Ulcerative Colitis And Genes
Your genes appear to play a part in whether you get UC. Researchers have found variations in several genes that they think are linked to the condition. Some of these genes are thought to be involved in your immune system. Others are associated with protecting your intestines.
Youre more likely to get UC if a relative has it. Research has found that up to 1 out of every 4 people with the condition has a family history of inflammatory bowel disease .
Anyone can get ulcerative colitis. But some groups, including white people and those of Ashkenazi Jewish descent, are at higher risk of getting UC than others. This also suggests a genetic connection.
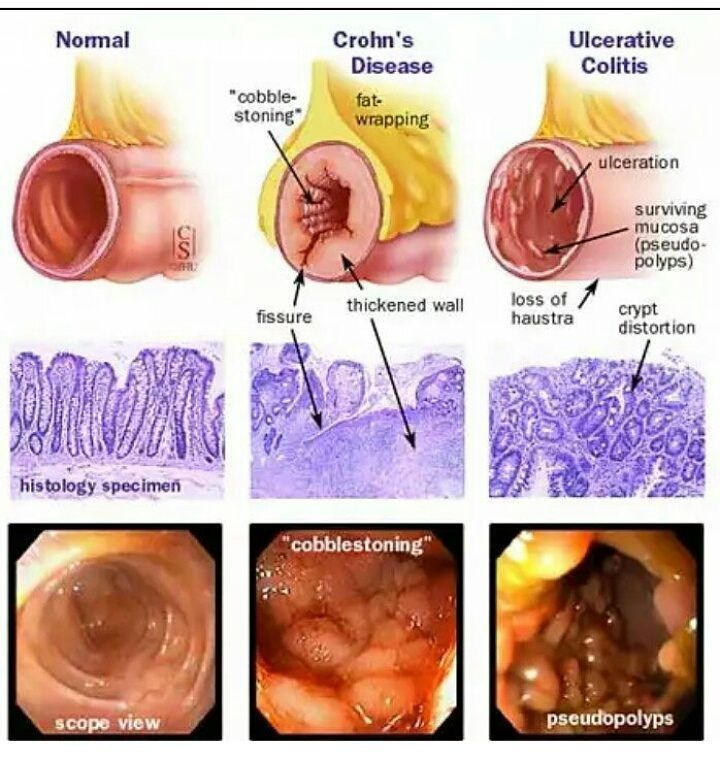
What Are Symptoms Of Crohns Disease And Ulcerative Colitis
Symptoms of Crohns disease and ulcerative colitis that are similar include:
Crohns disease can also cause symptoms in the body outside the GI tract, including:
Additional symptoms of ulcerative colitis may include:
For both conditions, relapses, when inflammation and symptoms worsen can occur, followed by periods of remission that can last months to years when symptoms subside.
Complications Of Ulcerative Colitis
A small number of people with colitis can develop inflammation in other parts of the body, such as the liver, skin, joints and eyes.
Regular monitoring by a gastroenterologist, as well as colonoscopies, may help prevent complications from developing. But medications, including steroids and drugs designed to prevent inflammation and occasionally surgery may be needed.
Osteoporosis can develop as a side effect of long-term corticosteroid use.
Cases of marked inflammation caused by UC can also lead to:
- nutritional deficiencies
- heavy bleeding due to deep ulcers
- perforation of the bowel
- problems with the bile ducts, affecting the liver
- fulminant colitis and toxic megacolon, conditions that cause the bowel to stop working
In the long-term, UC is associated with an increased risk of developing bowel cancer. After 10 years the risk of bowel cancer is 1 in 50, and after 20 years it increases to 1 in 12. This risk can be decreased by maintaining a healthy diet, exercising and avoiding alcohol and smoking.
Read Also: How Long Does An Ulcerative Colitis Flare Up Last
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
Read Also: Is Papaya Good For Ulcerative Colitis
Environmental Factors And Ulcerative Colitis
A germ, like a virus in your environment, might raise your chances of getting ulcerative colitis.
If you use nonsteroidal anti-inflammatory drugs, antibiotics, or birth control pills, your chances of having it may increase slightly. Its possible a high-fat diet is related to it, too.
