What Is Ulcerative Colitis
- Ulcerative colitis is a form of inflammatory bowel disease, or IBD that affects the large intestine.
- In a person with UC, the lining of the colon becomes inflamed and swollen.
- Symptoms:
Management Of Moderate To Severe Ulcerative Colitis
- Gastroenterology
You’ve saved your first item
You can find your saved items on your dashboard, in the “saved” tab.
You’ve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
You’ve subscribed to your first topic alert
What does that mean?
How Do You Get Diagnosed With Ulcerative Colitis
Common tests used in patients with UC are:
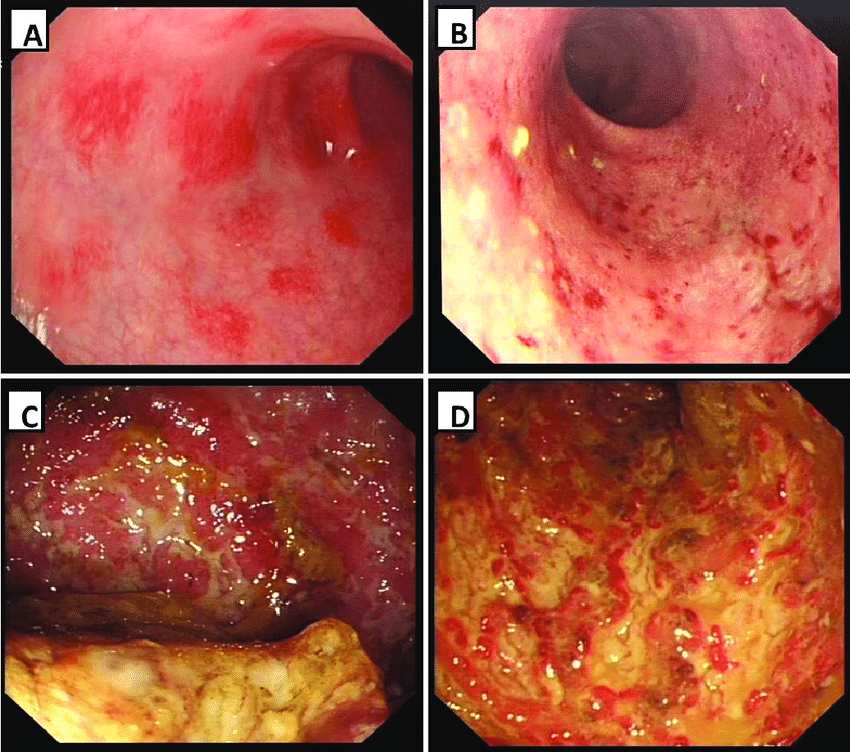
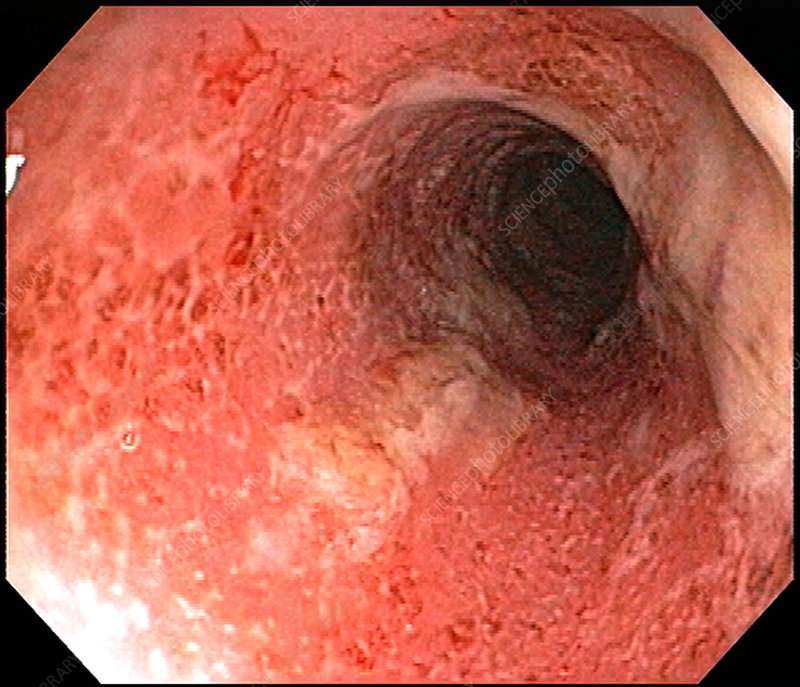
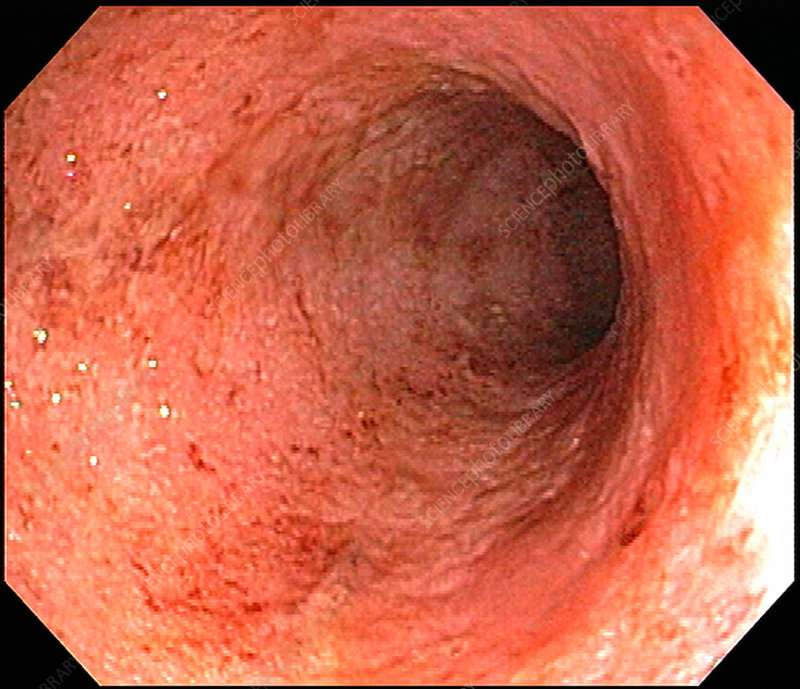
- Colonoscopy: this is the test used most commonly to make the initial diagnosis of UC and later for ongoing monitoring of disease severity.
- Routine blood tests: detect infection, anemia, inflammation and vitamin deficiencies.
- Fecal blood test: detects blood in your stool and bleeding in the intestines.
- Other stool tests: detect infection and monitor disease severity.
- Computerized tomography : shows different images of the bowels and surrounding tissue.
Read Also: Treating Hindgut Ulcers In Horses
Cyclosporine For Refractory Acute Severe Uc
Patients with fulminant UC who have not responded to high-dose IV steroids for 57 days may respond to IV cyclosporine.,, IV cyclosporine has been demonstrated to induce response or remission in 6482% of patients ,, however, up to 50% of patients ultimately undergo a colectomy. Because long-term cyclosporine is not effective for maintenance of remission, bridge therapy to 6-MP or azathioprine is necessary. Concurrent use of 6-MP or azathioprine as a bridge therapy with cyclosporine may decrease the release rate in those individuals who initially respond to cyclosporine to as low as 10%. Potential side effects associated with cyclosporine include severe, opportunistic infections , nephrotoxicity, hypertension, seizures, peripheral neuropathy, and anaphylaxis.,,
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with inflammatory bowel disease and their loved ones. On MyCrohnsAndColitisTeam, more than 148,000 members come together to ask questions, give advice, and share their stories with others who understand life with Crohns disease and ulcerative colitis.
Are you living with Crohns disease or ulcerative colitis? How was your diagnostic process? Share your experience in the comments below, or start a conversation by posting on your Activities page.
