How Is Ibd Diagnosed
Your will have a complete physical exam. You may need some tests, such as blood tests, stool tests, CT or MRI scans, and colonoscopy with biopsy. The colonoscopy is to look for sores or inflammation in the intestine. Because most of the treatments for IBD have risks, you need to be completely sure that you have IBD before it is treated. Your intestinal tissue will be looked at very closely under a microscope to be sure you have IBD and not an infection or another illness.
Other Possible Causes Of Frequent Urination
Several other health conditions unrelated to UC could also lead to increased urination. They include:
- Bladder stones
- Prostate problems, including prostatitis or benign prostatic hyperplasia
- An overactive bladder
- Interstitial cystitis, also known as painful bladder syndrome
Needing to urinate more than usual is also a sign of diabetes. People with diabetes, which affects about 1 out of 10 Americans, may have high blood sugar levels that can damage tissues and organs. In addition to frequent urination, diabetes can also cause symptoms like increased thirst and hunger, blurry vision, extreme tiredness, and bruises and cuts that take a long time to heal.
Taking diuretics also leads to increased urination. These medications are used to treat heart failure and certain kidney and liver problems.
If The Kidney Stone Is Not Causing Any Symptoms Should I Still Be Treated
There are some instances when it is OK to leave a kidney stone untreated. If the stone is small and not causing any pain, there is a good chance that it will pass on its own after it falls into the ureter. Such stones may be followed with “watchful waiting.” This means that the stone is not actively treated, but instead your doctor keeps a check on the stone to be sure that it is not growing or changing. This can be done with periodic X-rays.
You May Like: What Do I Take For An Ulcer
Blood In Stool And Crohns Disease
Bleeding in Crohns disease can vary depending on the location of inflammation. If it takes place in the colon or rectum, there will be more blood present in stools.
Blood loss in Crohns disease may be due to anal fissures that develops as a complication of Crohns disease. The good news is, anal fissures can be successfully treated without surgery.
What About Vitamins And Minerals
It is a good idea for all people with IBD to take a standard multivitamin every day. People with IBD who are doing well do not need any extra vitamins or minerals. If you have Crohns disease is in the ileum or the ileum has been removed you may need to take B12, calcium, or vitamin D. You may need iron supplements if you have blood loss during inflammation or reduced iron absorption as a result of inflammation. Diarrhea or vomiting can cause loss of potassium and magnesium. If you are lactose intolerant and avoid dairy products, this can lead to low calcium. Ask your doctor if you need to be tested for any of the above.
You May Like: Food Not Good For Stomach Ulcer
Also Check: Natural Treatment Of Ulcer In Hindi
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
- cramps
- diarrhea
- fatigue
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Crohns disease may affect any part of the GI tract, from the mouth to the anus. Its most often found in the small intestine. UC only affects the large intestine and rectum.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Ulcerative Colitis And Colon Cancer
Your risk for colon cancer goes up if you have UC. It depends on how much of your colon is involved and how serious it is. The odds also rise after youve had UC for 8-10 years and they go up over time. Treatment that puts your UC in remission may also make cancer less likely. Colonoscopy screening helps doctors find colon cancer early, when its easier to treat.
- Use websites and cellphone apps to find restrooms in airports, train stations, or other large venues ahead of time.
- Carry extra underwear and wet wipes.
- Bring enough medication to last the entire trip, along with copies of your prescriptions.
- Tell your doctor about your plans to see if you need to take other precautions.
You May Like: Stomach Ulcer Pain Relief Medicine
Why Does Kidney Disease Cause Weight Gain
Kidney disease doesnt just affect the kidneys, it affects the whole body. In the early stages, it can cause weight loss, while in the later stages it can cause weight gain. These variations are the result of different aspects of the disease. Heres some information to help you understand the issue of kidney disease and weight gain, courtesy of Dr. Allen Lauer, of Associates in Nephrology.
You May Like: What To Do For A Kidney Infection
Risk Factors: Nsaids Age Physical Activity And Gender
In a study published in PLoS One,¹ intestinal surgery, extended use of nonsteroidal anti-inflammatory drugs , stenosis of the bowel, activity, and duration of disease, and diagnosis of Crohns disease may all be correlated with an increased risk of gallstones and kidney stones in patients with .
