Risk Of Bias Assessment
Assessments of the risk of bias of the included studies are shown in Figure 8. In the observational studies, the representativeness of the exposed and the selection of the non-exposed cohort was judged to be at high risk in multiple studies . In the studies of Daperno, Protic, and Radojcic, no comparison was performed between groups regarding age, sex, and extent of disease .
Figure 8. Risk of bias in RCTs and in non-randomized studies.
Among the RCTs, the studies of Williams and Laharie carried the lowest risk of bias . As they were open trials, participants and personnel were not blinded however, in the study of Williams, outcome assessment remained blinded. Because the study of Scimeca et al., was only published in a conference abstract form, almost all domains were judged as carrying unclear risk of bias .
Clinical And Endoscopic Response
Three months after surgery, five patients failed the study due to the requirement of colectomy or trial medication . In the remaining 25 patients, the post-operative Mayo score was significantly decreased when compared with baseline . Clinical response was observed in 16 patients, of whom 7 were in endoscopic remission. Little or no change in symptoms was seen in 9 patients. During follow up, gradual weaning of medication was performed, according to the decision of the MDT.
Twelve months after appendectomy, an additional 6 patients had failed . Of the remaining 18 patients, 12 showed clinical response at this time point 5 of these 12 were in endoscopic remission . None of the patients were using steroids at this time point.
Flow chart of clinical response after appendectomy.
Perforation Of The Colon
Chronic inflammation caused by ulcerative colitis can weaken the wall of the colon until a hole, or perforation, develops. Once the colon has been perforated, the contents of the intestine can spill into the abdomen and cause a serious infection called peritonitis.
This is a potentially life-threatening condition that needs immediate medical treatment.
Read Also: How To Cure Tongue Ulcer
Little Girl Visited By Gary Neville At Children’s Hospital Ends Up Working For Footy Legend 15 Years Lateryour Browser Indicates If You’ve Visited This Link
A woman who was visited in hospital by Gary Neville 15 years ago has shared the inspirational story of how she now works alongside the football legend. Jenny Byrne, 21, from Stockport, was rushed into hospital at the age of six and was later diagnosed with Ulcerative Colitis – an inflammatory bowel disease.
Manchester Evening News on MSN.com
Ulcerative Colitis Surgical Procedures
The standard surgical procedure to treat ulcerative colitis is a proctocolectomy. This surgery removes both your colon and your rectum .
There are two types of proctocolectomy procedures used to treat ulcerative colitis.
-
Proctocolectomy with ileal pouch-anal anastomosis: Removal of the colon and rectum, and creation of an internal pouch that eliminates the need for a permanent external ostomy.
-
Proctocolectomy with end ileostomy: Removal of the colon, recturm, and anus and creation of an external ostomy.
It can feel overwhelming when you are recommended for one of these surgeries. We can help you understand whats involved with each surgery, and be prepared for life after your proctocolectomy.
