Summary Of Studies Included In The Review
Clinical evidence profile: different positions for repositioning â semi recumbent position versus standard care .
9.2.1.1. Comparison between kinetic beds and conventional beds
Clinical evidence profile: kinetic treatment table versus standard care for pressure ulcer prevention.
9.2.1.2. RCT Narrative summary
The following study is summarised as a narrative because the outcomes were not appropriate for GRADE due to incomplete outcome reporting:
One study examining the effects of the 30° tilt position in reducing the incidence of non-blanching erythema compared to the use of 90° lateral and supine position reported that 5 out of 23 participants in the experimental arm were unable to tolerate the intervention. No data was provided for the individuals in the control arm.
When You Are In Bed
Use a foam mattress or one that is filled with gel or air. Place pads under your bottom to absorb wetness to help keep your skin dry.
Use a soft pillow or a piece of soft foam between parts of your body that press against each other or against your mattress.
When you are lying on your side, put a pillow or foam between your knees and ankles.
When you are lying on your back, put a pillow or foam:
- Under your heels. Or, place a pillow under your calves to lift up your heels, another way to relieve pressure on your heels.
- Under your tailbone area.
- Under your shoulders and shoulder blades.
- Under your elbows.
Other tips are:
- DO NOT put pillows under your knees. It puts pressure on your heels.
- Never drag yourself to change your position or get in or out of bed. Dragging causes skin breakdown. Get help if you need moving in bed or getting in or out of bed.
- If someone else moves you, they should lift you or use a draw sheet to move you.
- Change your position every 1 to 2 hours to keep the pressure off any one spot.
- Sheets and clothing should be dry and smooth, with no wrinkles.
- Remove any objects such as pins, pencils or pens, or coins from your bed.
- DO NOT raise the head of your bed to more than a 30 degree angle. Being flatter keeps your body from sliding down. Sliding may harm your skin.
- Check your skin often for any areas of skin breakdown.
Appendix 2 Ovid Medline Economics Search Strategy
1 exp Pressure Ulcer/ 2 ).tw. 3 ).tw. 4 ).tw. 5 or/1â4 6 exp Posture/ 7 .tw. 8 position*.tw. 9 .tw. 10 .tw. 11 .tw. 12 turning.tw. 13 .tw. 14 pressure relie*.tw. 15 .tw. 16 or/6â15 17 5 and 16 18 economics/ 19 exp “costs and cost analysis”/ 20 economics, dental/ 21 exp “economics, hospital”/ 22 economics, medical/ 23 economics, nursing/ 24 economics, pharmaceutical/ 25 .ti,ab. 26 .ti,ab. 27 value for money.ti,ab. 28 budget*.ti,ab. 29 or/18â28 30 adj cost).ti,ab. 31 .ti,ab. 32 adj expenditure).ti,ab. 33 or/30â32 34 29 not 33 35 letter.pt. 36 editorial.pt. 37 historical article.pt. 38 or/35â37 39 34 not 38 40 Animals/ 41 Humans/ 42 40 not 43 39 not 42 44 17 and 43
Read Also: Wound Care Treatment For Diabetic Foot Ulcer
What Items Should Be In Our Bundle
The sections above have outlined best practices in pressure ulcer prevention that we recommend for use in your bundle. However, your bundle may need to be individualized to your unique setting and situation. Think about which items you may want to include. You may want to include additional items in the bundle. Some of these items can be identified through the use of additional guidelines .
Action Steps
Identify your bundle of best practices.
3.5.1 How do we customize the bundle for specific work units?
Patient acuity and specific individual circumstances will require customization of the skin and pressure ulcer risk assessment protocol. It is imperative to identify what is unique to the unit that is beyond standard care needs. These special units are often the ones that have patients whose needs fluctuate rapidly. These include the operating room, recovery room, intensive care unit, emergency room, or other units in your hospital that have critically ill patients. In addition, infant and pediatric patients have special assessment tools, as discussed in section 3.3.5.
Action Steps
- Identify the units that will require customization of the skin and risk assessment protocols.