You May Like: Remicade Infusion For Ulcerative Colitis
Diagnosing Colitis And Chronic Ulcerative Colitis
Your gastroenterologist may suspect colitis based on your medical history and a review of your symptoms. He or she will have you undergo a colonoscopy procedure using a colonoscope to view the colon and rectum, and may take a tissue sample to help determine the cause. Other tests and procedures include:
- BLOOD TESTSBlood tests are taken to determine both red and white blood cell counts. A low red blood cell count can indicate anemia, from bleeding within the colon and rectum. Elevated white blood cells, which fight infection, indicate inflammation within the colon and rectum.
- STOOL SAMPLEA stool sample may be taken to rule out a parasitic infection that can cause colitis.
- CT SCANIn addition to a colonoscopy, a CT scan can determine what areas of the rectum and colon are inflamed.
Classification of chronic ulcerative colitis
Gastroenterologists categorize chronic ulcerative colitis based on the location and extent of inflammation within the colon and rectum. For most patients, the affected area remains the same during the course of the disease.
Managing Ulcerative Colitis With Diet
Dietary changes are among the best ways to control ulcerative colitis. The food you eat can affect the tissue inside your digestive system and trigger inflammation. Avoid trigger foods and replace them with foods that are easier to digest to reduce the chances of a flare-up.
Foods that are less likely to trigger ulcerative colitis symptoms
Foods that are generally easily tolerated include:
- Lean protein .
- Refined grains .
- Cooked vegetables if they are skinless and seedless.
- Calcium-rich foods such as yogurt, collard greens, certain dairy products.
- Food with probiotics such as kimchi, miso, and sauerkraut.
Foods more like to trigger ulcerative colitis symptoms
Foods that are more likely to cause a flare-up of symptoms include:
- Insoluble fiber .
- Lactose .
Read Also: Ulcerative Colitis Social Security Disability
Assessing Ulcerative Colitis Disease Severity
Multiple factors are used to assess disease severity in UC, including the frequency of bowel movements, the extent of rectal bleeding, the endoscopic appearance, and the effects of the condition on a patients quality of life and day-to-day activities. Mild disease, which is typically considered to be fewer than 5 bowel movements per day, does not negatively affect daily life, as patients are able to adapt to the bowel frequency. Moderate to severe disease is characterized by more frequent bowel movementsup to 10 per daywith bleeding. This degree of severity may interfere with patients attendance at work or school.
Clinical trials in UC have classically used the Mayo Score, which is based on the frequency of bowel movements, the number of bowel movements with blood, and an overall assessment of how the symptoms impact daily activities . There is not one simple method of evaluating a patients disease severity. One patient may develop proctitis that is severe and disabling, whereas another patient may have extensive colitis that is mild and has a limited effect on daily activities. There can also be disparities between a patients symptoms and the endoscopic appearance. There are patients with mild endoscopic disease who have severe symptoms, and there are patients with more severe colonic inflammation who have no quality-of-life impairments.
Assessing Severity Of Disease In Patients With Ulcerative Colitis
Ulcerative colitis is a chronic disease that can present at various stages of disease activity and severity. Traditionally, severity scoring has focused on disease activity during a single moment with various tools, including patient-reported symptoms, as well as clinical, laboratory-based, endoscopic, histologic, and imaging variables. Optimal delivery of care depends on the accurate assessment of disease severity, which must take longitudinal variables into account. This article reviews the history of severity scoring in UC and provides a concise, clinically oriented approach to assessing disease severity.
Keywords: Clostridium difficile
Recommended Reading: How To Use Aloe Vera Gel For Ulcerative Colitis
You And Your Care Team Are In Control
While there is no cure for UCwhile also knowing it can progress and symptoms can get worse over timeits important to remember that you and your doctor can get your disease under control. Recognizing the signs early and getting treatment right away is key. Thats why having open conversations with your doctor and being prepared for every appointment is crucial to managing your UC.
Speak openly with your doctor about how much your UC is truly impacting you. Make a personal action plan to see how much of your time your disease is affecting and get customized steps to help you and your doctor get control of your disease.
Some Doctors May Use The Following Table To Classify Your Symptoms*:
*A patient does not need to have all of these factors to be considered in a specific category of disease
Ulcerative colitis symptoms are considered moderate when you experience between 4-6 stools per day which include a moderate amount of blood. Severe UC is when you experience 6-10 per day with a severe amount of blood when passing.