Using data from the Swiss Inflammatory Bowel Disease Cohort Study , an adult, population-based cohort in Canton of Vaud, Switzerland, the study included 2,323 patients with IBD. Of these, 55.4% reported having CD and 42.6% reported having ulcerative colitis.¹
“Among the subjects, 7.8% of patients with CD and IBD, and 3.8% of patients with UC and IBD were diagnosed with gallstones.¹ A multivariate analysis demonstrated that, in addition to a CD diagnosis, several other factors were correlated with the presence of gallstones in patients with IBD,” according to the authors. These included:¹
-
Extraintestinal manifestations of disease
-
Age at diagnosis
-
Duration of disease
-
History of intestinal surgery
-
NSAID usage
-
Disease activity .
Within this same cohort, 4.6% of patients with CD and 3.0% of patients with UC was diagnosed with kidney stones, said lead author, Stefania Fagagnini, Division of Gastroenterology and Hepatology at the University Hospital in Zurich, Switzerland. A multivariate analysis showed five significant risk factors for the development of kidney stones in patients with IBD.¹These included:
-
Level of disease activity
-
Prolonged use of NSAIDs
-
Being male .
You May Like: Diabetic Foot Ulcer Treatment Ointment
Medications For Ulcerative Colitis
The goal of medication is to control inflammation and heal the intestinal lining known as mucosal healing.
Medications used to treat ulcerative colitis include:
- Aminosalicylates, such as sulfasalazine and mesalamine , which reduce inflammation
- to treat bacterial infections
- Antidiarrheals to control diarrhea
- Biologic agents that can rapidly induce remission in patients with severe ulcerative colitis, defined as more than six bloody stool episodes daily
- Corticosteroids
- Immunomodulators that suppress the bodys immune response, such as azathioprine and 6-mercaptopurine
After beginning medication therapy, follow-up blood and stool tests for markers of disease activity, such as fecal calprotectin can help monitor the response to various therapies.
Uc Treatments And Urinary Changes
Sometimes, UC treatments can affect urinary habits. Corticosteroids such as prednisolone may cause urinary changes in people with UC. This medication usually causes someone to pee less, but it can also cause someone to pee more often.
Several members have noticed this effect. Has anybody ever experienced frequent, urgent urination whilst on prednisolone? asked one member. I am definitely peeing more often, but the urgency at which I need to get to the bathroom to have a pee is a bit worrying. Another member mentioned that they had experienced this effect. When I take prednisone or budesonide, I urinate much more frequently, which is a known side effect of steroids.