Don’t Miss: Ulcerative Colitis Surgery Pros And Cons
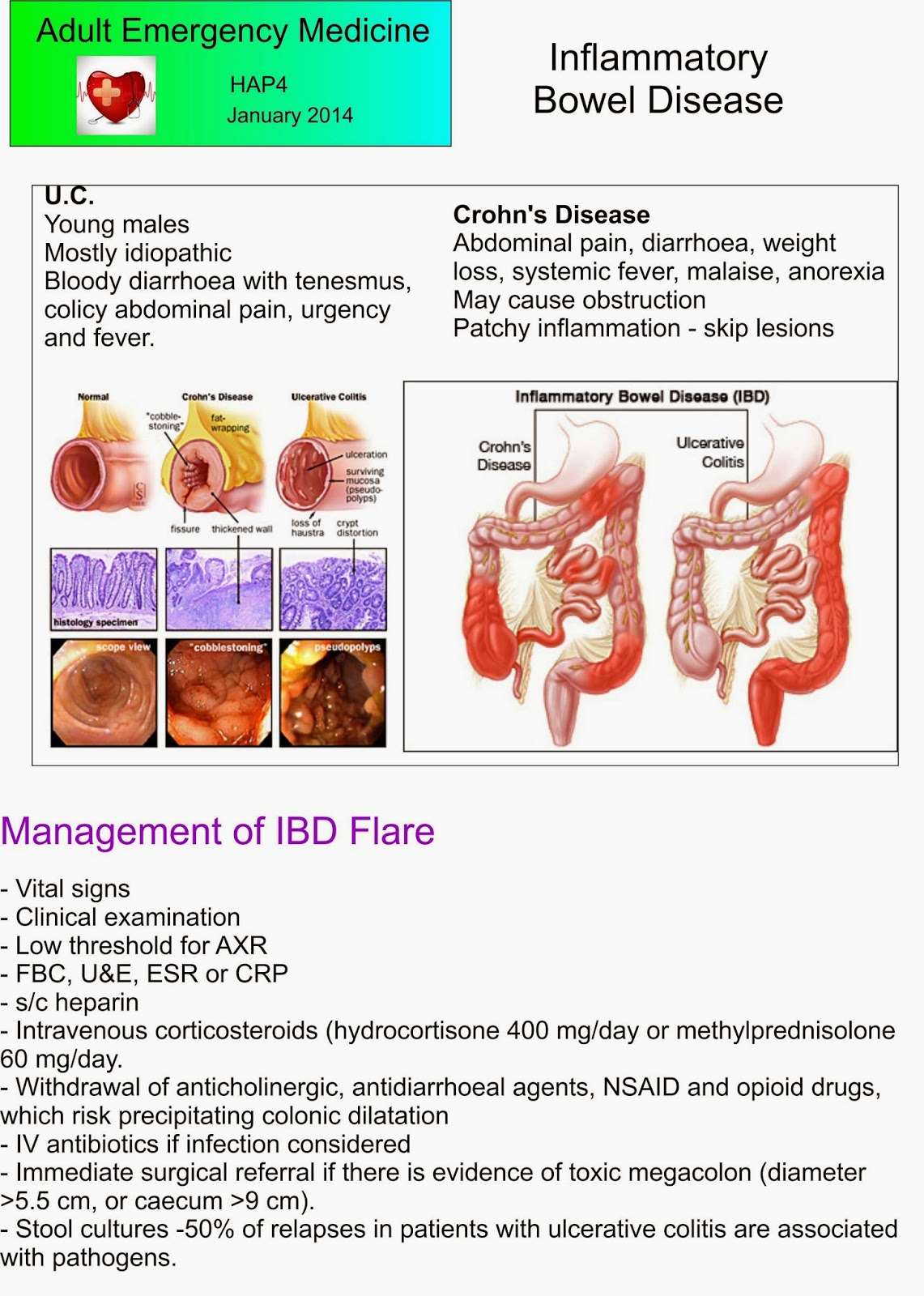
Management Of Ulcerative Colitis
Management of ulcerative colitis involves first treating the acute symptoms of the disease, then maintaining remission. Ulcerative colitis is a form of colitis, a disease of the intestine, specifically the large intestine or colon, that includes characteristic ulcers, or open sores, in the colon. The main symptom of active disease is usually diarrhea mixed with blood, of gradual onset which often leads to anaemia. Ulcerative colitis is, however, a systemic disease that affects many parts of the body outside the intestine.
