What If Youve Had Surgery For Uc
If youve had surgery for UC, such as an ileostomy , your GI may give you specific guidelines regarding your diet and nutrition. For example, they may recommend you eat extra foods with vitamin B12 or take a supplement since removal of the ileum can make it hard for you to absorb the B12 you need. A lack of this vitamin can affect the health of your nerve and blood cells.
Its also extra important to stay hydrated if youve had surgery for UC, so make sure youre drinking lots of water and eating foods with a high-water content. Talk with your health care team and registered dietitian to understand how your surgery may affect your dietary needs.
Ulcerative Colitis Treatment Medications
Treatments for ulcerative colitis includes both medications and surgery however, there is no medication that can cure ulcerative colitis. Medicationsthat treat ulcerative colitis are
- anti-inflammatory agents, for example, 5-ASA compounds like sulfasalazine , and olsalazine , and topical and systemic corticosteroids), and
- immunomodulators, for example, 6-mercaptopurine , azathioprine , methotrexate , cyclosporine .
Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohns disease.
Dont Miss: What Can I Take For A Stomach Ulcer
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
You May Like: Treating Leg Ulcers With Sugar
Natural Remedies For Ulcerative Colitis
11 min. read
Dr. David Williams
Ulcerative colitis is a serious inflammation of the lower bowel. This inflammatory bowel disease seems to be hereditary and usually begins between the ages of 15 and 40. Ulcerative colitis is rare in most populations that havent adopted the typical Western diet that is high in refined carbohydrates and fats and low in fiber. And in some cases, ulcerative colitis has been linked to allergic reactions to certain foods. Corn, wheat, and milk products seem to be the most common culprits.
With ulcerative colitis, the inflammation of the lower bowel surface often results in ulcerations that lead to profuse bleeding, along with other symptoms including severe, chronic diarrhea and bloody, mucus-laden stools. If the condition persists, the individual will suffer from fat, protein, vitamin, and mineral deficiencies. If ulcerative colitis continues for 10 years or more, studies have shown the risk of developing colon cancer is almost 200 times greater than that of the general population.
Most doctors in this country rely on powerful drugs to treat ulcerative colitis, even though their side effects can be substantial and their success rate is relatively low.
My plan below, however, consists of proven all-natural therapies, along with a few additional alternative remedies to try for especially stubborn cases. Of course, because ulcerative colitis can turn severe in some instances, it should always be monitored by a doctor.
What Is The Research Into Vsl#3 And Other Bowel Conditions

VSL#3 is also licensed to be used as a medical food in the dietary management of irritable bowel syndrome following various studies into VSL#3 and IBS. One study8 found that IBS patients taking VSL#3 had less abdominal pain and less abdominal distention and/or bloating and it significantly improved their quality of life.
Also Check: Natural Cure For Peptic Ulcer
Supplements Being Studied For Ulcerative Colitis
Researchers are checking a number of supplements to see if they can help people with UC. In at least one study, omega-3 fatty acids found in fish oil reduced symptoms and prevented UC from returning. Other studies, however, have not had the same results.
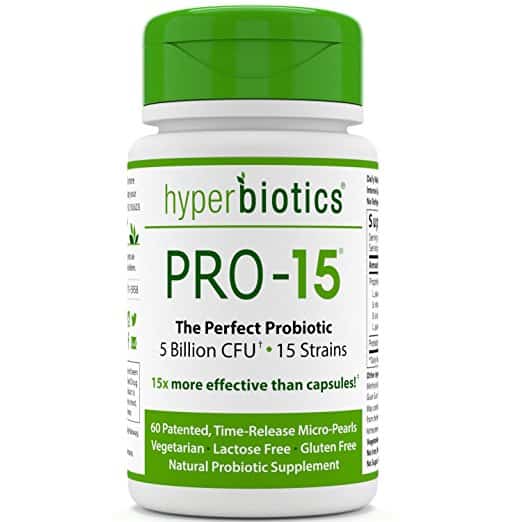
Probiotics are “good” bacteria or other microorganisms that can be healthful. Several studies show they reduce ulcerative colitis symptoms. The thinking is that probiotics, like lactobacillus or live-culture yogurt, help to restore balance to the good bacteria that live inside the intestines.
A few studies have seen benefits from aloe vera when you take it in the form of a gel that you swallow, but more research is needed to confirm this.
Talk to your doctor about other supplements that are being studied to see if they can help you manage ulcerative colitis.
Show Sources
Good Bacteria Show Promise For Clinical Treatment Of Crohns Disease Ulcerative Colitis
- Date:
- University of North Carolina Health Care
- Summary:
- A new study shows how a novel consortium of bacteria that live in the digestive tracts of healthy individuals can be used to prevent and treat aggressive colitis in humanized mouse models.