Using high doses of steroids or using steroids for a long time can sometimes lead to problems with the adrenal glands small organs that make hormones to regulate many body processes. Frequent urination can be a sign of this issue. Other symptoms include dizziness, a fast heart rate, irregular heartbeats, blurry vision, or feelings of weakness. Tell your doctor if you notice these symptoms while taking steroids.
Several other health conditions unrelated to UC could also lead to increased urination. They include:
- Bladder stones
- Prostate problems, including prostatitis or benign prostatic hyperplasia
- An overactive bladder
- Interstitial cystitis, also known as painful bladder syndrome
Read Also: Meal Replacement Shakes For Ulcerative Colitis
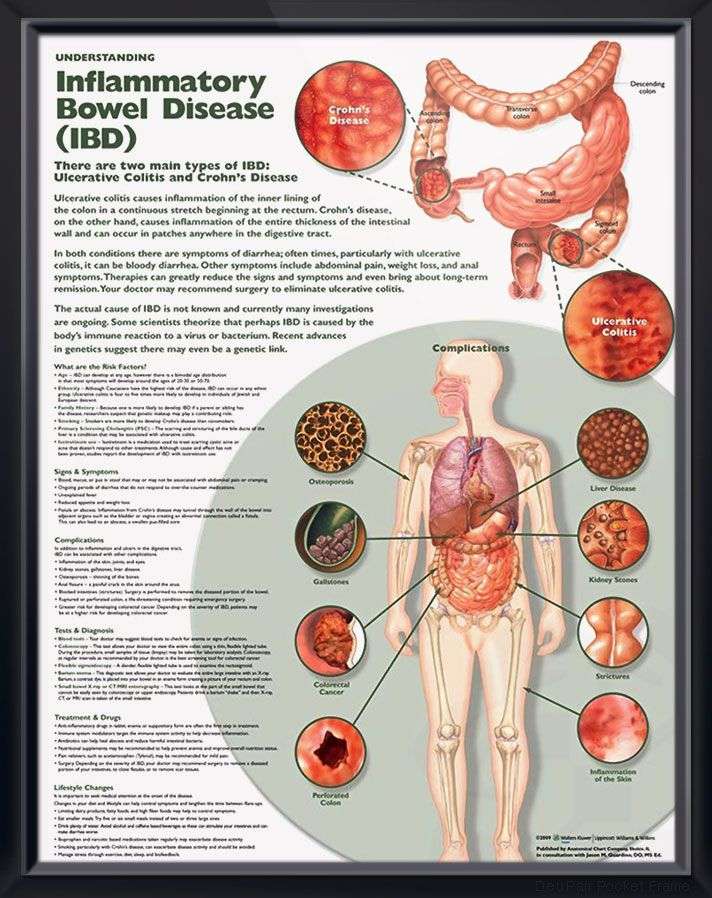
What Are The Symptoms Of Ibd
The symptoms of IBD partly depend on where the inflammation occurs. Inflammation in the colon often causes diarrhea and bloody stools. Inflammation in the rectum often causes urgency and tenesmus . If the colitis is severe, the inflammation may extend deep into the wall of the intestine and cause abdominal pain and cramping.
Crohns disease often causes abdominal pain, tenderness, and cramping. These symptoms occur as the muscles in the intestine push food through narrowed areas. Stomach cramps and bowel obstruction may lead to nausea and vomiting. In addition to bowel symptoms, you may have other symptoms such as severe fatigue, weight loss, loss of appetite, fever, sore or red eyes, skin rashes, and pain in the large joints, such as knees. People with IBD tend to have flares with active symptoms and periods of remission with no symptoms.
What Are The Complications Of Ibd
Scar tissue may result as the inflamed tissue heals. This scarring can narrow or even block the intestine. The narrowed area is called a stricture. If food cant move through your intestine, you may have nausea and vomiting. Long-term obstruction raises the pressure in the part of the intestine before the narrowed or blocked area. This pressure can cause the inflamed intestinal wall to burst . An untreated perforation lets intestinal contents out into the abdomen. This is quite painful and requires immediate surgery. More commonly, the perforation forms a small hole and a tunnel to another organ as a way to release the pressure that builds up from the blockage. This tunnel is called a fistula. A fistula most commonly connects to another part of the intestine, to the skin, to the bladder, or to the vagina. If a fistula does not connect to an exit site, it can form a cavity filled with infected intestinal contents and pus. This is called an abscess.
Read Also: Foods You Can Eat With Ulcerative Colitis
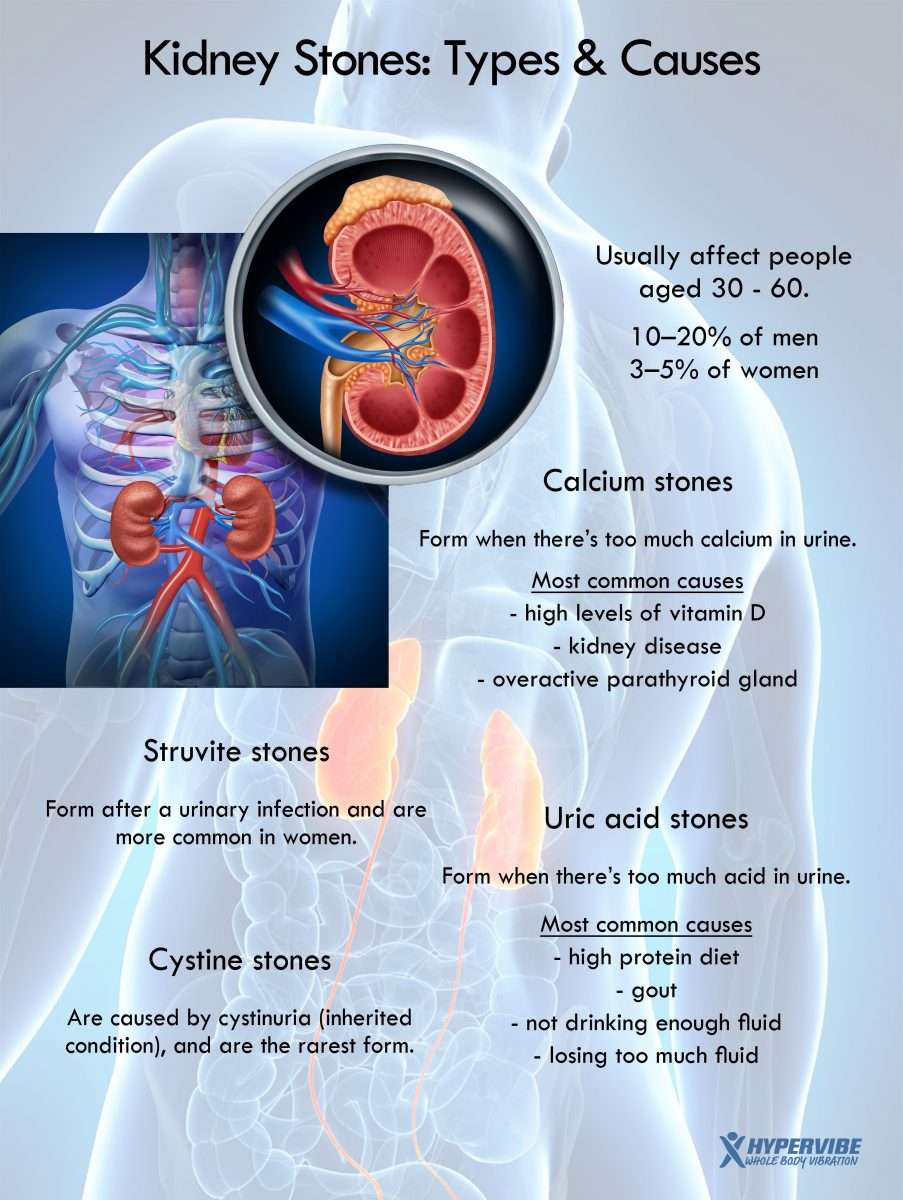
Why Do People With Crohns Disease Get Kidney Stones More Often