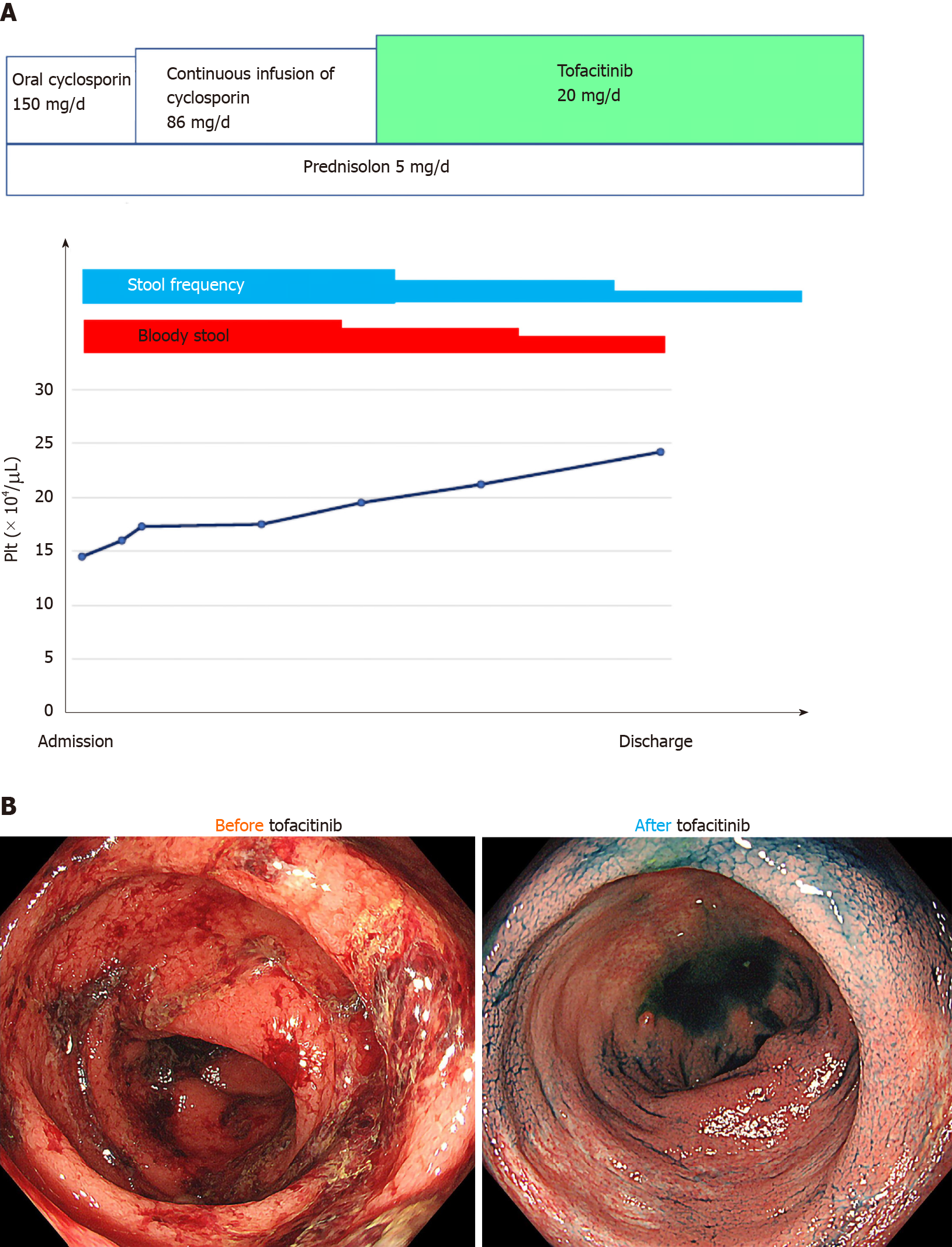
Cyclosporine For Refractory Acute Severe Uc
Patients with fulminant UC who have not responded to high-dose IV steroids for 57 days may respond to IV cyclosporine.,, IV cyclosporine has been demonstrated to induce response or remission in 6482% of patients ,, however, up to 50% of patients ultimately undergo a colectomy. Because long-term cyclosporine is not effective for maintenance of remission, bridge therapy to 6-MP or azathioprine is necessary. Concurrent use of 6-MP or azathioprine as a bridge therapy with cyclosporine may decrease the release rate in those individuals who initially respond to cyclosporine to as low as 10%. Potential side effects associated with cyclosporine include severe, opportunistic infections , nephrotoxicity, hypertension, seizures, peripheral neuropathy, and anaphylaxis.,,
Also Check: What To Drink With Stomach Ulcer
Infliximab For Refractory Moderate
Infliximab was initially demonstrated to be effective for UC in preliminary studies. In the definitive multicenter clinical Active Ulcerative Colitis Trials 1 and 2 , patients who received infliximab at Weeks 0, 2, and 6 had a 6169% clinical response rate after 8 weeks compared with a placebo clinical response rate of 2937%. At Week 54, the clinical response rates were 4445% with infliximab compared to a 20% pla cebo response, whereas at Week 54 the infliximab clinical remission rates were 3435% compared to a 17% placebo response. Infliximab was also found to decrease steroid use and induce mucosal healing. For maintenance of remission, infliximab is continued long-term, using progressive decreases in infusion intervals and increases in dose as needed. Thus, infliximab is an appropriate therapeutic approach for moderate-to-severe UC patients who are refractory to other therapies .