A new study published in Nature Communications demonstrates that a consortium of bacteria designed to complement missing or underrepresented functions in the imbalanced microbiome of inflammatory bowel disease patients, prevented and treated chronic immune-mediated colitis in humanized mouse models. The studys senior author, Balfour Sartor, MD, Midget Distinguished Professor of Medicine, Microbiology and Immunology, Co-Director of the UNC Multidisciplinary IBD Center, said the results are encouraging for future use treating Crohns disease and ulcerative colitis patients.
The idea with this treatment is to restore the normal function of the protective bacteria in the gut, targeting the source of IBD, instead of treating its symptoms with traditional immunosuppressants that can cause side effects like infections or tumors, Sartor said.
GUT-103 and GUT-108 were given orally three times a week to germ-free mice that had been specially developed and treated with specific human bacteria, creating a humanized mouse model. The therapeutic bacteria consortia worked by addressing upstream targets, rather than targeting a single cytokine to block downstream inflammation responses, and reversed established inflammation.
Story Source:
You May Like: Stage 2 Pressure Ulcer Characteristics
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
A Look At The Research So Far: Clinical Trials For Probiotics And Crohns Disease
A non-pathogenic strain of E.coli has been one of the most clinically trialled probiotics with regard to Crohns disease. In a 1997 double-blind study by Malchow5 E.Coli Nissle 1917 or placebo was taken daily for twelve months by 32 patients with active Crohn’s disease. Both groups also received standard steroid treatment at the same time. The results showed that whilst remission rates were similar for both groups the subsequent relapse rates were lower in the E.coli treated group . This means that once remission had been achieved less of the probiotic group re-developed symptoms. Whilst this particular strain of E. coli has shown probiotic potential, we would suggest practitioners wait for more research before seeking out any E. coli supplements, as of course other strains of this bacteria are well documented and widely known for their pathogenic effect on the human body. E. coli does not appear on the European Food Safety Authority’s Qualified Presumption of Safety list.
The fact that the relapse rate was significantly lower in patients treated with the drug in combination with S. boulardii, suggests a protective effect from the probiotic.
You May Like: How To Treat Ulcerative Colitis Pain
Myths And Facts About Ulcerative Colitis
to make your appointment today.
Ulcerative colitis affects about 1 million people in the United States. This form of inflammatory bowel disease affects your colon, causing inflammation and subsequent irritation and digestive distress.
Symptoms usually develop over time and can progress to a point where theyre debilitating with the possibility of life-threatening complications. The board-certified gastroenterology team at Digestive Disorders Associates cant cure your ulcerative colitis no one can but we can help greatly reduce the symptoms of the disease.
If youre newly diagnosed with ulcerative colitis or have been living with it for a while, understanding some of the myths and facts associated with your condition can help you achieve remission.
What To Do During An Ulcerative Colitis Flare To Minimize Symptoms
Youll inevitably experience another UC flare-up at some point, despite your best prevention efforts. When this happens, there are a few ways youll need to tweak your normal routine to minimize the severity of your symptoms and get back into remission ASAP. Even some of your typically healthy habits like loading up on veggies may be a no-go. Here are a few natural remedies that may help:
Dont Miss: Best Fruits For Ulcerative Colitis
Also Check: Treatment Of Ulcerative Colitis In Child
Medication For Ulcerative Colitis
If diet alone doesnt control your symptoms, your doctor may suggest medication. Some medications address inflammation so your bowel can heal. Other medications help you stay in remission when your ulcerative colitis is under control.
Aminosalicylates: These anti-inflammatory drugs treat mild or moderate ulcerative colitis or help extend remission.
Corticosteroids: Steroids provide short-term help for moderate to severe ulcerative colitis.
Immunosuppressants: These treat people with moderate to severe ulcerative colitis and help them stay in remission. Immunosuppressants can also treat severe ulcerative colitis in people who are hospitalized.
Biologics: These drugs are derived from naturally occurring chemicals. They treat people with moderate to severe ulcerative colitis and help them stay in remission.
If you have ulcerative colitis, ask your doctor what treatments will work best for you.
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
You May Like: Foods You Can Eat With An Ulcer
You May Like: What Are Infusions For Ulcerative Colitis
How We Select Supplements
Our team works hard to be transparent about why we recommend certain supplements you can read more about our dietary supplement methodology.
We support supplements that are evidence-based and rooted in science, as well as clinically tested and approved for use in humans. We value certain product attributes that we find to be associated with the highest quality products. These attributes include non-GMO, Organic, and allergy-friendly products that are free of most artificial ingredients including colors, flavors, preservatives, and sweeteners. When possible, we recommend products that are third-party tested and certified.
It’s important to note that the FDA does not review dietary supplements for safety and effectiveness before they go to market. Our team of experts has created a detailed, science-backed methodology to choose the supplements we recommend.