A few other things could be related to the cause or might trigger a flare-up:
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Also Check: How Long To Ulcerative Colitis Flare Ups Last
You May Have An Increased Risk Of Colorectal Cancer
When theres inflammation in the colon, the cells in the lining of the colon continuously turn over to try to repair the damage, explains the Crohns & Colitis Foundation. This constant turnover can increase the odds of a mutation occurring that can lead to cancer.
If there are any irregular polyps or growths in your colon, unchecked inflammation can make it difficult for your doctor to spot them during a colonoscopy. You really want to have a clean slate when you do a colonoscopy, so your doctor can be sure everything looks good, Bonthala says.
How Does Ulcerative Colitis Increase The Risk Of Colorectal Cancer
If you have ulcerative colitis, your risk of developing colon cancer is higher if you have the following conditions:
- An ulcerative colitis diagnosis at a young age
- Had ulcerative colitis for more than eight years
- Ulcerative colitis that affects most of your colon
- Uncontrolled inflammation
- Damage to your livers bile duct from inflammation or scarring
- Family history of ulcerative colitis
Read Also: Do Ulcers Make You Throw Up
It Can Affect You Mentally Too
Beyond the physical symptoms, UC might also impact your mental health.
Fighting a war with your own body can take a mental toll.
- Around 35% of people with UC or Crohns disease experience symptoms of anxiety.
Note: A UC flare on its own typically doesnt lead to a new mental health condition like depression or anxiety, says Dr. Max Pitman, gastroenterologist at Salvo Health. But UC might worsen your existing anxiety or mood-based issues through the gut-brain connection.
When Im flaring up, its like being stuck in a dark fog. I feel hopeless, anxious, and even guilty often because I feel too exhausted to stick to work deadlines and have to cancel plans.
But, I had to learn how to give myself a break. Im not lazy: Im just tired. I have a chronic illness that impacts my gut. And my gut may affect my brain, in turn: One review found that people with IBD have higher rates of anxiety when the disease is active versus in remission, suggesting an upset gut may play a part in mental distress.
If youre having trouble managing your mental health, treatments like cognitive behavioral therapy could help.
Pitman recommends a form of CBT called gut-directed cognitive behavioral therapy, which helps you learn coping methods for your thoughts and emotions when you have a GI illness. Some research even suggests that gut-based CBT might improve digestive tract symptoms.
Recommended Reading: How To Stop Ulcers From Hurting
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Recommended Reading: How To Stop Ulcer Pain Instantly
Systemic And Extraintestinal Symptoms
Systemic symptoms affect the whole body. Extraintestinal symptoms affect areas of the body outside the intestines.
While these symptoms are less common than bloody diarrhea and abdominal pain, 25-30% of those with UC will have extraintestinal symptoms. The most frequent is peripheral arthritis. This is a type of arthritis that commonly affects the elbows, wrists, knees, and ankles.
