Living With Uc: Probiotics
These “friendly” bacteria are similar to those that live in your intestine and prevent the growth of too many harmful bacteria. We need more research to know if probiotics can help with ulcerative colitis. You can find probiotics in some yogurts, milk, tempeh, and soy beverages. Or you can buy them as supplements.
Pain As A Tool For Diagnosis
Because pain can come from different sources, and pain in the abdomen is particularly difficult to pinpoint, it is not a symptom that is normally used to diagnose IBD or a particular form of IBD.
Rather, the type and location of pain is more often used together with other signs and symptoms when diagnosing IBD or other conditions. In other words, it might be a starting point to help a healthcare provider know where to start looking for inflammation, but it’s only one part of the picture.
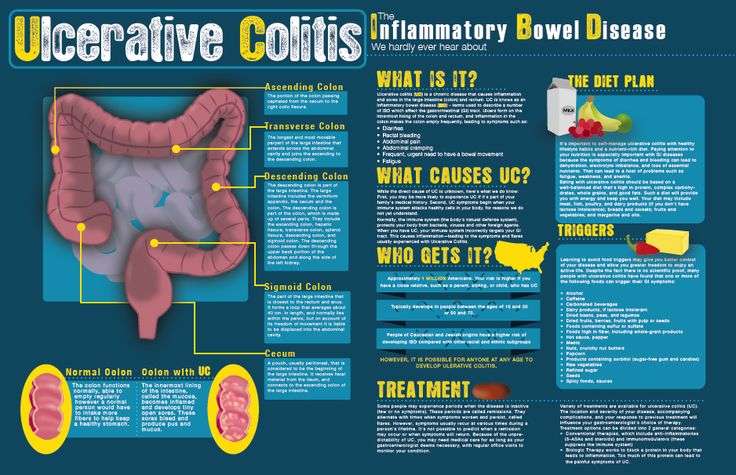
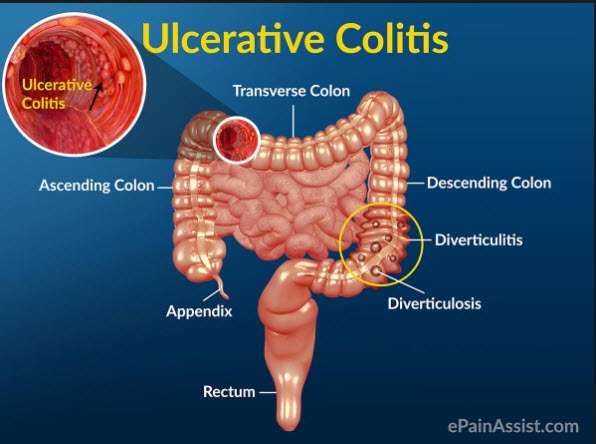
Types Of Ulcerative Colitis
The types of ulcerative colitis depend on where it occurs in the body. There are several types of ulcerative colitis, and symptoms vary depending on the location. The types of ulcerative colitis include:
- Ulcerative proctitis: The mildest form of ulcerative colitis inflammation is in the rectal area and causes rectal pain and bleeding and the feeling of needing to go to the bathroom urgently.
- Proctosigmoiditis: The inflammation is in the rectum and lower area of the colon, and causes stomach pain and cramping, bloody diarrhea and trouble going to the bathroom despite the urge to go.
- Left-sided colitis: The inflammation extends from the rectum through the sigmoid and descending colon, in the upper-left abdomen, and causes stomach pain and cramping on left side, bloody diarrhea and weight loss.
- Pancolitis: Inflammation of the entire colon that causes stomach pain and cramping, bloody diarrhea, significant weight loss and tiredness.
- Fulminant colitis: The rarest form of ulcerative colitis, this inflammation of the entire colon can be life-threatening. It can cause extreme diarrhea, dehydration and shock.
Talk to your doctor if you have diarrhea plus stomach pain, blood in your stool or a fever that lasts more than a couple of days or that doesnt get better with over-the-counter medications.
