Pressure Ulcers And Mortality
Pressure ulcers have been associated with increased mortality rates in both acute and long-term care settings. Death has been reported to occur during acute hospitalization in 67% of patients who develop a pressure ulcer compared with 15% of at-risk patients without pressure ulcers . Patients who develop a new pressure ulcer within 6 weeks after hospitalization are three times as likely to die as patients not developing a pressure ulcer . In long-term care settings, development of a pressure ulcer within 3 months among newly admitted patients was associated with a 92% mortality rate, compared with a mortality rate of 4% among residents who did not subsequently develop a pressure ulcer . Residents in a skilled nursing facility who had pressure ulcers experienced a 6-month mortality rate of 77.3%, whereas patients without pressure ulcers had a mortality rate of 18.3% . Patients whose pressure ulcers healed within 6 months had a significantly lower mortality rate than patients whose pressure ulcers did not heal .
Treatment For Pressure Sores
There are a variety of treatments available to manage pressure sores and promote healing, depending on the severity of the pressure sore. These include:
- regular position changes
- special mattresses and beds that reduce pressure
- being aware of the importance of maintaining healthy diet and nutrition
- dressings to keep the sore moist and the surrounding skin dry. There is no advantage of one type of dressing over another.
- saline gauze dressing may be used if ointments or other dressings are unavailable.
- light packing of any empty skin spaces with dressings to help prevent infection
- regular cleaning with appropriate solutions, depending on the stage of the sore
- there is no advantage of one particular type of antiseptic or antibiotic treatment over another
- specific drugs and chemicals applied to the area, if an infection persists
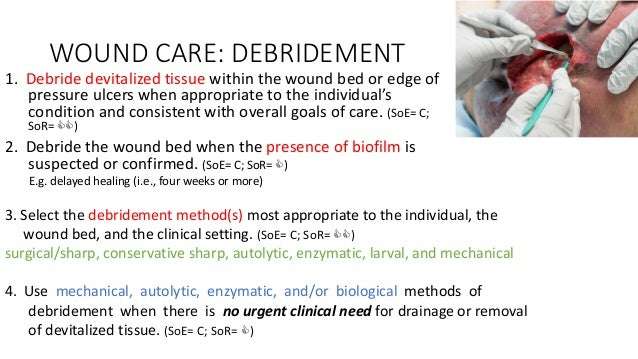
- surgery to remove the damaged tissue that involves thorough debridement of the wound, the removal of underlying or exposed bone, and filling the empty space
- operations to close the wound, using skin grafts if necessary
- continuing supportive lifestyle habits such as eating a healthy and nutritious diet, as suggested by the nutritional staff.
Key Points About Bed Sores
- Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period.
- Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile.
- Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas.
You May Like: Ulcerative Colitis And Lung Disease
Topical Dressings And Local Wound Care
Local wound treatment is directed to providing an optimum wound environment and improving host factors. The most commonly used dressing for pressure ulcers at hospital discharge in the United States is dry gauze . The use of dry gauze persists despite clear data suggesting that it results in delayed healing . Compared with wet-to-dry gauze dressings, moist dressings are clearly superior. Moist wound healing allows experimentally induced wounds to resurface up to 40% faster than air-exposed wounds .
Occlusive dressings have been developed to produce a moist wound environment. The term âocclusiveâ describes the lessened ability of a dressing to transmit moisture vapor from a wound to the external atmosphere. The degree to which dressings dry the wound can be measured by the moisture vapor transmission rate . A MVTR of less than 35 g of water vapor per square meter per hour is required to maintain a moist wound environment. Woven gauze has an MVTR of 68 g/m2/h, and impregnated gauze has an MVTR of 57 g/m2/h. In comparison, hydrocolloid dressings have an MVTR of 8 g/m2/h . Any therapy that dehydrates the wound, such as dry gauze, heat lamps, air exposure, or liquid antacids, is detrimental to the healing of chronic wounds .
