Staging Of Pressure Injuries: Based On National Pressure Injury Staging System
Stage 1: Skin is completely intact! The area will be very red but it does NOT blanch .
Stage 2: Skin is visibly damaged and NOT intact with PARTIAL loss of the dermis. No subq will be visible. Wound may be opened with superficial red/pink opened ulcer or may have the formation of an opened or closed blister.
Stage 3: Skin is visibly damaged and NOT intact with FULL loss of the skin tissue. May see the subq . Wound edges may be rolled away..epibole. Bone, tendon and muscle NOT visible.
Stage 4: Skin is visibly damaged with FULL loss of the skin tissue that will expose bone, muscle, tendon, and ligaments.
Unstageable:
Slough or eschar is covering a full thickness ulcer. You cant assess the actual depth of the wound because of the slough or eschar covering the ulcer.
Deep-Tissue Injury:
Presents as purplish or blackish areas over skin that is intact. The fatty tissue below is injured. Also, may look like a black blister area. It may feel heavy or spongy.
Other Factors That Put Patients At Risk Include4
- Rigidity of devices
- Not easy to secure or adjust the device to the body
- Difficult to safely remove or lift the device to inspect the skin underneath
- Poor positioning or fixation of the device
- Inappropriate size of the device
- Limited knowledge of the impact of edema
- Failure to check tubing
- Lack of awareness of the need to remove, reposition and provide basic skin care underneath devices
- Limited best practice guidelines
What Bundle Of Best Practices Do We Use
Given the complexity of pressure ulcer prevention, with many different items that need to be completed, thinking about how to implement best practices may be daunting. One approach that has been successfully used is thinking about a care bundle. A care bundle incorporates those best practices that if done in combination are likely to lead to better outcomes. It is a way of taking best practices and tying them together in a systematic way. These specific care practices are among the ones considered most important in achieving the desired outcomes.
The pressure ulcer bundle outlined in this section incorporates three critical components in preventing pressure ulcers:
- Comprehensive skin assessment.
- Standardized pressure ulcer risk assessment.
- Care planning and implementation to address areas of risk.
Because these aspects of care are so important, we describe them in more detail in the subsequent subsections along with helpful clinical hints. While these three components of a bundle are extremely important, your bundle may stress other aspects of care. It should build on existing practices and may need to be tailored to your specific setting. Whatever bundle of recommended practices you select, you will need to take additional steps. We describe strategies to ensure their successful implementation as described in Chapter 4.
The challenge to improving care is how to get these key practices completed on a regular basis.
Resources
Additional Information
Tools
Practice Insights
Also Check: How To Heal Leg Ulcers
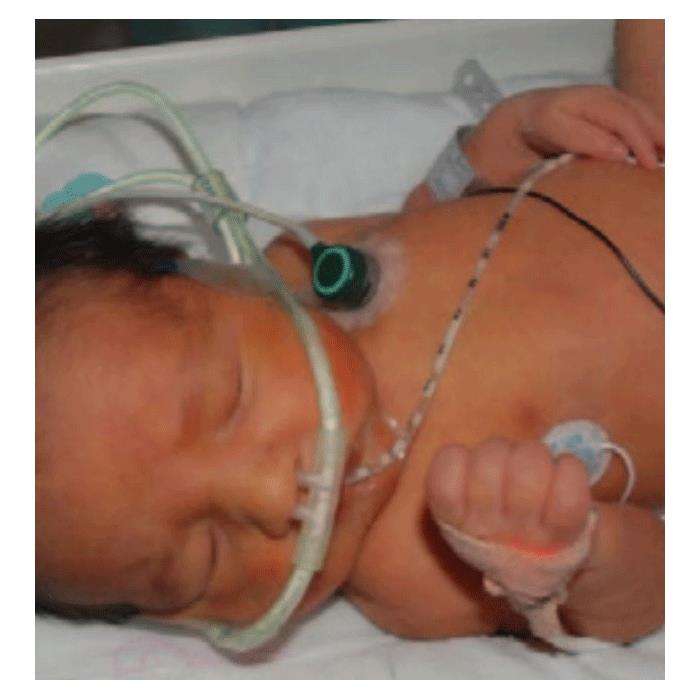
Ways To Lower The Risk Of Medical Device Related Pressure Injuries
Pressure injuries arent new to healthcare. Whats surprising is that more of these injuries are caused by medical devices. Today, medical device related pressure injuries account for more than 30% of all hospital-acquired pressure injuries.1
Currently the cost of pressure ulcers is $9.1$11.6 billion per year in the U.S.2 Reversing this trend, or even holding costs steady, seems unlikely as the U.S. population ages. The reality is, more patients who rely on medical devices for their treatment are being admitted to all healthcare settings.