There are a number of reasons why people with Crohns Disease are more likely to get kidney stones.
Kidney stones are formed when there is a decrease in urine volume and an increase in stone-forming substances in the body.
One of the most common causes of kidney stones is malabsorption. This is a condition where the small intestine isnt able to absorb nutrients properly. For example, fat in the small intestine could bind to calcium, releasing oxalates. This stone-producing substance can then absorb into the kidneys.
In addition, dehydration is a significant risk factor for kidney stones.
Those with Crohns Disease are more likely to have these two symptoms. Also, they may have more concentrated urine, which is another risk factor for kidney stones.
Kidney stones are a serious health concern. They cause pain and discomfort and create the potential to block normal urine flow. Speak with your treating physician as soon as you notice the warning signs of a kidney stone developing.
Bladder And Bowel Incontinence
Incontinence is a loss of control of a personâs bowels or bladder which can cause accidental leakage of body fluids and waste. Incontinence can be more than a physical problem. It can disrupt your quality of life if its not managed well.
Fear, anxiety, and anger are common feelings for people dealing with incontinence. You may avoid being intimate or having sex because you are afraid of urine, gas, or stool leakage. Fear of having an accident may keep you from being physically active, enjoying hobbies, or spending extended time outside your home.
Both men and women can have incontinence during and after surgery or some other treatments for cancer. Incontinence can also occur because of other non-cancer medical conditions. Be sure to talk to your health care team if you have difficulty controlling urination or bowels. Talking about incontinence can be embarrassing, but being open and honest with your health care team can help manage it.
Recommended Reading: Ulcer On White Of Eye
Living With Kidney Stones And Crohns Disease
Kidney stones can cause a variety of complications , some of which require surgery to resolve. As one MyCrohnsAndColitisTeam member shared, I had three kidney stone surgeries in the past 30 days. I was in horrific pain!
Having kidney stones can also make dealing with Crohns even more frustrating. Kidney stones can impact a persons quality of life and overall well-being. As one member explained, I have a five-millimeter kidney stone. I had to have an emergency stent put in yesterday. I feel awful pain and pressure today. Does anyone else with an ileostomy suffer from kidney stones? Add it to the list of awful things that come along with Crohns. Another member shared: Crohns and kidney stones are a thing! Unfortunately, theyre a yearly occurrence, sometimes more.
