Can You Have Normal Faecal Calprotectin Levels But Still Have Ibd
Yes. Increased levels of faecal calprotectin are associated with lower gastrointestinal inflammation . If your levels come back normal you could still have Crohns disease in the upper part of your gastrointestinal tract or you could currently be in clinical remission from Crohns disease or ulcerative colitis in your lower gastrointestinal tract meaning there is currently no active inflammation in your intestines. You may have another condition which could be causing your bowel symptoms .
IBD is a chronic life-long condition which cannot currently be cured. If you have previously been diagnosed with IBD but your faecal calprotectin levels are below normal then it is likely you are in remission and have not been cured.
Can It Cure Uc
Fecal treatments have not been proven to cure UC, but research has shown they may help put the disease into remission for some people. Remission occurs when UC symptoms get better or go away completely for a period of time, such as weeks, months, or even years.
However, further study is needed to learn how long remission from UC may last after a fecal transplant. These procedures are not currently used to treat UC outside use in clinical trials.
Theres no cure for UC, but there are many methods that can help manage the condition and reduce flares, including:
- taking medications, like corticosteroids, biologic drugs, and immunomodulators
- using natural remedies, such as probiotics
- maintaining a diet, especially avoiding foods that trigger flares
- reducing stress levels
- exploring surgery to remove the colon
Talk with a doctor to learn more about treatment options for UC.
Tips For Healthy Ulcerative Colitis Poop
There are several different approaches to UC treatment. Medications, diet, and other lifestyle changes can all help improve bowel symptoms in UC.
The foremost treatment for ulcerative colitis inflammation and related stool changes is medication. These include:
- Aminosalicylates such as Asacol or Azulfidine , to reduce inflammation
- Corticosteroids such as prednisone and Entocort EC , to reduce inflammation
- Immunomodulators such as Imuran or cyclosporine, to reduce your immune system response
- Biologic therapies such as Remicade or Simponi , to neutralize proteins made by the immune system and reduce inflammation
Your diet also plays a role in your bowel habits. After all, what goes in, must go through and come out. The following diet modifications may help reduce bowel symptoms:
- Avoid your individual trigger foods.
- Limit dairy products.
- Drink plenty of water throughout the day.
- Eat small meals.
Stress is another factor that can contribute to changes in the stool. The brain-gut connection may play a role in inflammation of the GI tract. Managing your stress levels might be able to decrease diarrhea and other changes in your stool.
In addition, participating in regular physical activity is healthy for the GI tract. Exercise helps with the movement of stools, which can be especially helpful for constipation.
Also Check: What Are The Symptoms Of Having A Stomach Ulcer
How Are Stool Tests For Ibd Done
Your doctor or nurse will give you instructions as to how to collect your sample and these should be followed if they differ from the instructions below:
You will probably be provided with a specimen pot to put the stool sample into. If you arent then any clean, dry, screw top container will do.
Make sure the pot or container is labelled with your name, date of birth and the date you are taking the sample.
When collecting the sample try not to let it touch the toilet or toilet water and try not to collect any urine with it. To do this make sure you urinate first. To get the stool sample you could use a potty or a large, empty container to go to the toilet in or place plastic wrap or newspaper over the rim of the toilet seat to catch the stool.
You will then need to use a spoon or spatula to collect a piece of the stool. You should fill the sample pot about a third full – or collect a sample about the same size as a walnut if you are using your own pot.
After collecting the sample make sure you dispose of anything that you used to collect the sample by tying it in a plastic bag and putting in the bin. Make sure you wash your hands thoroughly afterwards. If you have an infection and you dont do this you could pass it on to other people.
Screening Of Pediatric Ibd Stool Using An Aptamer
An overview of the study flow is depicted in Fig. . For the initial aptamer-based screen of stool proteins, 24 stool samples were interrogated for 1129 proteins, as detailed in the methods section. Of the 1129 proteins assayed using the aptamer-based screen, significant upregulation of multiple proteins was seen in IBD stool compared to healthy controls, as shown in the volcano plot . Of the proteins that were significantly elevated in IBD vs HC, 48 stool proteins were found to be elevated in both CD and UC stool when compared to healthy control stool . Of these 48 stool proteins, only 3 survived multiple testing corrections , presumably because of the small sample size. Two proteins were elevated in the stool of CD patients but not UC when compared to healthy controls, while 18 proteins were elevated in the stool of UC patients when compared to healthy controls while not being elevated in CD stools compared to the healthy controls .
Fig. 1: An overview of the study showing the discovery of panels of stool proteins arising from an initial aptamer-based screen.Fig. 2: Aptamer-based screening of pediatric IBD stool samples for 1129 proteins.