Present On Admission Versus Facility Acquired

Of the 804 MDR PIs, 75% were facility acquired, and 25% were present on admission. Of the 10,847 non-MDR PIs, 35% were facility acquired, and 65% were present on admission .1). The MDR PIs were 2.1 times more likely to be facility acquired than non-MDR PIs. A 2 test revealed that the distributions shown in Figure Figure11 are significantly different from each other .
PERCENTAGE OF PRESSURE INJURIES PRESENT ON ADMISSION VERSUS FACILITY ACQUIRED
Abbreviation: MDR PI, medical-device related pressure injury.
Survey responders were asked to report the number of days the patient was in the facility before the facility-acquired PI was discovered. A t test found that facility-acquired MDR PIs formed on average 3 days faster than non-MDR facility-acquired PIs .3). The average number of days recorded before a non-MDR facility-acquired PI formed was 15 days, but the average number of days recorded before a facility-acquired MDR PI formed was 12 days .3). The sample sizes for this analysis are reduced because the survey responders occasionally did not fill in the number of days before a facility-acquired PI was discovered.
Read Also: Is White Rice Good For Ulcerative Colitis
How To Lower The Risk
A knowledgeable and empowered frontline staff can help reduce MDR pressure injuries. Margaret Falconio-West, BSN, RN, APN/CNS, CWOCN, DAPWCA, senior vice president, market solutions, Medline Industries, suggests these best practices:
Contributing Factors Of Pressure Ulcers
Many different issues can lead to a pressure ulcer or bedsore forming on the body. Its important for patients and caregivers to keep these in mind to avoid an ulcer from forming:
- Friction When the skin is rubbed by any material, friction may occur. If a patients skin is sensitive due to injury or other factors, friction can be very high-risk. Wearing soft clothes and changing bed linens regularly can help reduce the amount of friction that occurs when moving.
- Pressure Prolonged periods of pressure on a single part of the body can cause ulcers to form. Patients who cannot get out of bed or out of their chair for many hours need to regularly adjust and move their bodies to place pressure on different areas. The frequency of movement depends on the patient, but laying on a different side every two hours is a common remedy to ensure regular pressure changes.
- Shear When two surfaces move in different directions, shear may occur. This can happen if a patient is improperly seated or sliding down on an elevated bed. Caregivers should be aware of the patients positioning and the possibility of this extra pressure that could exist.
Avoiding these factors can help reduce or eliminate the chance of pressure ulcers from occurring. Every patients body will be different, so a variety of remedies should be considered when trying to stop pressure ulcers from forming.
Read Also: Natural Ways To Heal Stomach Ulcers
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Temperature.
- Skin integrity .
Tools
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Why The Shift From Pressure Ulcer To Pressure Injury
Vapotherm Clinical Nurse Educator
Jeanne Pettinichi has 34 years experience as a nurse, including 10 years experience as a Clinical Nurse Education Specialist at two Level I Trauma CentersChildrens National, DC and Cincinnati Childrens.