Don’t Miss: How To Treat Oral Ulcers
What Pain Relief Medicines Are Used In Inflammatory Bowel Disease
There are a variety of pain relief medicines available which can help to control pain in Crohns disease and ulcerative colitis.
Paracetamol
Paracetamol is a commonly used over-the-counter painkiller you can buy without a prescription. It can be used to help with mild to moderate pain, and can also help to control a high temperature. Paracetamol can be used by adults and children and is available in a variety of forms, including:
- Tablets, capsules and caplets
- Oral suspension
- Suppositories
Paracetamol works by blocking the production of chemicals in your body called prostaglandins, making your body less aware of any pain. It also reduces your temperature by acting on the part of your brain responsible for controlling it.
Paracetamol is often combined with other medicines, including other types of painkillers. Always check any additional medicines are also safe for you to use.
It is generally considered safe to take paracetamol if you have inflammatory bowel disease, however if you need to take paracetamol for longer than three days, or have a new pain, you should speak to your IBD team.
Two paracetamol tablets every four hours, up to four times a day is considered a safe dose for adults. Side effects are uncommon with paracetamol.
You should read the patient information leaflet in your medicine packet to check if paracetamol is suitable for you. Do not take more than the maximum dose in a 24 hour period as an overdose of paracetamol can be very dangerous.
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
Recommended Reading: Ulcerative Colitis Joint Pain Treatment
How To Deal With Ulcerative Colitis
Ulcerative colitis, a type of inflammatory bowel disease, causes painful open sores in your large intestine and rectum. The disease can affect both children and adults. Although there is currently no cure for ulcerative colitis, symptoms can be managed with medications and dietary changes in many cases.
What are the symptoms of ulcerative colitis?
Although symptoms of ulcerative colitis vary depending on the severity of the disease, diarrhea that contains blood or pus is a frequent problem. It may be difficult to get the bathroom in time, particularly if a bout of diarrhea strikes in the middle of the night. Other symptoms can include:
- Nausea
- Fatigue
- Difficulty defecating
If you have severe ulcerative colitis, you may be more likely to develop one or more serious complications, such as severe dehydration or bleeding, a perforated colon, osteoporosis, megacolon, blood clots or colon cancer.
What are the risk factors for ulcerative colitis?
Ulcerative colitis symptoms usually appear between the ages of 15 and 35. You’re more likely to develop ulcerative colitis if other people in your family have it. Your ancestry may also affect your risk. Caucasians and people of Ashkenazi Jewish descent get the disease more often than other ethnic groups.
How is ulcerative colitis treated?
Whats A Good Plan To Manage Uc Cramping
Monitor your medications. Talk to your doctor about any prescription, over-the-counter, or herbal medications youre taking. Iron deficiency is common with UC, but oral iron supplements have been shown to increase the risk of inflammation and cramping. Some antibiotics and pain relievers, such as ibuprofen, may also increase flare-ups and cramping.
Review your diet. Keep a food diary and note the connection between the foods you eat and your UC symptoms. In general, its smart to stay away from processed foods and those high in saturated fat and sugar. High-fiber foods and dairy products can also cause UC cramping, but check with your doctor before eliminating foods from your diet, to ensure youre getting the nutrients you need.
Eat frequent, small meals. Instead of two or three large meals, eat four to six smaller meals spaced more closely throughout the day. Also, take your time while eating and chew thoroughly.
Skip caffeine and carbonated drinks. Caffeine can cause gas, intensifying abdominal cramping. It is also a stimulant, which can make cramping and diarrhea worse.
Drink enough water. People with UC may be at increased risk of dehydration, so be sure to drink plenty of H2O. A good rule of thumb, according to the Crohns and Colitis Foundation, is to aim for about 64 ounces or eight 8 oz glasses per day.
Read Also: Best Meds For Ulcerative Colitis
Prevent Bloating With A Change In Diet
The easiest way to prevent bloating is to avoid gas-causing foods as mentioned above. When changing your diet in a drastic way, please consult your doctor before doing so.