Read Also: Early Stages Of Ulcerative Colitis
How Long Does It Take For A Stool Transplant To Work
In clinical trials and early studies, fecal transplants helped some people with UC have fewer symptoms or even achieve remission in 4 to 8 weeks. However, this research often involved a small sample size, so more study is needed on how long it takes before a stool transplant works for UC in larger groups of people.
When used to treat C. diff, stool transplants offer results within a few hours or days, according to NYU Langone Health.
Research on stool transplants for UC is still in the early stages, and even though some studies have shown promising results, further study is needed to determine whether this is a safe, effective treatment option for the condition.
In general, fecal transplant is considered to be a when donors and samples undergo thorough screening. The most common side effects of the therapy include:
Daisys Story: Symptoms And Medical History
I was 16 years old when I first noticed symptoms that I later found out were due to ulcerative colitis. The first symptom I noticed was severe fatigue, but I put this down to the exams I was taking at the time. I was also noticing abdominal pain more frequent bowel movements, and I was also passing blood. I noticed mucus in my stools and was experiencing frequent bouts of diarrhea.
At first, doctors thought that my symptoms were happening because of hemorrhoids, a stomach bug, parasite, or possibly a small tear. As my exams finished and my stress levels decreased, my symptoms became less noticeable too. However, they still persisted, and I was admitted to the hospital when I began to lose weight after not being able to eat drink.
When the doctors asked my mother and me about my family history, we explained that bowel cancer had affected some family members in the past. The doctors then ordered some blood and stool tests to investigate further.
Also Check: Best Mattress For Pressure Ulcers
Stool Test Is Useful Before Gps Refer For Possible Inflammatory Bowel Disease
This is a plain English summary of an original research article
A stool test by GPs has been shown to support referral decisions for young adults, not suspected of cancer, to investigate possible inflammatory bowel disease . This study supports current NICE guidelines that the calprotectin stool test can usefully inform patient referral pathways and reduce unnecessary invasive tests such as colonoscopy.
High levels of faecal calprotectin are associated with gut inflammation, as occurs in IBD and other organic intestinal diseases low levels are associated with functional bowel disorders, requiring different management.
In this cohort study, 789 adults aged 18-46 with gastrointestinal symptoms suggestive of either IBD or functional bowel disorders, and who had calprotectin tests to inform GP referral decisions, were followed for a year to assess diagnostic investigations and outcomes. Of patients with a negative calprotectin test, 99% did not have IBD.
Used as a decision aid, the test result influenced referral decisions for 45% of patients tested: it helped to avoid referral for 40% and led to referral for an additional 5%.
What Does Having Positive Calprotectin Mean
Patient
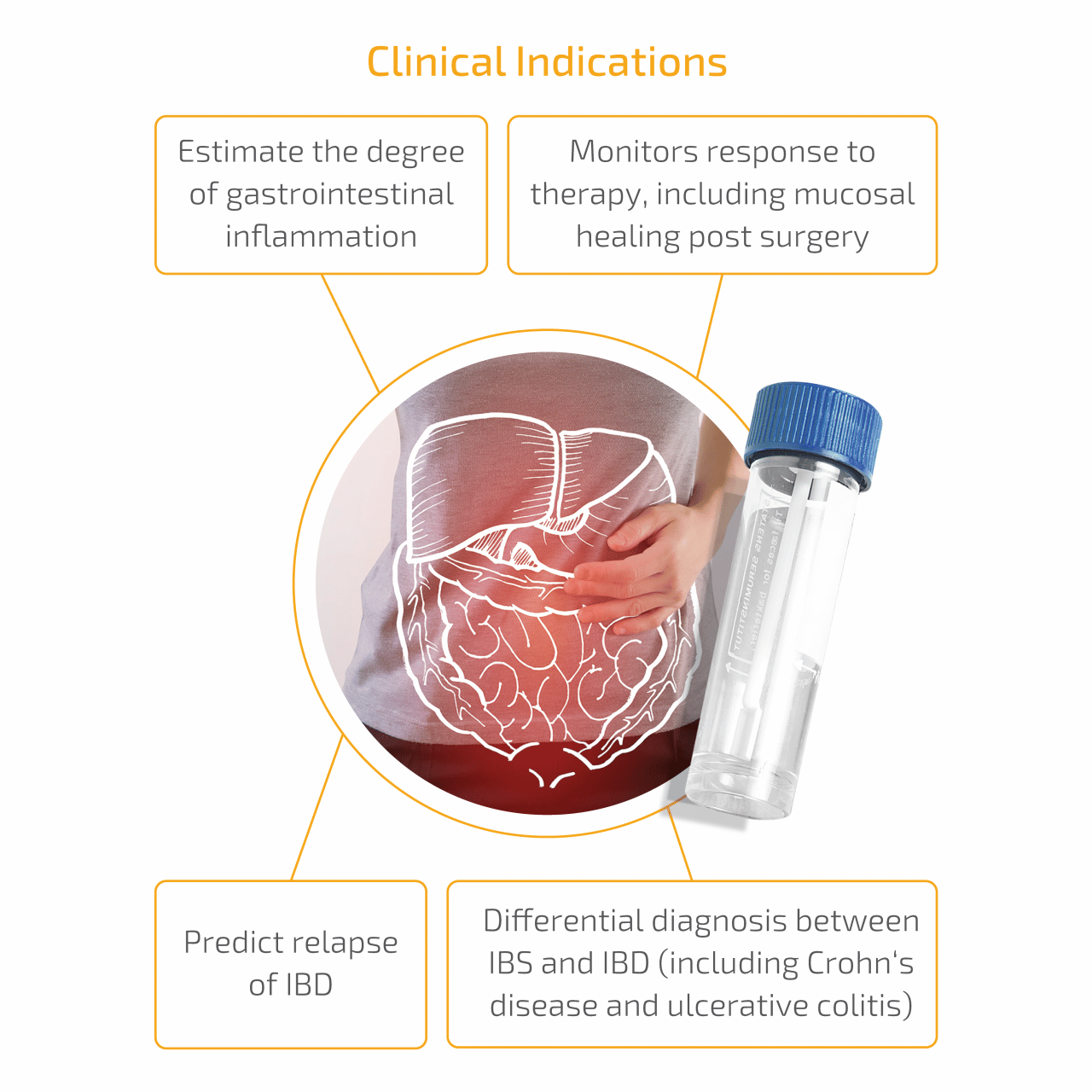
Fecal calprotectin 1 is a protein found in leucocytes, and it appears in the intestinal mucosa when there is inflammation. It can be detected in the stool. If a patients test results show positive calprotectin, it means that there is intestinal inflammatory activity. This biomarker allows assessing that activity in an easy, fast and non-invasive way.