Other examples of systemic or extraintestinal symptoms of ulcerative colitis include:
- Weight loss or muscle wasting
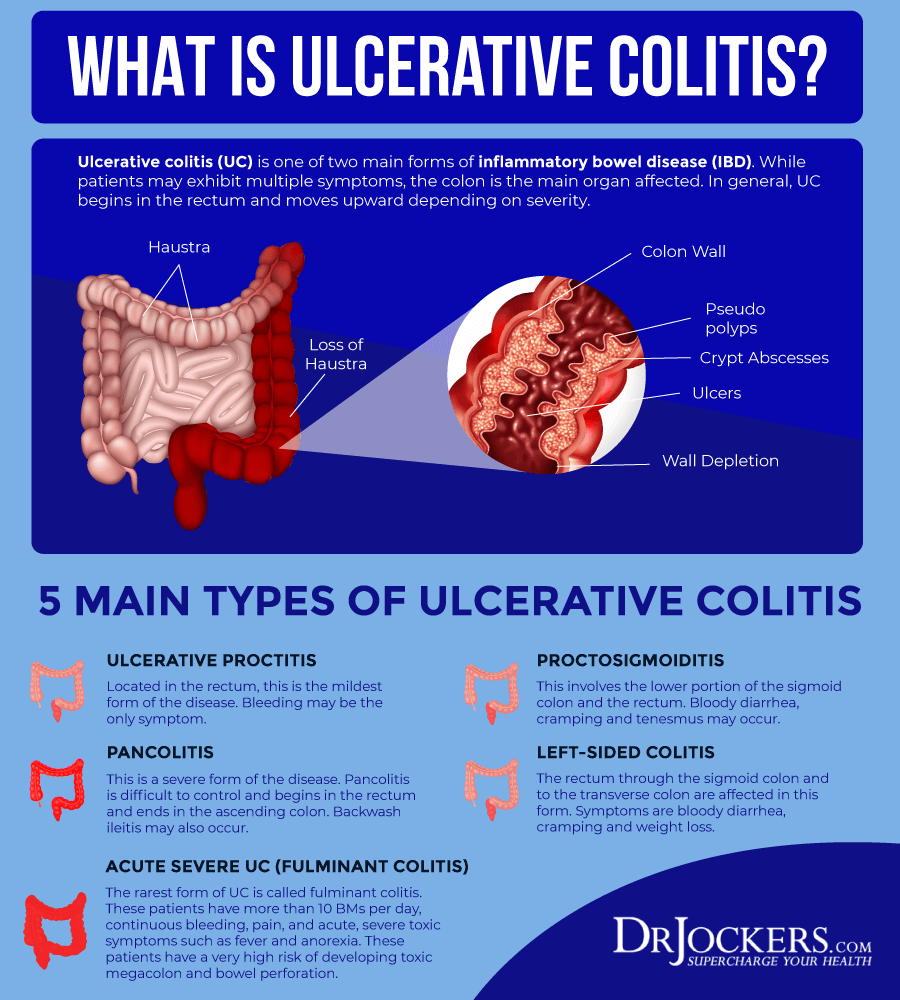
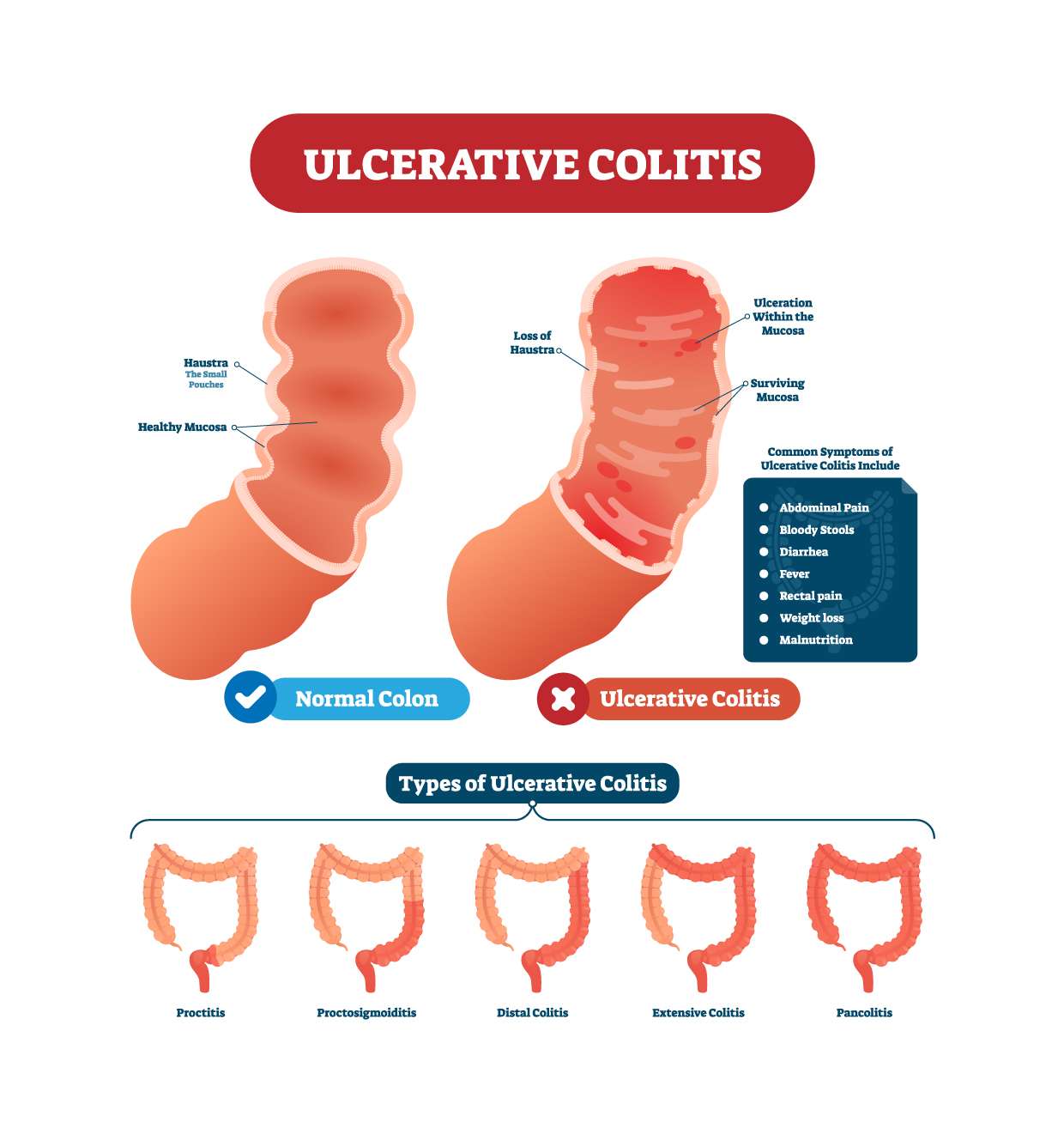
Healthcare providers classify ulcerative colitis by the area of irritation and how far it spreads. Most symptoms overlap between types, but a couple of unique characteristics exist.
- Ulcerative proctitis: Inflammation in the rectum where rectal bleeding is sometimes the only symptom
- Proctosigmoiditis: Irritation in the rectum and sigmoid colon .
- Left-sided colitis: The inflammation extends up the color to the left side of the body around the spleen. Abdominal pain is on the left side.
- Pancolitis: Inflammationinthe whole colon
You Could Develop Toxic Megacolon
If ulcerative colitis remains untreated, the inflammation can spread to the deeper layers of your colon and result in a very dangerous complication called toxic megacolon. This condition can lead to life-threatening infections, kidney failure, or a colon rupture and needs to be treated immediately.
At this point, there is really no other option for medical treatment than surgery, Bonthala says. Surgery for toxic megacolon typically involves removing all or part of your colon.
Don’t Miss: Stage 2 Pressure Ulcer Treatment Dressing
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, persons with ulcerative proctitis generally do not have nutrient deficiencies however, other factors may influence an individuals nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, then modifications to the diet will be necessary to compensate for this.
Better overall nutrition provides the body with the means to heal itself. It is important to follow Canadas FoodGuide, but some foods may irritate the rectum and increase symptoms, even though they do not affect the disease course. The customized recommendations of a registered dietitian can address your sensitive digestive tract.
Also Check: How To Soothe Mouth Ulcers
Treatment Of Ulcerative Colitis
Vedolizumab is a drug for people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The most serious side effect it causes is increased susceptibility to infection. Vedolizumab has a theoretical risk of a serious brain infection called progressive multifocal leukoencephalopathy Progressive Multifocal Leukoencephalopathy Progressive multifocal leukoencephalopathy is a rare infection of the brain that is caused by the JC virus. People with a weakened immune system are most likely to get the… read more because this infection has been reported with the use of a related drug called natalizumab.
Ustekinumab is another kind of biologic agent given to people who have moderate to severe ulcerative colitis that has not responded to TNF inhibitors or other immunomodulating drugs or who are unable to tolerate these drugs. The first dose is given by vein and then by injections under the skin every 8 weeks. Side effects include injection site reactions , cold-like symptoms, chills, and headache.