The International Guideline Qrg App
|
Announcing the Official Mobile App of the EPUAP, NPIAP, and PPPIA – 2019 International Pressure Ulcer/Injury Guideline! You’re invited to the launch of our exciting new app! We’ve taken the years of time and dedication poured into the International Guideline, and turned it into a useful Mobile App. This beautiful app places all of the Quick Reference Guideline content at your fingertips today… Find out more now! |
Recommended Reading: Besivance Dosage For Corneal Ulcer
General Statement On Use Of 2019 Guideline Content
“The use of EPUAP/NPIAP/PPPIA material does not imply endorsement of products or programs associated with the use of the material.”
Assessment Of Those With Pressure Ulcers
In patients presenting with pressure ulcers the ulcer is documented using photographic evidence. Patients general health and nutritional status is assessed.
Mobility, previous pressure damage, level of consciousness, psychological factors etc. are also assessed.
The patient undergoes a routine blood test to detect infections, high blood sugar , high blood cholesterol) and sometimes blood cultures to determine presence of infections.
Blood cultures are prescribed if there are signs of severe blood poisoning like fever, elevated white blood cell count, rigors, sweating and delirium.
Nutritional assessment is made by testing for serum albumin and haemoglobin . A routine chest X ray is performed before any surgical treatment is chosen.
Recommended Reading: What Foods Should You Avoid When You Have An Ulcer
Small Cell Technology In Alternating Pressure Mattresses
The International Guideline Development Group has reviewed the evidence on small cell technology in alternating pressure mattresses. The recommendation to avoid using small cell alternating pressure mattresses and overlays has been retracted by the guideline development team.
In one older study pressure ulcers occurred more frequently in individuals who received a small cell mattress compared with a large cell mattress . However, both the mattresses trialled in this study used technology and materials that are outdated and the results cannot be extrapolated to contemporary technologies.
When selecting a mattress or overlay with alternating pressure features the choice should be individualized according to pressure ulcer risk, comfort of the individual and effectiveness determined through regular skin assessments. Clinical evaluation of an alternating pressure support surface should include assessment of the individual using the surface in supine, lateral and sitting positions, and the potential for the support surface to redistribute pressure without “bottoming out”. The individual’s body shape, size, weight distribution, and any asymmetrical bony prominences may influence the performance of an alternating pressure support surface.
References
When You Are In Bed
Use a foam mattress or one that is filled with gel or air. Place pads under your bottom to absorb wetness to help keep your skin dry.
Use a soft pillow or a piece of soft foam between parts of your body that press against each other or against your mattress.
When you are lying on your side, put a pillow or foam between your knees and ankles.
When you are lying on your back, put a pillow or foam:
- Under your heels. Or, place a pillow under your calves to lift up your heels, another way to relieve pressure on your heels.
- Under your tailbone area.
- Under your shoulders and shoulder blades.
- Under your elbows.
Other tips are:
- DO NOT put pillows under your knees. It puts pressure on your heels.
- Never drag yourself to change your position or get in or out of bed. Dragging causes skin breakdown. Get help if you need moving in bed or getting in or out of bed.
- If someone else moves you, they should lift you or use a draw sheet to move you.
- Change your position every 1 to 2 hours to keep the pressure off any one spot.
- Sheets and clothing should be dry and smooth, with no wrinkles.
- Remove any objects such as pins, pencils or pens, or coins from your bed.
- DO NOT raise the head of your bed to more than a 30 degree angle. Being flatter keeps your body from sliding down. Sliding may harm your skin.
- Check your skin often for any areas of skin breakdown.
You May Like: Compression Therapy For Venous Leg Ulcers
Guideline Launch: Los Angeles 15
The GGG are proud to announce the upcoming publication of the third edition ofthe Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline.We are please to invite you to a special launch event with atwo-day program focused on pressure injuries:
- USC Hotel and University of Southern California Campus
- 15-16 November 2019
Treatment At Wound Site
Once a pressure ulcer has begun to develop, reducing the pressure on that area is critical to improving the condition. Some patients may be unable to avoid resting on certain parts of their body. They may also be unaware when they shift into a position that worsens a pressure ulcer. Bone protrusions on particularly thin patients can also be difficult to work around. Cullum, Mcinnes, Bell-Syer, and Legood, discuss the advantages of padded support surfaces for patients who are unable to keep weight of a certain part of the body. The softer surface reduces the pressure in the area and stops the tissue from becoming ischemic. This tool can work as a preventative measure as well, but is a vital tool in reducing the effects of a pressure ulcer once it has developed for patients who struggle with resting in different positions.