If youre concerned about any of your symptoms, talk to your doctor immediately.
You May Like: Can Stress Cause Flare Up Ulcerative Colitis
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
New Guideline Provides Recommendations For The Treatment Of Mild
Bethesda, MD Most patients with ulcerative colitis have mild-to-moderate disease characterized by periods of activity or remission, but practice variations exist in disease management. A new clinical guideline from the American Gastroenterological Association published in Gastroenterology, the official journal of AGA, addresses the medical management of these patients, focusing on use of both oral and topical 5-aminosalicylates medications, rectal corticosteroids and oral budesonide, to promote high-quality care for UC patients.
AGAs new clinical guideline is meant to help with the management of patients with mild-to-moderate UC, but not all patients will effectively respond to the outlined therapies. In those cases, there may be a need to escalate treatment to systemic corticosteroids, immunomodulators and/or biologic therapies for induction and maintenance of remission. However, the use of biologic therapies and/or immunomodulators are not specifically addressed within the guideline.
The guideline recommends the following for the medical management of mild-to-moderate ulcerative colitis: 1. Use either standard dose mesalamine or diazo-bonded 5-ASA rather than low dose mesalamine, sulfasalazine or no treatment in patients with extensive mild-moderate UC.
2. In patients with extensive or left-sided mild-moderate UC, add rectal mesalamine to oral 5-ASA.
11. In patients with mildmoderate UC , AGA makes no recommendation for use of probiotics.
Also Check: Natural Supplements For Ulcerative Colitis
Ulcerative Colitis Vs Crohns Disease Vs Irritable Bowel
Other gut diseases can have some of the same symptoms.
- Ulcerative colitis affects only your large intestine and its lining.
- Crohnâs disease causes inflammation, but it affects other places in your digestive tract.
- Irritable bowel syndrome has some of the same symptoms as UC, but it doesnât cause inflammation or ulcers. Instead, itâs a problem with the muscles in your intestines.
How Can You Use This Information
You dont need to become an expert in the tools your doctor uses to determine the severity of your condition. However, it is helpful to understand how this information is used.
Determining severity helps your doctor know how to best treat your IBD. Following changes in severity over time helps you and your doctor know if treatments are working.
There are two separate goals of treatment: improving your symptoms and healing your bowels. While the two usually go hand in hand, your health care provider may see improvement in your bowels before you experience an improvement of your symptoms, or vice versa. If youre not seeing improvement in symptoms or in your bowels, it may be time to discuss different treatment options.
It is important to discuss your treatment goals with your doctor, so you can work together to meet those goals.
Don’t Miss: I Think I Have Ulcerative Colitis
What Are The Treatment Options
Ulcerative colitis treatments fall into two categories: medication to reduce inflammation and promote healing, and medication to manage symptoms. Surgery may also be necessary in some cases.
5-Aminosalicylates
5-aminosalicylates are the most common medicines for treating ulcerative colitis. They include drugs like mesalamine and sulfasalazine. Patients can use these medications orally or as a suppository or enema, depending on the severity of their symptoms. These drugs are anti-inflammatory and are usually taken long-term to maintain remission and prevent flare-ups. Side effects that can be present:
- Headaches
- Insomnia
Immunosuppressants
Immunosuppressants reduce inflammation by dampening the immune response. Therefore, they can increase the risk of infections and are generally prescribed when other treatments have not worked. Other side effects vary depending on the drug, but anemia is a common issue and patients on immunosuppressants should have regular blood tests. They are usually given by injection.
Painkillers
Patients can manage symptoms like abdominal pain by taking acetaminophen. People with ulcerative colitis should not take non-steroidal, anti-inflammatory drugs like aspirin, ibuprofen, naproxen, or diclofenac, as they can exacerbate symptoms.
Anti-Diarrhea Medication
Patients with severe diarrhea can take anti-diarrhea drugs, such as loperamide, to manage this symptom.
Antibiotics
Surgery
How Does Your Doctor Determine Severity
To determine the severity, or disease activity, of a persons IBD, doctors look at a number of different measures. These include patient-reported outcomes, which is the information you tell your doctor about your symptoms. Other ways to measure disease severity include lab tests, endoscopic evaluation , and imaging studies.