The views and ideas presented in this blog article are solely those of the author, and the content is not intended to serve as medical advice. Vapotherm does not practice medicine or provide medical services. Practitioners should refer to the full indications for use and operating instructions of any products referenced herein before prescribing them. Jeanne Pettinichi is an employee of Vapotherm.
If you, like me, started your clinical career decades ago, you probably heard the term pressure ulcer over and over again. But the term pressure injury has become much more prevalent now when discussing wound care and prevention. It even happened that recently, the National Pressure Ulcer Advisory Panel officially changed their name to National Pressure Injury Advisory Panel .
The word ulcer connotes an open sore, while injury doesnt have to. For example, if I have a patient who has a tightly strapped mask on his face and develops redness and swelling along the bridge of his nose, that is a pressure injury. The skin may not be broken at all. By calling these incidences pressure injuries, the language we use more accurately describes our patients reality.
Prevention Strategies
Read Also: Signs Of Ulcerative Colitis Flare Up
A Covered Pressure Ulcer Heals Faster
Pressure ulcers generally take a long time to heallonger than most wounds. The healing process is even slower if the patient has diabetes, circulation problems, or blood clotting disorders. Making matters worse, a skin infection is possible any time there is a break in the skin. When a pressure ulcer becomes infected, it slows down the healing process even further and greatly complicates the situation
According to the National Pressure Ulcer Advisory Panel , pressure ulcers should be kept covered with appropriate dressings. The reason: a covered wound heals faster than an uncovered wound. The NPUAP recommends covering pressure ulcers of all stages and severities. Stage 1 pressure ulcers should be covered to reduce the risk that the skin will break down. Covering the wound helps maintain a moist environment in Stage 2 pressure ulcers. Experts recommend covering non-infected Stage 2 pressure ulcers with moist dressings. On the other hand, infected Stage 2 pressure ulcers should be covered with a dressing that removes excess fluid from the wound. A wound care nurse or physician should manage Stage 3 and Stage 4 pressure ulcers however, even these severe wounds should be kept covered with the correct dressings.
International Pressure Ulcer Prevalence Survey
The IPUP survey has been conducted since 1989.7 It is an international, voluntary survey to enable facilities to benchmark and track their PI prevalence rates against other, similar facilities. Originally, only acute care hospitals participated, but current data include acute care hospitals, long-term acute care hospitals, long-term care, and rehabilitation facilities. The survey has grown over the years from 148 facilities and 34,987 patients participating in 1989 to approximately 1000 facilities surveying approximately 100,000 patients per year. In 2007, medical devicerelated pressure ulcers were added to the survey form. In 2016, a field to indicate the type of device that caused the MDR PI was added. The list of the devices that the survey responder had available to choose from included:
Primary analyses consisted of summary statistics . A t test was used to compare MDR PIs to non-MDR PIs based on days until facility-acquired PIs developed. 2 tests were used to determine whether the distribution of MDR PIs versus non-MDR PIs was significantly different by care setting, whether the PI was present on admission or facility acquired, injury stage, and anatomic location. Significance was set to .05 for all analyses. This study was reviewed by the Schulman institutional review board and found to be exempt.
You May Like: Boost Vs Ensure Ulcerative Colitis
In Addition To Applying Dressings Beneath Medical Devices Continue To Lift And/or Move The Medical Device To Examine The Skin Beneath It And Reposition For Pressure Relief
This recommendation is from expert opinion. It is appreciated that the use of a dressing on the skin beneath a medical device is not a replacement for other prevention strategies. Skin should be inspected according to agency policy or accepted standards of care. Skin must be inspected for signs of pressure due to the device, which cannot be seen while the device is still in place. For example, an endotracheal tube must be moved to inspect the lips for pressure injury. In obese patients, the medical device may become hidden it the skin folds, and the nurses need to be diligent to account for all medical devices in these patients. Threequarters of devicerelated PUs were not identified until they were stage III, stage IV or unstageable compared with 54% of nondevicerelated PUs. Twenty percent of nondevicerelated PUs were first identified when they were stage I, compared with only 5% of devicerelated ulcers 5. The dressing must be removed to visualise the skin, and then reapplied before replacing the medical device. An important consideration is the ability of dressing to be removed without injury to the skin during repeated assessments. The bridge of the nose is thinly covered with skin and could be easily injured with highly adhesive dressings. If possible, avoid placing a medical device back onto pressureinjured skin.