Standard treatments at the sight of injury for such wounds should also be administered. Bandaging can help reduce additional damage caused by friction of the wound against surfaces such as clothes and bedding. Topical ointments or antiseptics may be used as prescribed by the patients physician to manage the healing process and prevent against infection. In particularly severe pressure ulcers, surgery may be necessary to remove necrotic tissue and promote healthy tissue to regrow in the area .
You May Like: Natural Supplements For Ulcerative Colitis
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
Pressure Ulcers: Prevention And Management
Clinical guideline
This guideline covers risk assessment, prevention and treatment in children, young people and adults at risk of, or who have, a pressure ulcer . It aims to reduce the number of pressure ulcers in people admitted to secondary or tertiary care or receiving NHS care in other settings, such as primary and community care and emergency departments.
You May Like: Diabetic Foot Ulcer Treatment Guidelines
Nutrition In The Treatment Of Pressure Ulcers
One of the most important potentially reversible host factors contributing to wound healing is nutritional status. Several studies suggest that dietary intake, especially of protein, is important in healing pressure ulcers . Greater healing of pressure ulcers has been reported with a higher protein intake irrespective of positive nitrogen balance . Breslow evaluated 48 patients with Stage II through Stage IV pressure ulcers in a dietary intervention trial. Undernutrition was defined as a serum albumin below 35 g/l or body weight more than 10% below the midpoint of the age-specific weight range. The results suggested that patients fed a 24% protein diet healed their pressure ulcers at a greater rate than those fed a standard 14% protein diet. However, changes in body weight or in biochemical parameters of nutritional status did not occur between groups. The study was limited by a small sample size , nonrandom assignment to treatment groups, confounding effects of air-fluidized beds, and the use of two different feeding routes .
An optimum dietary protein intake in patients with pressure ulcers is unknown but may be much higher than current adult recommendations of 0.8 g/kg/d. Half of the chronically ill elderly persons are unable to maintain nitrogen balance at this level . Increasing protein intake beyond 1.5 g/kg/d may not increase protein synthesis and may cause dehydration . A reasonable protein requirement is therefore between 1.2 and 1.5 g/kg/d.
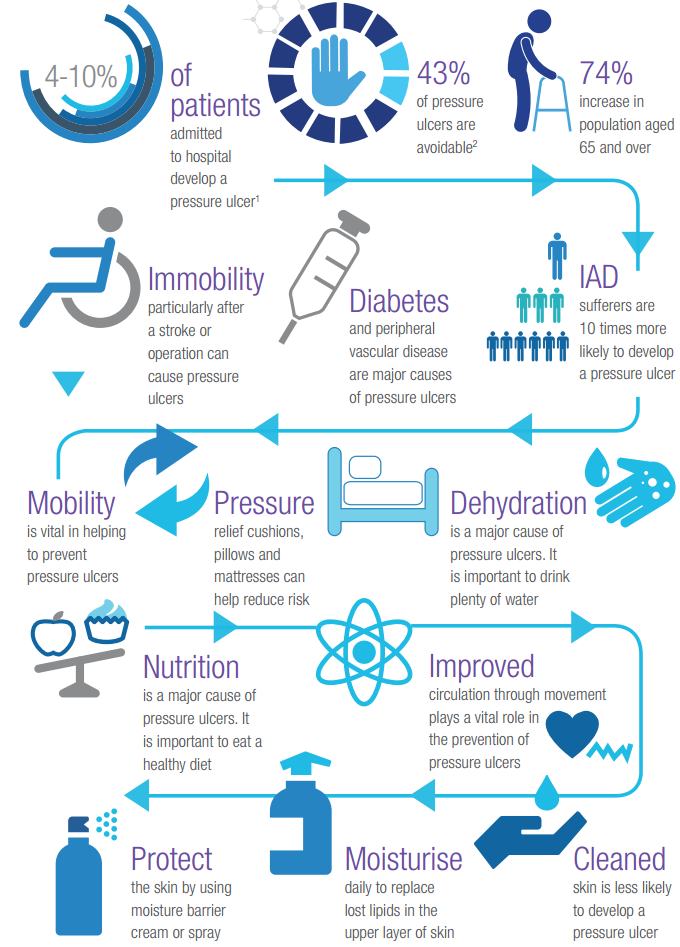
Risk Factors For Pressure Sores
A pressure sore is caused by constant pressure applied to the skin over a period of time. The skin of older people tends to be thinner and more delicate, which means an older person has an increased risk of developing a pressure sore during a prolonged stay in bed.