Here, the best probiotics:
-
Helps with diarrhea, gas, and bloating
-
For adults and kids
Food Supplements For Ulcerative Colitis
A well-balanced diet is your first step to guard against malnutrition. You need to eat a variety of things from different food groups and make sure you get enough protein and calories. Work with a dietitian who can help you plan meals that meet your nutrition needs.
Even with a well-designed meal plan, you may still need some of these supplements:
Vitamin D. You need it to keep your bones strong. It also plays a role in how your immune system — your body’s defense against germs — works.
If you have ulcerative colitis, especially if you need steroids, you may be at risk for having low levels of vitamin D.
A good source of vitamin D is dairy foods, but a lot of people with UC cut back on dairy to help them curb symptoms of diarrhea.
Experts have different views on vitamin D supplements, so ask your doctor if it’s a good idea for you to take them.
Calcium. It’s a mineral your body uses to build bones, help your muscles contract, and send messages through your nervous system.
If your system doesn’t have enough calcium, your body removes it from the bones, which causes them to become brittle and leads to a bone-weakening disease called osteoporosis.
If you avoid calcium-rich dairy products or need certain kinds of medicines, you could be at risk for low levels of calcium. If your doctor recommends a calcium supplement, you’ll probably need 1,000 to 1,200 milligrams a day.
Also Check: Average Age Of Ulcerative Colitis Diagnosis
Probiotics Bacteria And Gut Health
Often, bacteria are perceived as dangerous germs that lead to the development of disease. For instance, many people are familiar with strep throat a bacterial infection caused by the bacteria streptococcus. However, bacteria like probiotics can also be beneficial to your health, and many naturally live in the human body as part of the microbiome.
The microbiome and the bacteria in it are critical for proper digestion and overall health. The good bacteria within the microbiome are responsible for:
- Producing certain vitamins and amino acids
- Breaking down toxic food, complex carbohydrates, and sugars including lactose, which is broken down by the bacteria Lactobacillus rhamnosus
- Forming short-chain fatty acids, which some clinical trials have demonstrated may help treat Crohns disease
The microbiome is responsible for many vital functions, so protecting and maintaining its health is important. Ingesting probiotics can help maintain and even boost the population of good bacteria in the gut. These good bacteria help preserve and thicken the barrier in the GI tract that blocks harmful bacteria from penetrating the lining of the GI tract . Probiotics may also help manage the health of the gastrointestinal immune system and reduce intestinal inflammation.
Probiotics For Ulcerative Colitis
The AGA doesnt recommend probiotics for treating ulcerative colitis outside of use in a clinical trial. As with Crohns disease, the limitations in the type of studies that have been done so far are the main factor in this decision.
The AGA found 11 studies done using probiotics for treating ulcerative colitis. They used various different strains of probiotics, which makes comparing these studies difficult.
There were four studies that compared the use of probiotics with the medications mesalamine or balsalazide. A few of the studies allowed co-therapy with steroids and one was done with the use of probiotic enemas in children.
While the evidence was considered low, the AGA does indicate that for some of the studies, the benefit was uncertain. There was one study that showed a potential for benefit. This appears to be in contrast to Crohns disease, where there doesnt seem to be much indication that probiotics might be beneficial.
Theres a call for more research and there are no recommendations for using probiotics for ulcerative colitis.
Also Check: How To Ease Stomach Ulcer Pain
How To Take Probiotic Supplements
We cant stress enough that its a good idea to visit a doctor and/or a registered dietitian before taking something new to treat ulcerative colitis.
They may have some advice about which probiotic to take and what dosage might be right for you.
Probiotic dosage for ulcerative colitis is not an exact science. The dosages found to be effective in various studies usually range from 2 billion to 25 billion colony-forming units . The more bacteria, the merrier.
Check the expiration date and make sure to store them properly, refrigerating them if recommended on the packaging. These are living organisms that require a little TLC, and they die out over time if not used.
What Really Causes Ulcerative Colitis
From my years of experience of having helped hundreds of people treat ulcerative colitis without being dependent on long term medications, I feel I have gained a good understanding of what causes ulcerative colitis, and how to cure ulcerative colitis naturally.
Most doctors will not question the conventional and somewhat vague medical reason, which I was told was an autoimmune disease with no known cause.
I asked my gastrointestinal consultant if she knew how to cure ulcerative colitis naturally, whether chronic stress was a cause, as I was in a very stressful career and I asked whether my diet that was high in gluten may be a trigger factor?
She said there was no proof for this and basically told me to shut up and keep taking the pills as they were the only approved treatment. I really wanted to know the true cause because with this knowledge I would then be able to figure out how to cure ulcerative colitis naturally, without being dependent on the medications that were making me feel much worse!
From deep personal introspection and by going back to my own feeling for what causes ulcerative colitis in myself, I believe the main causes for most people are:
Dont Miss: How To Cure Ulcerative Proctitis
Also Check: Ulcerative Colitis And Blood Thinners