Better Care With Reduced Costs
35% of all pressure ulcers acquired in hospital from medical devices affect the ears1. Flexicares soft-touch tubing minimizes stresses in this delicate area, reducing the potential for skin breakdown and associated costs.
Improved Patient Compliance and Comfort
Avoids Additional Treatment Costs
Recommended Reading: What Can I Take For Ulcerative Colitis Pain
Risk Factors For Pressure Injury Development
Risk Factors: think of any patient population that has issues with alleviating pressure on a bony prominence or will have issues with skin integrity
- Poor Nutrition.decreases skin integrity
- Immobile.cant alleviate pressure
- Neuro Issues: unaware of the need to shift weight.spinal cord injuries or altered mental status.cant alleviate pressure
- Diabetics.decreased awareness with sensory and decreased circulation
- Incontinence of urine or stool.decreases skin integrity
- Activities that cause friction and shear.patient sliding down in the bed or not properly moved up in the bed etc.
How To Put On A Nasal Cannula
To find the right nasal cannula placement, insert the prongs of your oxygen nose piece into your nostrils, then take the oxygen tubes on either side of your face and lift the tubes, placing them over your ears like you would glasses. Then, use the slider that holds the tubes where they come together under your chin to adjust the fit. The tubes of your nasal cannula should fit snugly over the tops of your ears and against your jaw and chin. You should have enough room to fit two fingers between the tubing and your chin for the most comfortable nasal cannula fit. If you are able to wear it comfortably after a couple uses, you are wearing it correctly! If you find that it is uncomfortable, however, here are a few tips.
Recommended Reading: Removing Colon Due To Ulcerative Colitis
Pressure Ulcers Can Be Serious
Pressure ulcers cause a considerable amount of suffering. Not only are they painful, but they put patients at risk for other illnesses. For instance, pressure ulcers can and often do become infected. This infection can stay in and around the ulcer, or it can spread to the bloodstream. Tissue that is starved of oxygen and nutrients will die, leaving black, necrotic tissue. Indeed, patients with severe pressure ulcers may need one or more surgeries to treat the affected area. Therefore, anyone who cares for someone at risk for pressure ulcers should look for pressure ulcers diligently and treat them aggressively.
Reduction Of Respiratory Device
Jan 10, 2020 | Clinical, Department Management, ICU & Ventilation |
Respiratory devices such as NIV masks, ETT/tracheostomy devices and holders, and nasal cannula can cause pressure injuries to patients. A study by researchers at Baptist Medical CenterJacksonville found that a targeted intervention implemented within its RT department successfully prevented respiratory device-related pressure injuries in acutely ill patients.
It is estimated that $11 billion is spent annually in the United States on pressure injuries, with the average cost per injury being $500-$70,000. When the Centers for Medicare and Medicaid Services changed reimbursement rules in 2006, hospital-acquired pressure injuries became a priority for hospitals because CMS saw pressure injuries as a preventable injury for inpatients. CMS deems Stage 3 and Stage 4 pressure injuries to be preventable while admitted as inpatients to medical facilities.
Pressure ulcers are a real concern to acute and long-term care facilities because they increase morbidity, cost of care, and decrease reimbursement. In addition, the presence of these injuries can cause pain for the patient and emotional distress, not only for the patient but also for their family.
At Baptist Medical Center , there had been an increase in pressure injuries from respiratory devices documented in the healthcare systems adverse events reporting system.
Methods
The facility interventions were as follows:
Results
Discussion
Recommendations
Recommended Reading: Crohn’s Disease And Ulcerative Colitis Differences