- Modify the bundle, the assignment of roles, and the details of the unit to meet these special features.
Additional Information
Was The Treatment Allocation Adequately Concealed
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation sequentiallyânumbered drug containers of identical appearance sequentiallyânumbered, opaque, sealed envelopes.
High risk of bias
Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on: using an open random allocation schedule assignment envelopes were used without appropriate safeguards alternation or rotation date of birth case record number any other explicitly unconcealed procedure.
Unclear
Insufficient information to permit judgment of low or high risk of bias. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgment, for example if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed.
Also Check: How To Find Out If You Have Ulcerative Colitis
How The Intervention Might Work
Pressure, from lying or sitting on a particular part of the body results in oxygen deprivation to the particular area . Normally, this results in pain and discomfort, which stimulates the person to change position. However, if the person is unable to reposition themselves, or has impaired sensation and therefore does not experience the discomfort, assistance will be required. Repositioning reduces the duration of pressure experienced by the tissues and so decreases tissue hypoxia and consequently the theoretical risk of pressure ulceration .
Negative aspects of frequent repositioning
Whilst frequent repositioning underpins current practice guidelines, it may also be associated with negative consequences for patients, nursing staff and health care . Repositioning can lead to disruption of sleep, particularly sleep fragmentation . In acutely ill people, disruption of sleep can lengthen recovery, suppress immune function and predispose people to infection . A sleep cycle, which has light and deep stages of sleep, occurs about every 90 minutes. Consequently if repositioning is undertaken every two hours, it may result in fragmentation of sleep at a detrimental stage of the sleep cycle .
Other negative effects of repositioning include possible increases in patients’ pain perception. Although regular movement is important, unnecessary repositioning may cause increased discomfort for people with wounds, stiff joints, bony pain or contractures.
What Other Kinds Of Aids Are Available
Another thing that can help prevent damage to the skin is sheepskin mattress covers. Some people find sheepskin unpleasant, though, because it can make your skin very warm after a while.
Pressure ulcers often occur on peoples heels. So heels are often elevated using pillows, or special heel protectors made out of animal skin or foam are used. But there is no proof that these actually prevent pressure ulcers. Some people find the heel protectors uncomfortable and choose not to wear them. There are also concerns that they could increase the risk of falling if people get up and walk around while wearing them.
There hasn’t been much research on aids such as special positioning cushions or special cushions for people to sit on either.
Recommended Reading: Ulcerative Colitis Iv Infusion Treatment
Scheduling Repositioning: Consistency Is The Key To Patient Compliance
The two-hour gap between each “turn” came from the spinal injury unit at Stoke Mandeville hospital in the United Kingdom, although others might take claim for it, I suppose. My father was in the unit for over a year in 1956, and the ward orderlies would start at one end of the Nightingale ward, and by the time they got to the last patient, two hours had elapsed, and they would start again. Quite different from the spinal injury units of today.
There is no doubt in my mind at all: The most important thing about repositioning schedules is that the manager of the floor insists on a consistent approach and follows up with checks to ensure whatever system is chosen is actually carried out. It is just too important to assume the nursing assistants and other staff will actually stick to the policy without oversight. Total patient involvement happens only if there is total staff involvement. If there is a posted schedule and patients don’t see anyone refer to it, they know it is not important. For them, this translates to all pressure injury prevention strategies, not just a posted schedule that no one has updated because everyone ignores it. This is why oversight from management and senior staff is important.