Living With An Ileostomy
You can live a long, active, and productive life with an ileostomy. In many cases, ileostomy patients can participate in the same activities they did before the surgery, including sports, outdoor activities, swimming and other watersports, travel, and work.
Whether your ileostomy is permanent or temporary, it is common for patients to initially feel self-conscious about their ostomy and you may notice a change in how you feel about your body image. Some patients prefer to limit how visible the bag is to others. The ostomy bag typically lays fairly flat under your clothing.
Remember, it is just as important to take care of your mental and emotional health as it is your physical health. Speak with your doctor or a mental health professional if you feel you are experiencing symptoms of depression or anxiety.
-
There are several pouching systems for you to choose from. You will learn how to use your system as well as how to care for the skin surrounding the stoma.
-
Talk to your doctor about any specific dietary restrictions with an ileostomy. It is important for you to drink plenty of fluids to avoid dehydration and loss of electrolytes.
-
Eating foods high in pectin, including applesauce, bananas, and peanut butter, will help thicken your stool output and control diarrhea. Discuss this with your doctor.
The United Ostomy Associations of America has additional resources as you learn to live with your ostomy.
Read Also: Is Alcohol Bad For Ulcerative Colitis
Data Collection And Analysis
Patient demographics along with their clinical, haematological, biochemical and radiological profiles and disease characteristics were recorded prospectively on a dedicated database in addition to operative and postoperative details. Access equipment and length of stay costs were determined by the directorate business manager. Postoperative classifications were categorized as by Clavien-Dindo. Unless otherwise stated, data is represented as median and n represents the number of patients included in the analysis. Differences in categorical variables were evaluated using a Pearson’s chi-squared test and differences in continuous variables were evaluated using MannWhitney U and Students t-testing where appropriate . All calculations were done using SPSS version 12.0 .
What To Expect After Your Surgery
Most people do very well after their surgery and are able to return to work and their normal daily activities after they recover.
-
You should expect an adjustment period of up to one year to get used to the changes in your body after your proctocolectomy.
-
You will likely be on liquid or soft food diet for the first few days after surgery. Your doctor will then have you slowly introduce bland solid foods. You should chew your food thoroughly and avoid any foods that may cause gas, diarrhea or anal irritation. Its also important to drink plenty of water. We recommend six to eight glasses a day.
-
Some patients may still feel as if they need to have a bowel movement after their surgery, just as people who have lost a limb sometimes still feel as if the limb is still there. This called phantomrectum and it completely normal. It does not require any treatment and often subsides over time.
-
Your doctor may recommend a physical activity restriction for a minimum of six weeks, depending on what type of surgery you had.
-
Talk to your doctor about resuming normal sexual activity after your surgery. Some people find their sex life improves some time after surgery due to improvements in pain, inflammation, and other ulcerative colitis symptoms.
Don’t Miss: Does Ulcer Pain Come And Go
Complications Of Ibd As A Disability
IBD may increase the risk of a rare condition called short bowel syndrome. The Social Security Administration lists short bowel syndrome under Section 5.07 in the disability evaluation.
People may also be eligible for disability benefits if they experience unintentional weight loss due to a digestive disorder. They need to have two body mass index readings of less than 17.50, taken 60 days apart.