One member shared that they believe kidney stones to be as difficult as Crohns: Ive got kidney stones that are related to Crohns. I passed a couple, but I have one in my left kidney. I cant wait until that starts to move! The side effects of Crohns are as horrendous as the disease itself.
Passing A Kidney Stone
Small kidney stones may pass on their own without treatment. A doctor may recommend drinking more fluids to help flush the stone out of the system.
In some cases, the doctor may prescribe the medication Tamsulosin. This drug relaxes the ureter, making it easier for stones to pass. Some people may also require over-the-counter or prescription pain relief medication.
According to the AUA, a person should wait no longer than 6 weeks to pass a small kidney stone. They should seek medical attention sooner if they experience worsening pain or an infection.
In some cases, a doctor may recommend surgery to place a ureteral stent to allow urine to bypass the stone, with or without removing the stone at the same time. According to the Urology Care Foundation, doctors usually reserve surgery for stones that may have caused or lead to infection or stones that do not pass and block urine flow from the kidney.
Read Also: What Foods Should You Avoid If You Have Ulcerative Colitis
Inflammatory Bowel Disease May Increase Ckd Risk
Inflammatory bowel diseases , such as ulcerative colitis and Crohns disease, or their treatments may increase the risk for chronic kidney disease , according to new research published in Clinical Gastroenterology and Hepatology.
Ravy K.Vajravelu, MD, MSCE, of the University of Pennsylvania in Philadelphia, andcolleagues conducted a retrospective study comparing 17,807 IBD patients fromthe United Kingdom with 63,466 matched control patients. Stage 3 or higher CKD,assessed by repeat measurements of estimated glomerular filtration rate ordiagnosis code, developed in 5.1% of IBD vs 3.5% of control patients, with age-standardizedincidence rates of 130.3 vs 91.3 per 100,000 person-years. The risk of CKD inpatients with IBD diminished with age, from a 7.9-fold increased risk of CKD byage 16 years to a 1.13-fold increased risk at age 77 years. The risk was onlyslightly lower for ulcerative colitis compared with patients who had Crohns disease.Active flare did not appear to influence eGFR.
Previous studies havelinked common non-biologic IBD therapies with impaired renal function. In thisstudy, neither 5-aminosalicylate nor methotrexate was associated with reducedeGFR. Azathioprine was associated with a slightly higher eGFR . Biologic medications, such as infliximab, adalimumab, andvedolizumab, are not usually prescribed by general practitioners in the UK, butthese medications have not been associated with CKD among IBD patients in priorstudies, according to the authors.
Background And Aim Of The Work
Historical studies have demonstrated that the prevalence of symptomatic nephrolithiasis is higher in patients with inflammatory bowel disease , compared to general population. The aim of the review was to analyze literature data in order to identify the main risk conditions described in literature and the proposed treatment.
Don’t Miss: Offloading The Diabetic Foot For Ulcer Prevention And Healing
S Boulajaad1* M Haida1 Ait Errami1 S Oubaha2 Z Samlani1 And K Krati1
*Corresponding author:Received: Accepted:Keywords
Abstract
The extradigestive manifestations of chronic inflammatory bowel disease most often affect the articulations, skin, eyes, liver and bile ducts. Renal involvement is rare, and manifests as kidney stones, glomerulonephritis, tubulointerstitial nephritis, and secondary amyloidosis. In this context of chronic inflammatory bowel disease, in particular ulcerative colitis, renal involvement is very often secondary to nephrotoxicity of the basic treatment of digestive pathology, and very rarely an authentic extradigestive manifestation of intestinal disease.
We report a case of IgA nephropathy as an extra-digestive manifestation of ulcerative colitis.
The objective of this study is not to neglect the IgA nephtopathy as an extradigestive manifestation of IBD which, even though rare, remains a condition to be looked for by clinicians during the follow-up of IBD.
How To Use Sulfasalazine Suppositories
Sulfasalazine suppositories are used to treat inflammatory bowel disease.
You will generally use the suppositories twice a day, in the morning and at bedtime. Use them after you do a poo.
You May Like: What Can Be Done For An Ulcer