Patient-reported outcomes are symptoms reported by individuals with Crohns disease or ulcerative colitis, sometimes through questionnaires. Your doctor might want to know the number and quality of your bowel movements, whether there is blood in your stool , if you have abdominal pain or have lost weight, whether you can perform daily activities, and if you have any complications related to IBD.
| Are you living with Crohns disease or ulcerative colitis?How was your diagnostic process?Click in the comments below. |
Physical exams help doctors assess severity by measuring vital signs, such as body temperature and heart rate, as well as feeling for abdominal tenderness and abdominal masses.
Laboratory tests include fecal calprotectin and blood tests for hemoglobin, albumin levels, and markers of inflammation, such as erythrocyte sedimentation rate and C-reactive protein levels. Imaging studies can include X-rays, computed tomography , magnetic resonance imaging , and ultrasound of the abdomen.
Don’t Miss: How Do You Treat A Peptic Ulcer
What Are Ulcerative Colitis Causes And Risk Factors
The cause of ulcerative colitis is not known, but it is thought to involve an abnormal activation of the immune system in the intestines that results in chronic inflammation and ulcers in parts of the large intestine.
Having a first-degree relative who has ulcerative colitis is a risk factor for developing ulcerative colitis. The susceptibility to abnormal activation of the immune system is genetically inherited.
Role Of Rectal Therapy
When considering the various treatment modalities for UC, it is important to recognize that the rectum requires separate treatment. Patients receiving a biologic agent or mesalamine may require a second agent to address rectal symptoms such as tenesmus, urgency, or worsening continence. Although such rectal symptoms may qualify as mild to moderate by standard definitions, they are often considered severe by patients living with the condition. For example, incontinence can be embarrassing and difficult to manage.
The decision to use rectally administered therapy is guided by the proximal extent of disease and by patient preference. There are clear advantages to rectal delivery over oral therapy in some circumstances. It has long been recognized that left-sided disease and extensive disease have improved responses when topical therapy is added to the existing oral mesalamine regimen., Topical mesalamine has been advocated as preferable to oral therapy in patients with proctitis/proctosigmoiditis and left-sided UC because it provides sufficient concentrations of active drug at the inflamed site. Moreover, systemic absorption is considerably low given that the therapeutic efficacy of mesalamine is topical in nature. Other advantages include a generally faster response and a less frequent dosing regimen.
You May Like: Causes Of Bleeding Ulcers In Stomach
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Drugs That Target Inflammation
Most people with UC take prescription drugs called aminosalicylates that tame inflammation in the gut. These include balsalazide , mesalamine , olsalazine , and sulfasalazine . Which one you take, and whether it is taken by mouth or as an enema or suppository, depend on the area of your colon that’s affected. As long as you avoid your triggers, these may be enough if your disease is mild to moderate.
You may need something else if your condition is more severe or if those standard treatments stop working. Your doctor may consider other medicines. Some people may also need surgery.
Don’t Miss: How Do You Know If You Have Ulcerative Colitis
Spicing Up The Treatment Of Mild To Moderate Ulcerative Colitis
- Charles N. BernsteinAffiliationsUniversity of Manitoba IBD Clinical and Research Centre, Department of Internal Medicine, College of Medicine, Faculty of Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada
N Engl J Med.
- Hommes D.W.
- et al.
Gut.Gastroenterology.N Engl J Med.
Gut.
- Moro L.
- et al.
Gastroenterology.
Gut.
- Moro L.
- et al.
Gastroenterology.
Ann Intern Med.Gut.Am J Gastroenterol.Ann Intern Med.
- Middleton S.
- et al.
Gastroenterology.N Engl J Med.
Am J Gastroenterol.
- Graff L.A.
- et al.
Gut.
Clinical Gastroenterology and HepatologyClin Gastroenterol Hepatol.
- Wu J.C.Y.
- et al.
Clin Gastroenterol Hepatol.
Clin Gastroenterol Hepatol.Gastroenterology.
- Feagan B.J.
- et al.
Gastroenterology.