References And Recommended Reading
Yang A, Chen Y, Scherl E, et al.: Inflammatory bowel disease in patients with celiac disease. Inflamm Bowel Dis 2005, 11:528532.
Ardizzone S, Molteni P, Imbesi V, et al.: Azathioprine in steroid-resistant and steroid-dependent ulcerative colitis. J Clin Gastroenterol 1997, 25:330333.
Fraser AG, Orchard TR, Jewell DP: The efficacy of azathioprine for the treatment of inflammatory bowel disease: a 30 year review. Gut 2002, 50:485489. Although a retrospective review, this is one of the largest, most comprehensive studies establishing a role for the purine analogues in the induction and maintenance of remission in IBD patients.
Warman JI, Korelitz BI, Fleisher MR, Janardhanam R: Cumulative experience with short- and long-term toxicity to 6-mercaptopurine in the treatment of Crohns disease and ulcerative colitis. J Clin Gastroenterol 2003, 37:220225.
Matula S, Croog V, Itzkowitz S, et al.: Chemoprevention of colorectal neoplasia in ulcerative colitis: the effect of 6-mercaptopurine. Clin Gastroenterol Hepatol 2005, 3:10151021.
Dubinsky MC, Vasiliauskas EA, Singh H, et al.: 6-thioguanine can cause serious liver injury in inflammatory bowel disease patients. Gastroenterology 2003, 125:298303.
Cummings JR, Herrlinger KR, Travis SP, et al.: Oral methotrexate in ulcerative colitis. Aliment Pharmacol Ther 2005, 21:385389.
Read Also: Is Kimchi Good For Ulcerative Colitis
Single Port Access Device
The single port access device of preference was the Surgical Glove Port. Constructed table-side, in short, this comprises a standard surgical glove into which laparoscopic trocar sleeves are inserted without needing obturators into three fingers cut at their tips .1). The ports are tied in position using strips cut from the other glove in the pair and the cuff of the Glove port stretched onto the outer ring of a wound protector-retractor sited in the operative access wound.
Objectives And Research Question
In the treatment of steroid-refractory ASUC, two randomized controlled trials demonstrated equal short-term efficacy and safety of IFX and CYS . These results were opposed by a previous meta-analysis of observational studies, where IFX was associated with significantly higher rates of treatment response and a lower 12 months colectomy-rate compared to that with CYS . A lately reported network meta-analysis with benefit-risk analysis also suggested that there is a rank order of efficacy for colectomy-free rates favoring IFX over CYS, although the difference between the treatments was small .
Since new studies have been released and long-term survival data have become available. Therefore, we aimed to summarize the currently available evidence on the long-term efficacy and safety of IFX and CYS in steroid-refractory ASUC.
Don’t Miss: What Kind Of Yogurt Is Good For Stomach Ulcer
Colectomy And Remission In The Entire Cohort
Forty-five patients in our entire cohort underwent colectomy at a median time of 0.5 years after initiation of tacrolimus . Colectomy was performed 5.3 years after the diagnosis of UC . Eighteen colectomies were carried out within the first 3 months while under tacrolimus. Another five cases were noted before 6, five before 12 and seven before 24 months. Overall, colectomy was necessary in 35 patients within 24 months after the initiation of tacrolimus. After 24 months an additional 10 patients underwent colectomy.
Overall, clinical remission was induced in 104 of 156 tacrolimus-treated patients . Median time to remission was 0.9 months and remission was maintained for 0.9 years . Fifty out of 104 patients in remission experienced a relapse and median time to relapse was 1.0 year . Three and 6 months after the start of tacrolimus, remission was observed in 61.4 and 63.1% of patients at risk, respectively. At months 12 and 24, remission decreased to 53.8 and 39.7%.
Steroids were used in 93% of patients at baseline , in 31% after 3 months, 32% after 6 months, 18% after 12 months and 12% after 24 months.
Surgery For Ulcerative Colitis
Living with a chronic illness like ulcerative colitis often means several approaches to treatment. This can include medication, dietary modifications, nutritional supplementation, and even surgery.