The FC varies its presence levels in the organism depending on the age. Newborns have elevated levels, but it decreases from the first week of life to the age of 5, when they are equal to those of an adult.
It is very useful to diagnose the inflammatory bowel disease , as well as to evaluate the response to the treatment and to see what course ulcerative colitis or Crohns disease take. As the positive calprotectin means that there is activity, the subsequent fall of it means the treatment is working well.
In order to detect fecal calprotectin, just take a stool sample and put it in a container. It is a normal collection that does not require any particular care. It is the same process as for a routine urine test it is advisable to take the sample with the first deposition of the day. It can be stored for three days maximum before taking it to the corresponding specialist for it to be analyzed.
Positive calprotectin: diagnose for an IBD
Positive calprotectin, valid to predict relapse
Positive calprotectin: diagnose for an IBD
Positive calprotectin, valid to predict relapse
Positive calprotectin in the IBD monitoring
Recommended Reading: What Are The 4 Stages Of Pressure Ulcers
What Are Common Tests For Ulcerative Colitis
Blood Tests
Even though blood tests alone cant diagnose ulcerative colitis, theyre an important tool in diagnosis and monitoring of the disease. These are only some of the blood tests used for UC. There are others your doctor may recommend.
These are used to detect infection, anemia , indicators of inflammation, and to identify deficiencies of vitamins or minerals.
Samples of stool may be tested for pathogenic bacteria and certain markers of inflammation. Your doctor will give you a container for collecting and storing the stool.
Imaging Tests
These are tests that take pictures of different parts of your body to provide a clearer view of your condition. They show your doctor areas of disease activity and possible complications. These are only some of the imaging tests used for UC. There are others your doctor may recommend.
A standard X-ray of your abdominal area can show narrowing, widening, or development of a perforation of the intestines or an intestinal blockagepossibly from inflammation or scarring. It may also be done to rule out certain UC complications.
This diagnostic test allows your doctor to evaluate your intestine by tracking the movement of a thick, chalky liquid called barium. The barium dye coats the lining of the bowelcreating a silhouette of your rectum, colon, and a portion of your intestine thats visible on an X-ray.
Biomarker Tests
Ways Biomarkers Can Help With UC Monitoring
Digestive Changes In Ulcerative Colitis
Ulcerative colitis is a chronic condition, meaning it comes on slowly over a long period of time. Currently, there is no known cure for UC.
With UC, inflammation and ulcers develop on the lining of the large intestine . Sometimes the rectum is affected, as well.
This inflammation can cause changes in bowel habits, including urgency, diarrhea, blood or mucus in the stool, and abdominal pain. When your large intestine is inflamed, it contracts and empties often, which is why you may have urgent bowel movements and diarrhea.
When chronic inflammation damages the lining of your colon, ulcers can develop. The ulcers can bleed, leading to blood in your stool. If you regularly lose a lot of blood in your stool, you might develop anemia .
Though diarrhea is more common, some people with UC experience constipation. Inflammation limited to the rectum, known as ulcerative proctitis, may result in constipation.
Other symptoms of UC include painful bowel movements, nausea, vomiting, fatigue, unintentional weight loss, and fever.
Read Also: Peptic Ulcer Food To Eat
Faecal Calprotectin Tests: The Ultimate Patient Guide
Want to learn more about testing for faecal calprotectin? Youve come to the right place.
This article explains what faecal calprotectin is, why you might want to know your faecal calprotectin level, and how you go about testing it. For a general introduction to faecal calprotectin, head over to Faecal Calprotectin Made Easy .
Endoscopy Of The Large Intestine
Doctors order endoscopy of the large intestine with biopsies to diagnose ulcerative colitis and rule out other digestive conditions. Doctors also use endoscopy to find out how severe ulcerative colitis is and how much of the large intestine is affected.
During an endoscopy, doctors use an endoscopea long, flexible, narrow tube with a light and a tiny camera on one endto view the lining of the large intestine. Doctors obtain biopsies by passing an instrument through the endoscope to take small pieces of tissue from the lining of your rectum and colon. A pathologist will examine the tissue under a microscope.
Two types of endoscopy used to diagnose ulcerative colitis are
- colonoscopy, in which a doctor uses a type of endoscope called a colonoscope to view the lining of your rectum and your entire colon
- flexible sigmoidoscopy, in which a doctor uses a type of endoscope called a sigmoidoscope to view the lining of your rectum and lower colon
Recommended Reading: Can Alcohol Cause Bleeding Ulcers
Daisys Story: Treatment First Steps
Once I had received a diagnosis, doctors suggested I try enemas and taking medications such as oral steroids. These can be very effective for ulcerative colitis, but, at first, I did not notice much of a change in my symptoms. However, as I understood the condition better, I realized the most powerful treatment was actually to combine the medication with lifestyle changes.
I researched different diets to try and kept a food diary to understand which foods caused my symptoms to worsen. I found information on the specific carbohydrate diet and gradually removed gluten and dairy from my diet as I identified them as trigger foods.
I did find that some dietary changes improved symptoms at first and then worsened them over time. This is why it was very important that I followed diets strictly and worked with doctors to understand the best course of treatment for me.
The specific carbohydrate diet involves cutting out foods that contain disaccharides and most polysaccharides, such as grains, milk products, and most sugars. A person can include foods that contain monosaccharides, such as fruits, nuts, non-starchy vegetables, meat, and fish.
Daisys Story: Blood Tests
My symptoms worsened as I went through various tests to work out their cause. One of the first tests was a blood test, which doctors ordered when they believed my symptoms were happening due to a parasite. When the results came back, the doctors told me I had clear signs of inflammation.
I began taking some medications to ease my symptoms, and after these blood test results came back, the doctors referred me for further tests.
Read Also: What Can I Do For A Stomach Ulcer
White Blood Cell Count
White blood cells are key components of your immune system. They not only target and neutralize disease-causing microorganisms but “learn” to identify specific pathogens so they can launch a targeted assault should that pathogen return.
White blood cells , also known as leukocytes, are comprised of various types of cells, each with its specific purpose. They include granulocytes , monocytes, and lymphocytes .
A white blood cell count is a panel of tests that measures each of these cell types. Elevations of WBC is generally a sign of an infection or inflammation. A healthcare provider can begin to investigate the most likely causes of the inflammation or infection based on which cells are elevated.
White blood cell counts are important because many of the drugs used to treat IBD are immunosuppressive, meaning that they blunt the immune system’s response to disease. If the WBC is too low, a person may be at a high risk of infection.
Daisys Story: Tips For Others
- Stay informed: Online resources from reputable sources can help a person understand ulcerative colitis better. It can help them prepare for test and appointments and may give them ideas of important questions to ask a doctor.
- Be open: Maintaining an honest and open line of communication with a doctor can speed up the diagnostic process. Do not dismiss the idea of lifestyle changes, which can make an enormous difference to symptoms, but be sure to follow the treatment advice doctors have given. Equally, make sure to tell a doctor in detail if a treatment does not seem to be working.
- Feel empowered: People should remember that their health condition does not define them. Some people find discussing bowel habits and colonoscopies embarrassing, and I definitely relate to that. However, it is important to remember that these are natural bodily processes and tests, and being open and honest can make a huge difference in managing symptoms successfully. It is important to make an invisible condition visible in this way.
- Stay mindful: Stress has always been a trigger for my symptoms, and the diagnosis process alone can be stressful. Try to make mindful activities part of the daily routine. This can help people learn to manage symptoms even after a flare-up has passed.
- Seek support: Several great support groups exist for people with ulcerative colitis. It can be helpful to know you are not alone and to learn more about current research and topics within this community.
Don’t Miss: 5 Asa Drugs Ulcerative Colitis