Other risk factors for pressure sores include:
- immobility and paralysis for example due to a stroke or a severe head injury
- being restricted to either sitting or lying down
- impaired sensation or impaired ability to respond to pain or discomfort. For example, people with diabetes who experience nerve damage are at increased risk of pressure sores
- urinary and faecal incontinence skin exposed to urine or faeces is more susceptible to irritation and damage
- malnutrition can lead to skin thinning and poor blood supply, meaning that skin is more fragile
- obesity being overweight in combination with, for example, immobility or being restricted to sitting or lying down can place extra pressure on capillaries. This then reduces blood flow to the skin
- circulation disorders leading to reduced blood flow to the skin in some areas
- smoking reduces blood flow to the skin and, in combination with reduced mobility, can lead to pressure sores. The healing of pressure sores is also a slower process for people who smoke.
If youre bedridden, pressure sores can occur in a number of areas, including:
- back or sides of the head
- rims of the ears
- backs or sides of the knees
- heels, ankles and toes.
Recommended Reading: How To Heal Ulcerative Colitis With Food
Position Changes To Prevent Pressure Sores
If you use a wheelchair shift position within your chair about every 15 minutes. If you spend most of their time in bed change position at least once every two hours, even during the night and avoid lying directly on your hipbones.
Pillows may be used as soft buffers between your skin and the bed or chair. The head-of-bed elevation should be maintained at/or below 30 degrees. Or depending on the your medical condition, the bed should at least be elevated to the lowest degree to prevent injury. When lying on your side, a 30 degrees position should be used.
Evaluation Of Type Of Discharge And Pus
Amount and type of discharge and pus is noted. This is assessed along with signs of infection.
A swap is used to take a sample of the pus or exudate and this is placed on a glass slide. This is evaluated after staining with appropriate dyes and examining under the microscope for presence of microorganisms.
The samples of the exudate is also used for culture in the laboratory and assessment of sensitivity to various antibiotics that may be used in therapy.
Presence of a track of pus or fistula or sinus is noted. This is usually a recurrent and bothersome condition that is difficult to treat without surgery.
Recommended Reading: What Foods Are Good For Ulcers And Gastritis
What Are The Risk Factors For Bedsores
Being bedridden, unconscious, unable to sense pain, or immobile increases the risk that a bedsore will develop. The risk increases if the person is not turned, positioned correctly, or provided with proper nutrition and skin care. People with diabetes, circulation problems and malnutrition are at higher risk.
Daily Skin Care To Prevent Pressure Sores
Ways to prevent pressure injuries include:
- Checking the skin at least daily for redness or signs of discolouration.
- Keeping the skin at the right moisture level, as damage is more likely to occur if skin is either too dry or too moist.
- Using moisturising products to keep skin supple and prevent dryness.
- Never massaging bony areas because the skin is too delicate.
Recommended Reading: How Do They Check For Ulcers
Ecri Guidelines Trust Acceptance Of 2019 Pressure Ulcer/injury Guideline
3 November 2020
The Guideline Governance Group is pleased to announce that the 2019 International Pressure Ulcer/Injury Guideline has been reviewed and accepted by the ECRI Guidelines Trust ®. The ECRI summaries of the International Guideline are available at these links after regsitering at the ECRI Guidelines Trust ® website .
Acceptance on the ECRI Guidelines Trust ® website serves as validation of the high quality of the 2019 International Pressure Ulcer/Injury Guideline. The ECRI Guidelines Trust ® website allows clinicians to compare this guideline with other similar guidelines. Because the ECRI Guidelines Trust ® website only contains a summary of posted guidelines, we recommend that those interested in implementing pressure ulcer/injury prevention and treatment guidelines access thefree QRG and consider purchasing the full CPG available at the guideline shop.