While surgery can be a big source of stress and worry, it can help alleviate some of your ulcerative colitis symptoms. We can help you understand some of the most common surgical procedures used to treat ulcerative colitis, so that you can have informed discussions with your healthcare team and your loved ones.
New! Check out our video on preparing for IBD surgery:
Video Length00:2:55
Preparing for IBD surgery If you are scheduled for IBD surgery, watch this video to learn some important information and things to keep in mind as you prepare, and after surgery.
Surgery may be recommended for patients who have stopped responding to their medication or if their medication is no longer as effective as it once was. Other patients choose to undergo surgery to improve their quality of life. Some patients become dangerously ill and require emergency surgery.
Disclaimer: This information should not replace the recommendations and advice of your doctor. Surgery information is up to date at the time of publication. You should always check with your doctor for the most current information.
Video Length00:07:41
Experiences with IBD surgery These patients talk through their experiences with surgery, including how they prepared mentally prior to their procedures, and their recovery and care.
Don’t Miss: Pressure Ulcer Prevention Care Plan
Tumor Necrosis Factor Alpha Blocking Agents As Treatment For Ulcerative Colitis Intolerant Or Refractory To Conventional Medical Therapy: A Meta
- Ruxi Lv ,
Contributed equally to this work with: Ruxi Lv, Weiguang Qiao
Affiliations School of Traditional Chinese Medicine, Southern Medical University, Guangzhou, People’s Republic of China, Research Institute of Traditional Chinese Medicine, Guangdong Medical College, Zhanjiang, Guangdong, People’s Republic of China
-
Contributed equally to this work with: Ruxi Lv, Weiguang Qiao
Affiliation Department of Gastroenterology, Nanfang Hospital, Southern Medical University, Guangzhou, People’s Republic of China
-
Affiliation School of Traditional Chinese Medicine, Southern Medical University, Guangzhou, People’s Republic of China
-
Affiliation Research Institute of Traditional Chinese Medicine, Guangdong Medical College, Zhanjiang, Guangdong, People’s Republic of China
-
Affiliation Emergency Department of Nanfang Hospital, Southern Medical University, Guangzhou, People’s Republic of China
-
* E-mail:
Affiliation Research Institute of Traditional Chinese Medicine, Guangdong Medical College, Zhanjiang, Guangdong, People’s Republic of China
Ulcerative Colitis And Long
If people are unable to work for an extended period of time due to UC, they may be eligible for long-term disability insurance through their employer. A person either pays privately into an insurance program or their employer pays into a benefits program which would pay a percentage of the employees salary.
People may qualify for long-term disability insurance if they meet the policys definition of being disabled for 90180 days.
Don’t Miss: What To Eat If You Have Peptic Ulcer
Refractory Distal Ulcerative Colitis: Is Proctocolectomy Always Necessary
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Rent for 48h to view
- Buy Cloud Access for unlimited viewing via different devices
- Synchronizing in the ReadCube Cloud
- Printing and saving restrictions apply
USD 8.50
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Colectomy For Refractory Severe Uc Non

For patients with severe refractory UC that does not respond or only partially responds to medications, colectomy must be considered and discussed . Colectomy offers a number of important benefits including removal of the diseased colon with its associated risks plus avoiding potent medications and their many potential side effects. Indications for colectomy for patients with refractory severe UC include: 1) toxic megacolon, 2) severe hemorrhage, 3) fulminant colitis unresponsive to therapy, 4) refractory acute or chronic severe UC, 5) dysplasia or carcinoma, and 6) colonic stricture.
Total proctocolectomy with or without recto-anal mucosal stripping and ileoanal anastomosis IPAA is the most common surgical procedure for UC. An ileal reservoir is created in order to allow continence at the ileoanal anastomotic junction. Although some complications can occur, most patients experience excellent pouch function and quality-of-life studies have revealed superb outcomes in the majority of patients who have undergone colectomy with IPAA. Total proctocolectomy with IPAA or ileostomy are therefore important options to consider for patients with refractory severe UC who have failed medical therapy.
Recommended Reading: Foods To Avoid With Peptic Ulcer