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Don’t Miss: What To Eat To Heal An Ulcer
Overview Of Ulcerative Colitis
While it can be overwhelming to receive a chronic disease diagnosis, learning all you can about ulcerative colitis will prepare you to manage your symptoms and live a full life.
Have you or a loved one been recently diagnosed with ulcerative colitis? Or were you diagnosed years ago but still dont fully understand your disease? Check out our latest video chat to learn more.
Video Length00:38:13
Video Chat: Ulcerative Colitis 101
Ulcerative colitis is a chronic inflammatory disease of the large intestine, also called the colon, that affects the lining of the colon and causes small sores, or ulcers, to form.
Those ulcers produce pus and mucous, which cause abdominal pain and the need to frequently empty your colon.
Video Length00:06:55
Ulcerative Colitis 101 This introductory video provides information on potential causes, symptoms, treatment and overall management of ulcerative colitis.
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
Recommended Reading: Good Foods To Eat When You Have An Ulcer
Your Immune System May Suffer
Inflammation can put constant stress on your body, which makes you vulnerable to infections and other illnesses. Your body is putting in so much energy to try to keep the inflammation under control that it really doesnt allow your body to do the normal housekeeping things its supposed to do, Bonthala explains. So people have a harder time fighting off illnesses and are more susceptible to catching other infections.
Does Ulcerative Colitis Affect Your Cancer Risk
Having ulcerative colitis doesnt mean you will get colorectal cancer, but it does increase your risk.
Ulcerative colitis is a chronic inflammatory bowel disease that affects the lining of the rectum and colon. It can be limited to the rectum or extend throughout the colon. Ulcerative colitis that affects the entire colon is called pancolitis.
The most common symptoms of ulcerative colitis are diarrhea and blood in your stool. Some patients may have abdominal pain. In severe cases, it can cause fever. Experts arent sure what causes the disease.
We talked to Yinghong Wang, M.D., about the link between ulcerative colitis, cancer and cancer treatment.
How does ulcerative colitis affect cancer risk?
If you have ulcerative colitis, your immune system recognizes the lining of your colon as a foreign body and attacks it. Over time, this damages the colon. As your body tries to repair the damage, the inflammation and constant cell replacement can result in a mutation that leads to cancer.
The more extensive your colitis and the longer you have it, the greater your risk of colorectal cancer. Males are at higher risk. And if you have both primary sclerosing cholangitis, which is inflammation of the bile duct, that puts you at even greater risk for colorectal cancer.
What should I do to reduce my cancer risk if I have ulcerative colitis?
Surgery is a cure. Because your colon is gone, the disease is gone, too.
What should cancer patients with ulcerative colitis know?
Recommended Reading: Best Supplements For Ulcerative Colitis
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your . Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Two Novel Jak Inhibitors Show Promise In Ulcerative Colitis
Megan Brooks
Patients with moderate to severe active ulcerative colitis who received induction therapy with either ritlecitinib or brepocitinib showed significant improvement across multiple outcome metrics in a phase 2b “umbrella” study of the two investigational agents.
The study by William J. Sandborn, MD, Division of Gastroenterology, University of California, San Diego, and colleagues was in Clinical Gastroenterology and Hepatology.
Ritlecitinib is a dual inhibitor that selectively inhibits Janus kinase 3 and the TEC family of tyrosine kinases, while brepocitinib is a dual tyrosine kinase 2 and JAK1 inhibitor.
Both agents have demonstrated efficacy and acceptable safety in the treatment of alopecia areata and rheumatoid arthritis and are being evaluated for treating vitiligo, Crohn’s disease, and UC.
The different JAK selectivity profiles of ritlecitinib and brepocitinib , compared with other JAK inhibitors, could further the understanding of the role these pathways play in UC, the investigators note.
You May Like: What Do You Do For A Bleeding Ulcer
Poor Growth And Development
Ulcerative colitis, and some of the treatments for it, can affect growth and delay puberty.
Children and young people with ulcerative colitis should have their height and body weight measured regularly by healthcare professionals.
This should be checked against average measurements for their age.
If there are problems with your child’s growth or development, they may be referred to a paediatrician .
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Also Check: How Do I Find Out If I Have An Ulcer