We hope that you use our tips on how to relieve ulcerative colitis, but if your abdomen feels tender, your bloating worsens or is accompanied by other symptoms, please seek immediate medical attention. If your symptoms dont go away, you will likely need medical interference. Stop by Village Emergency Centers in Katy, River Oaks, Clear Creek, or Jersey Village for the quality medical care that you deserve.
Further Reading:
Prognosis Of Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have ulcerative proctitis have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
Read Also: Ulcerative Colitis Abdominal Pain Relief
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
Could My Symptoms Be Ibs
Irritable Bowel Syndrome is a different condition from IBD, although some of the symptoms are similar. Like Crohn’s and Colitis, IBS can cause abdominal pain, bloating and bouts of diarrhoea or constipation. However, it does not cause the type of inflammation typical of Colitis, and there is no blood loss with IBS.
Some people with Colitis may develop IBS-like symptoms, for example experiencing diarrhoea even when their Colitis is inactive. These symptoms may need slightly different treatment from their usual IBD symptoms. IBS is more common in people with IBD than in the general population.
If you develop diarrhoea with bleeding and abdominal pain, your doctor may suspect you have Colitis, particularly if you are a young adult or have a family history of Crohn’s or Colitis. You will need tests and physical examinations to confirm a diagnosis. See Tests and Investigations for IBD.
You may need to have tests repeated from time to time to check on your condition and how your treatment is working.
Some drug treatments may also require a series of blood tests and, occasionally, x-rays or scans to check for any potential side effects. Your specialist will avoid giving you any unnecessary tests or investigations.
You may need more regular colonoscopies when you have had Ulcerative Colitis for a long time to check for any signs of cancer.
Also Check: List Of Foods Good For Ulcers
When Should You Call Your Doctor
If youre experiencing certain symptoms, chances are, your current treatment is not working and its time to consider a change in therapy, says Ha. Call your doctor if:
- Cramping is severe
- Youre experiencing a significant amount of abdominal pain that requires medication
- You have a fever that lasts longer than a couple of days
- You experience nausea or vomiting
- You have ongoing diarrhea or blood in your stool
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
You May Like: Ulcerative Colitis And Lactose Intolerance
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Recommended Reading: How To Heal An Ulcer In Your Mouth
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with ulcerative colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 138,000 members come together to ask questions, give advice, and share their stories with others who understand life with ulcerative colitis.
Are you living with ulcerative colitis pain? What has helped you to manage it? Share your experience in the comments below, or start a conversation by posting on your Activities page.
Don’t Miss: How Do You Know You Have A Stomach Ulcer
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
Read Also: How To Fix A Stomach Ulcer
People Describe How They Were Diagnosed With Ulcerative Colitis
Ulcerative colitis, or UC for short, is a form of inflammatory bowel disease that affects portions or all of your large intestine and rectum. The Centers for Disease Control and Prevention estimates that 3.1 million Americans have IBD, which also includes Crohn’s disease .
UC is a chronic condition that can cause long-term inflammation and ulceration, severe diarrhea, abdominal pain, blood and mucous in your stool, urgency, nausea, joint paint, fever, weight loss, and fatigue. UC is also a risk factor in colorectal cancer, according to the Mayo Clinic. And while there’s no known cure for ulcerative colitis, removal of the colon and rectum in a procedure called a proctocolectomy can eliminate the disease.
Other treatment options include corticosteroids, anti-inflammatory drugs called 5-aminosalicylates, immunosuppressant biologics , and bowel resection or removal. Patients can also manage symptoms with pain medication, anti-nausea medication, and antidiarrheals, though all medications should be taken under the care of a doctor. IBD is often confused with irritable bowel syndrome , a disorder that causes pain and cramping of the large intestine. But unlike IBD, IBS doesn’t cause long-term damage to your intestinal tissue or increase your risk of colorectal cancer.
Managing UC is a complex puzzle of treatment options and unpredictable symptoms. We spoke with nine women to find out what life is like with the disease.
Responses have been edited for length and clarity.
Related: