Clinical Management Of Uc Patients In Surveillance Program
Histological interpretation of surveillance biopsies plays an essential role in clinical management. There is unanimous agreement in the literature that the detection of flat HGD or a DALM with any degree of dysplasia carries a sufficiently high risk of prevalent CRC or short-term and high-risk progression to CRC to warrant immediate colectomy . The natural history of LGD is more controversial but, in two studies, LGD was associated with a 20% risk of prevalent CRC in patients who underwent immediate colectomy or colectomy within 6 months and 14.519.4% risk of progressing to CRC in patients who continued on surveillance alone . While outcome data are scarce for UC with changes indefinite for dysplasia, this diagnosis is associated with significant risk of prevalent HGD and significant progression rates to dysplasia and advanced neoplasia , suggesting that UC patients with this finding warrant close follow-up.
Conflict of interest: none declared.
Rectal Sparing In Colectomy Specimens
UC classically involves the rectum, particularly in adult patients. Rectal sparing is seen in about 32% of cases by endoscopic examination and 30% by histological examination of biopsy specimens . However, in colectomy specimens, only 5.4% of cases showed rectal sparing and all of these were considered relative’ . These findings suggest that rectal sparing on biopsy material should not be interpreted as definite evidence of Crohns disease, and that assessment of colectomy specimens provides more accurate information on the status of the rectum.
Complementary And Alternative Medicine
Probiotics may modestly reduce disease activity in active disease, but do not increase remission rates.34 However, Lactobacillus GG and Escherichia coli Nissle 1917 have been shown to be as effective as 5-ASA for maintenance therapy.16,17 Acupuncture has shown a small symptomatic benefit in active disease.35 Wheatgrass has also shown some effectiveness in reducing symptoms of active disease.36
Read Also: What Are The Symptoms Of An Ulcer In A Child
Management Of Acute Severe Ulcerative Colitis
- The presence of both of the following indicates acute severe ulcerative colitis :
- ⥠6 bowel movements daily
- ⥠1 sign of systemic toxicity
Neither total parenteral nutrition nor empiric antibiotics are routinely indicated in ASUC.
Classification Of Ulcerative Colitis By Severity
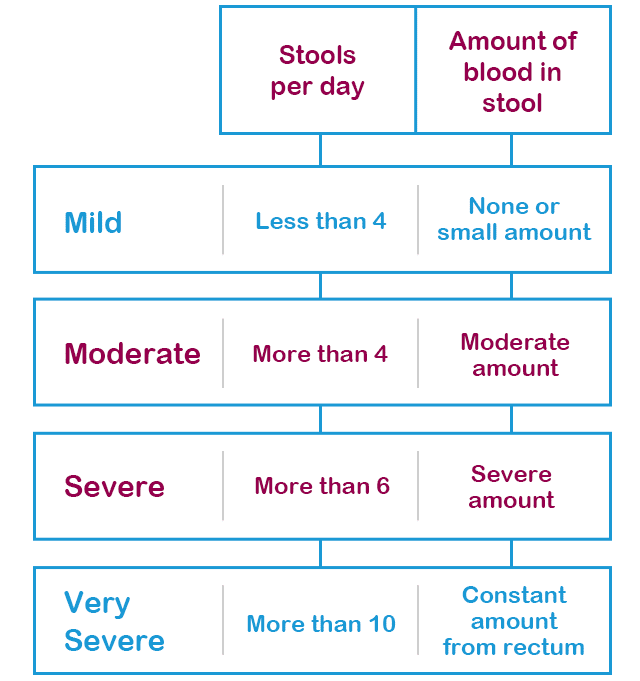
There are several classification systems that can be used to assess disease severity. Criteria include:
- Endoscopic findings
| American College of Gastroenterology ulcerative colitis activity index | |
|---|---|
| Criteria | |
| Frequency of blood in stool | Intermittent |
| Truelove and Witts severity index | |
|---|---|
| Criteria | |
| Amount of blood in stool | Small amount |
| ⤠30 mm/hour | > 30 mm/hour |
Treatment recommendations by the ACG are based on the ACG ulcerative colitis activity index, while recommendations by the American Gastroenterological Association are based on a combination of the Truelove and Witts severity index and the Mayo score for ulcerative colitis activity. There is significant overlap among the criteria used in all ulcerative colitis severity indices.
Also Check: How To Ease A Stomach Ulcer
Indeterminate Colitis In Colectomy Specimens
When indeterminate colitis is defined by the pathological findings in the resected colon as originally suggested, with features overlapping between UC and Crohn’s disease, the incidence of pouch complications will lie between UC and Crohn’s disease. However, if indeterminate colitis is defined as colitis showing features not classic for either UC or Crohn’s disease, the incidence of complications and pouch failure will not differ from those in UC . Regardless of the exact definition of indeterminate colitis, if there are no pathological stigmata of Crohns disease in the biopsy and colectomy, or clinical evidence of Crohn’s disease, patients with indeterminate colitis should not be denied an IPAA procedure .
Endoscopy Of The Large Intestine
Doctors order endoscopy of the large intestine with biopsies to diagnose ulcerative colitis and rule out other digestive conditions. Doctors also use endoscopy to find out how severe ulcerative colitis is and how much of the large intestine is affected.
During an endoscopy, doctors use an endoscopea long, flexible, narrow tube with a light and a tiny camera on one endto view the lining of the large intestine. Doctors obtain biopsies by passing an instrument through the endoscope to take small pieces of tissue from the lining of your rectum and colon. A pathologist will examine the tissue under a microscope.
Two types of endoscopy used to diagnose ulcerative colitis are
- colonoscopy, in which a doctor uses a type of endoscope called a colonoscope to view the lining of your rectum and your entire colon
- flexible sigmoidoscopy, in which a doctor uses a type of endoscope called a sigmoidoscope to view the lining of your rectum and lower colon
Recommended Reading: Ulcerative Colitis Joint Pain Treatment
Difficulties In Diagnosis Of Uc
As UC-associated dysplasia may occur in endoscopically normal mucosa, extensive biopsy sampling is necessary to confidently exclude the possibility of dysplasia. In order to exclude dysplasia with 90% confidence, a minimum of 33 well-oriented jumbo forceps biopsies are required 56 such biopsies are required to achieve a 95% level of confidence . This is the rationale for surveillance programs including periodic colonoscopic examination with protocol biopsies to detect dysplasia, which has now become the standard of care for surveillance in IBD patients .
In addition to sampling error, histological evaluation of dysplasia suffers from problems of diagnostic reproducibility. Few studies have evaluated inter-observer agreement in the diagnosis of UC-associated dysplasia , none of which assessed inter-observer agreement in the context of clinical outcome, the ultimate standard of diagnosis.
Referral And Differential Diagnosis Of Ibd
Joseph Feuerstein, MD: Dr Ungaro, could you fill us in on how you make the diagnosis for ulcerative colitis and Crohns disease when thinking of these 2 disease processes?
Ryan Ungaro, MD: Sure. Thanks, Joe. Its great to be here. With both diseases, theres a broad differential diagnosis when youre seeing a patient where theyre presenting with symptoms that can be mistaken for different etiologies. You can have a patient with diarrhea, bloody stool, and abdominal pain, which can be symptoms for multiple diseases. The first thing to consider in a patient presenting with bloody diarrhea or diarrhea and abdominal pain is infection and looking at different infectious causes of the symptoms. Thats always an IBD trigger. Its important to rule out infectionstandard stool tests are something to consideras well as tuberculosis if you have someone coming from a developing area of the world. Considering infection in your differential is always important. Getting stool studies to understand if theres an infectious etiology to the patients symptoms is very important.
Joseph Feuerstein, MD: Thank you, Ryan and Steve. That was a phenomenal explanation. Bruce, is there any use of any biomarkers or noninvasive tests assisting the diagnosis of ulcerative colitis or Crohns disease?
Transcript edited for clarity.
Don’t Miss: Ulcerative Colitis Blood In Urine
Features Of Treated Uc
In the setting of medically treated UC, endoscopically or histologically discontinuous disease may be observed as a result of uneven healing . The same process may also lead to absolute or relative rectal sparing. As patchiness of disease and rectal sparing mimic Crohn’s disease and are commonly seen in treated UC, evaluation of disease distribution to sub-type IBD should not be attempted in this setting rather, efforts should be directed toward identifying granulomas, superimposed infection, and dysplasia.
Establishment Of A Differential Diagnosis Scoring Model For Cd And Upil
The differential diagnostic scoring model for CD and UPIL was ultimately established based on the logistic regression model of clinical symptoms combined with endoscopic and imaging features. According to the previous multivariate analysis, we got the scores of each variable using the method shown in the statistical analysis subsection . A patient was diagnosed with CD if the total score was 1 otherwise, he or she was diagnosed with UPIL. The accuracy of the differential diagnosis using this model was as high as 83.66%. The calibration plot also demonstrated the good performance of this score model .
Figure 4 Calibration curve for predicting the possibility of CD. The calibration plot also demonstrated good performance of this score model.
Read Also: Venous Stasis Ulcer Wound Care
Immunohistochemical Analysis Of Retinoblastoma And
-
Affiliation Instituto de Ciências Biomédicas, Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
-
Affiliation Instituto de Ciências Biomédicas, Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
-
Affiliation Instituto de Ciências Biomédicas, Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
-
Affiliation Instituto de Estudos de Saúde Coletiva , Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
Special Issues Of Dysplasia In Patients With Uc
Dysplasia identified in endoscopically apparent lesions in patients with UC
Clinical correlation with the extent of colitis and location and endoscopic appearance of the polyp are essential for proper classification. It cannot be over-emphasised that the endoscopic impression of resectability is the key factor in determining appropriate management for visible dysplastic lesions in UC, as it is extremely difficult, if not impossible, to distinguish these entities on the basis of histological features alone. In addition, biopsy of the mucosa surrounding the polyp and attention to the epithelium of the polyp stalk may be useful in determining appropriate management. Regardless of whether an endoscopically resectable lesion represents polypoid IBD-associated dysplasia or a sporadic adenoma, this distinction is of little consequence as in most cases these may be adequately managed with complete polypectomy and close endoscopic surveillance. On the other hand, endoscopically unresectable lesions pose a high risk for adenocarcinoma and are typically managed with colectomy.
Also Check: Ulcerative Colitis Causes And Treatment
Clinical Relevance: When The Differential Diagnosis Affects Clinical Management
During the last fifteen years, the development of biological therapies and a widespread use of immunomodulators have radically changed treatment strategy in IBD. Consistently, prognostic indexes focusing on the assessment of mucosal inflammation have become an important treatment goal predicting long-term outcomes in terms of disease progression, complications and steroid sparing. In this context, the issue of differential diagnosis has received renewed attention, because both medical and surgical treatments imply more and more disease-specific strategies.
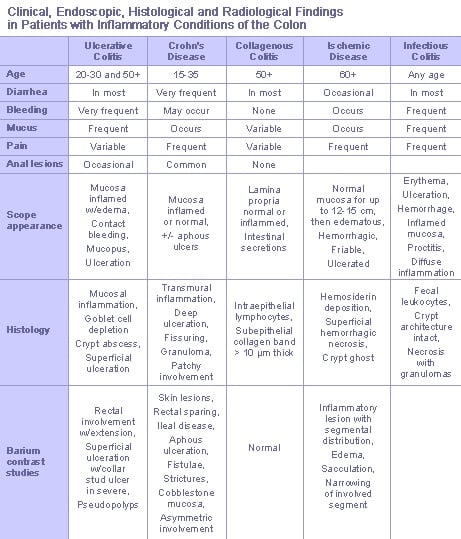
Differential Diagnosis: Current Approach
IBD colitis may present with a variety of unspecific features turning the differential diagnosis among UC, CD and IBDU into one of the greatest diagnostic challenges in gastroenterology. As stated above, no single gold standard is available for the diagnosis and the distinction of IBD. The diagnosis rests on a multidisciplinary work-up, based on clinical evaluation integrated with a combination of endoscopic, histological, radiological, and/or biochemical investigations .
Differential diagnosis in inflammatory bowel disease colitis.
Read Also: Medication For Ulcerative Colitis Flare Up
Disease Subtypes And Differential Diagnosis Of Uc And Cd
Miguel Regueiro, MD: Ellen, Im going to include you because David mentioned the differential diagnosis of IBD . But before I get to that, what are the subtypes of the different phenotypes of ulcerative colitis?
Ellen J. Scherl, MD:If you look at ulcerative colitis as part of a spectrumand we dont focus on the Crohn disease colonic phenotypewere talking about ulcerative proctitis left-sided disease or universal colitis , with separate phenotypes for ulcerative colitis. There are patients who look like classic ulcerative colitis, but over time they change to more of a Crohn phenotype, with either skip areas, perianal fistula, or even ileal disease.
The point is that we dont have a great molecular or cellular way of classifying these diseases. But in the April issue of Gastroenterology, which is devoted to the era of disease modification, they talk about the need to reclassify colitis-associated Crohn or colitis-associated ulcerative colitis, because Crohn colitis acts more like ulcerative colitis than ileal diseaserelated Crohn. Until we come to what Marcus Neurath has called reframing the inflammatory immune-mediated diseasesfrom target organs like colon vs ileum to more specific cytokine signatureswere left with this differential diagnosis: is it Crohn or ulcerative colitis?
Transcript Edited for Clarity
Infectious Colitis And Cord Colitis
Infectious colitisdue to a variety of agentsmay clinically mimic UC. However, most cases of infectious colitis demonstrate a histological pattern of acute colitis, which may be diffuse, patchy, or focal, without evidence of chronicity, as evidenced by architectural distortion . Less commonly, chronic infectious colitis may produce a histological pattern of chronic active colitis resembling IBD. Most cases of infectious colitis with the chronic active colitis pattern have no specific diagnostic features on histological examination in such cases, knowledge of the clinical history and correlation with serologic studies or stool cultures are required for diagnosis. However, an important exception is amoebic colitis, in which trophozoites of entamoeba histolytica may be observed in biopsy material showing features of chronic active colitis . Amoebae should always be excluded in biopsies of suspected IBD, as these organisms may not be identified by routine stool studies and because immunosuppressive therapy for presumed IBD may result in fulminant amoebic colitis with perforation .
Amoebic colitis may mimic ulcerative colitis by a manifestation of chronic active colitis with crypt distortion, mild basal lymphoplasmatocysis , and epithelial injury . However, trophozoites of entamoeba histolytica are evident on high magnification .
Don’t Miss: Foods To Eat With Peptic Ulcer Disease
Differential Diagnosis In Ulcerative Colitis In An Adolescent: Chronic Granulomatous Disease Needs Extra Attention
Correspondence to: Odul Egritas Gurkan, MD, Department of Pediatric Gastroenterology, Gazi University School of Medicine, Mevlana Boulevard, Besevler, 06510 Ankara, Turkey.
Telephone: +90-31-22024423 Fax: +90-31-22024423
The Diagnostic Value Of Different Indicators In Cd And Upil
To comparatively analyze the diagnostic value of clinical symptoms and various endoscopic and imaging indicators in CD and UPIL, we performed multivariate and ROC curve analyses of the clinical symptoms individually, clinical symptoms combined with endoscopic indicators, and clinical symptoms combined with endoscopic and imaging indicators to select the model with the best differential diagnostic power.
Table 6 Multivariate Analysis and Scores Based on Clinical Manifestations, Endoscopic, and Imaging Characteristics.
Figure 3 ROC curves based on different variables. The AUC for differentiating CD and UPIL based on clinical manifestations alone, combined clinical manifestations and endoscopic features, combined clinical manifestations, endoscopic, and imaging features was 0.726, 0.918, and 0.947, respectively.
Table 7 Comparisons among different indicators.
Therefore, including endoscopic and imaging indicators significantly improved the ability to differentiate between CD and UPIL.
Don’t Miss: What Is Good For Ulcer Pain
Features Of Classic Cases
In untreated disease, UC usually exhibits a histological pattern of chronic active colitis, which refers to the presence of active inflammation accompanied by features of chronic mucosal injury. Activity is defined as the presence of neutrophil-mediated epithelial injury, which may take the form of neutrophils infiltrating crypt epithelium , collections of neutrophils within crypt lumens , or by infiltration of surface epithelium with or without mucosal ulceration. Chronicity is defined by crypt architectural distortion, basal lymphoplasmacytosis, or Paneth cell metaplasia in the left colon. Architectural distortion is represented by shortening of the crypts and branching of the crypts . In normal mucosa, the crypts are uniformly spaced, arranged perpendicular to the muscularis mucosae, and the crypt bases contact the upper edge of the muscularis mucosae. Basal lymphoplasmacytosis refers to the presence of a lymphoplasmacytic infiltrate between crypt bases and the muscularis mucosae . While Paneth cells are a normal component of the right colon, their presence in the left colon is a metaplastic process, due to chronic crypt epithelial injury . Rarely, pyloric gland metaplasia may also be seen in UC . Microscopically, these changes of chronic active colitis are diffuse and uniform in distribution: that is, every biopsy fragment from the diseased colon shows a similar degree of injury and inflammation.
Ulcerative Colitis Versus Crohn Disease
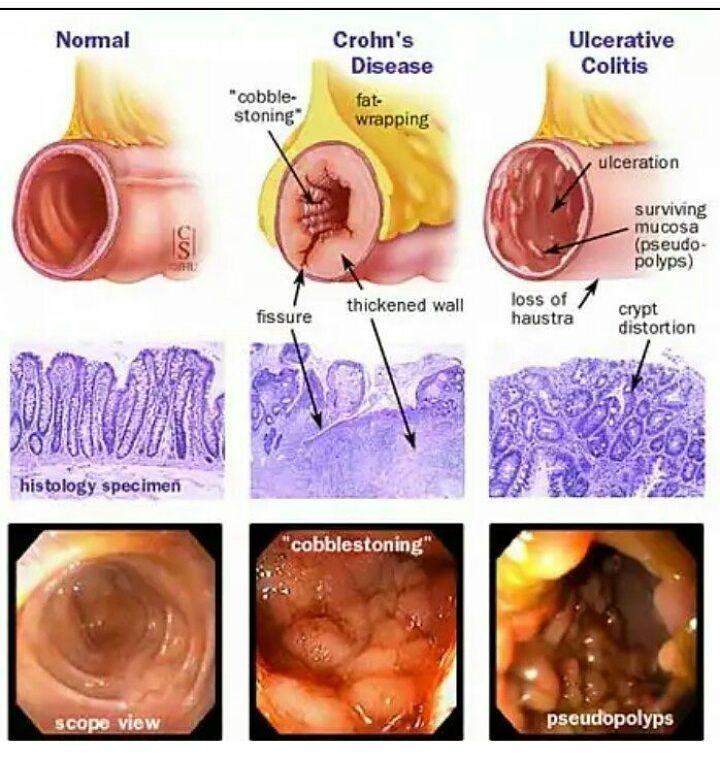
Grossly, Crohn disease is characteristically noncontiguous, with intervening, or skipped, areas of normal mucosa. The ulcerations in Crohn disease tend to be linear and often lead to the classic cobblestone appearance of the mucosa. Crohn disease may involve the entire gastrointestinal tract, whereas ulcerative colitis involves only the large bowel.
Microscopically, the inflammation in ulcerative colitis and Crohn disease can appear similar, but noncaseating granulomas are present only in Crohn disease therefore, their presence is specific for Crohn disease. The inflammation of Crohn disease may be transmural, whereas it is confined to the mucosa and submucosa in ulcerative colitis. Unfortunately, the differentiation is not always possible preoperatively. All large series of proctocolectomies include a subset of patients who were preoperatively thought to have ulcerative colitis but were subsequently diagnosed with Crohn disease.
References
Murata I, Satoh K, Yoshikawa I, Masumoto A, Sasaki E, Otsuki M. Recurrent subcutaneous abscess of the sternal region in ulcerative colitis. Am J Gastroenterol. 1999 Mar. 94:844-5. .
Kimura K, Hunter SF, Thollander MS, et al. Concurrence of inflammatory bowel disease and multiple sclerosis. Mayo Clin Proc. 2000 Aug. 75:802-6. .
Egan CA, Meadows KP, Zone JJ. Ulcerative colitis and immunobullous disease cured by colectomy. Arch Dermatol. 1999 Feb. 135:214-5. .
Wiesner W, Steinbrich W. . Ther Umsch. 2003 Mar. 60:137-44. .
You May Like: Foods That Help Ulcerative Colitis
Epithelium Positive For Dysplasia
This category is subdivided into low-grade dysplasia and high-grade dysplasia , based on the degree of architectural and cytological abnormalities , to imply the relative risk of a concurrent adenocarcinoma or progression to adenocarcinoma.
Positive for dysplasia: LGD
Most biopsy specimens of LGD have crypts lined by epithelium with enlarged and hyperchromatic nuclei. Nuclear stratification is present but typically confined to the basal half of the cells . The nuclei in LGD maintain normal polarity that is, their long axes are perpendicular to the basement membrane. Most cases of LGD do not exhibit surface nuclear maturation: in other words, atypical nuclear features should involve both crypt and surface epithelium .
Positive for dysplasia: HGD
In the originally proposed classification, the majority of HGD cases closely resemble adenomas in non-colitic patients with nuclear stratification extending to the superficial aspect of the epithelial cells. HGD exhibits enlarged nuclei with marked nuclear hyperchromasia, pleomorphism, and loss of nuclear polarity . In addition to these nuclear features, HGD may exhibit increased architectural complexity, which may manifest as crowded or cribriform glands or villiform/papillary surface configuration .