 2013 the National Quality Forum Specifically, they stated that stage 3 and 4 pressure injuries that occur after admission to a healthcare facility are unacceptable and unnecessary. This inclusion as a ânever eventâ brought with it financial implications for pressure injuries â in the simplest of terms, the Centers for Medicare and Medicaid Services ruled that they can deny Medicare payment for hospital-acquired conditions that fall under the category of ânever events,â making pressure injuries costly in more ways than one.
Other Tips For Preventing Pressure Ulcer
1. Check the skin daily for any signs or symptoms of pressure ulcers. The patients can take the help of Bedside Wound Care Services for this. 2. Maintain a healthy and balanced diet that contains sufficient and enough protein with good sources of vitamins and minerals.3. Quit smoking. People who smoke are more prone to develop pressure ulcers due to the damage caused to blood circulation. 4. For repositioning, wheelchair push-ups are good where the person can raise their body off the seat by pushing on the arms of the chair. The use of cushions or special mattresses is also prescribed to release pressure and ensure a well-positioned body. Avoid doughnut cushions as they can put pressure on surrounding tissues.5. Ensure regular pressure ulcer dressings to avoid any type of infection and effective wound healing.
Read Also: What Medicine Is Good For Ulcers