Appendix 1 Ovid Medline Ovid Embase And Ebsco Cinahl Effectiveness Search Strategies
Ovid MEDLINE
1 exp Pressure Ulcer/ 2 ).tw. 3 ).tw. 4 ).tw. 5 or/1â4 6 exp Posture/ 7 .tw. 8 position*.tw. 9 .tw. 10 .tw. 11 .tw. 12 turning.tw. 13 .tw. 14 pressure relie*.tw. 15 .tw. 16 or/6â15 17 5 and 16 18 randomized controlled trial.pt. 19 controlled clinical trial.pt. 20 randomized.ab. 21 placebo.ab. 22 clinical trials as topic.sh. 23 randomly.ab. 24 trial.ti. 25 or/18â24 26 ).sh. 27 25 not 26 28 17 and 27
Ovid EMBASE
1 exp Decubitus/ 2 ).tw. 3 ).tw. 4 ).tw. 5 or/1â4 6 exp patient positioning/ 7 .tw. 8 position$.tw. 9 .tw. 10 .tw. 11 .tw. 12 turning.tw. 13 .tw. 14 or/6â13 15 5 and 14 16 Randomized controlled trials/ 17 SingleâBlind Method/ 18 DoubleâBlind Method/ 19 Crossover Procedure/ 20 .ti,ab. 21 .ti,ab. 22 .ti,ab. 23 or/16â22 24 animal/ 25 human/ 26 24 not 25 27 23 not 26 28 15 and 27
EBSCO CINAHL
S16 S5 and S15 S15 S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 S14 TI body N5 posture* or AB body N5 posture* S13 TI turning or AB turning S12 TI turn* N5 frequen* or AB turn* N5 frequen* S11 TI turn* N5 interval* or AB turn* N5 interval* S10 TI turn* N5 patient* or AB turn* N5 patient* S9 TI position* or AB position* S8 TI or AB S7 S6 S5 S1 or S2 or S3 or S4 S4 TI or AB S3 TI or AB S2 TI decubitus or AB decubitus S1
You May Like: How To Heal Venous Stasis Ulcers
Single And Multicomponent Interventions
A number of standalone interventions to prevent pressure ulcers have been evaluated in high quality systematic reviews. These reviews have found convincing evidence of effectiveness for high-specification foam mattresses,7 but not for standalone nutritional interventions8 or for the application of topical agents over bony prominences.9 While both risk assessment and repositioning of patients are likely to be worthwhile practices, there is currently no clear evidence to favour one particular pressure ulcer risk assessment tool,10 or a particular frequency or position for repositioning.11
In practice, multicomponent interventions or care bundles are generally recommended over standalone interventions for the prevention of pressure ulcers. Recently, an NHS Stop the Pressure campaign was rolled out nationally to support a 50% reduction in pressure ulcer prevalence throughout winter 2013/14.2 As well as providing educational resources, the campaign promotes the SSKIN care bundle that emphasises the need for a bundle of practices, incorporating appropriate pressure-relieving surfaces, skin inspections, repositioning of patients, incontinence/moisture management, and where necessary nutrition/hydration support.
How Often Is Repositioning Necessary
Even though it’s often recommended that people be repositioned every two hours, there’s no single recommendation that works for everyone. Some people can lie in the same position for quite a long time without getting ulcers, while others need to switch much more often. Research has not yet found out how often someone should change position to get the best preventive effect.
Unnecessarily moving someone too much for no good reason can also have disadvantages. For instance, repositioning every two hours at night may wake the person each time and keep them from getting a good nights sleep. Changing position can also be very painful for people who have wounds or joint conditions. Frequent repositioning is physically demanding for caregivers or family members too. It’s therefore important to observe how often someones position really needs to be shifted. It can then help to make a note every time they are repositioned.
Also Check: How Do You Cure Mouth Ulcers
Classification Of Pressure Ulcers
Pressure Ulcers would be classified as grade I to IV according to The Pressure Ulcer Advisory Panel Consensus Development Conference 1989, and the National group for the study and counseling in Pressure Ulcers and Chronic Wound-Spain , 2003. We did not use the new pressure ulcer terminology and the updated stages provided by The National Pressure Ulcer Advisory Panel- NPUAP, given that all hospitals in our country follow the Ministry of Health Guidelines according to the primary pressure ulcers classification and also Pus are reported in this way.
This system, accepted until very recently, establishes four stages for pressure ulcers. The main objective of any classification system is to standardize the collection of information and provide a standard description of the severity of the ulcer for both clinical practice, evaluation, or research purposes.
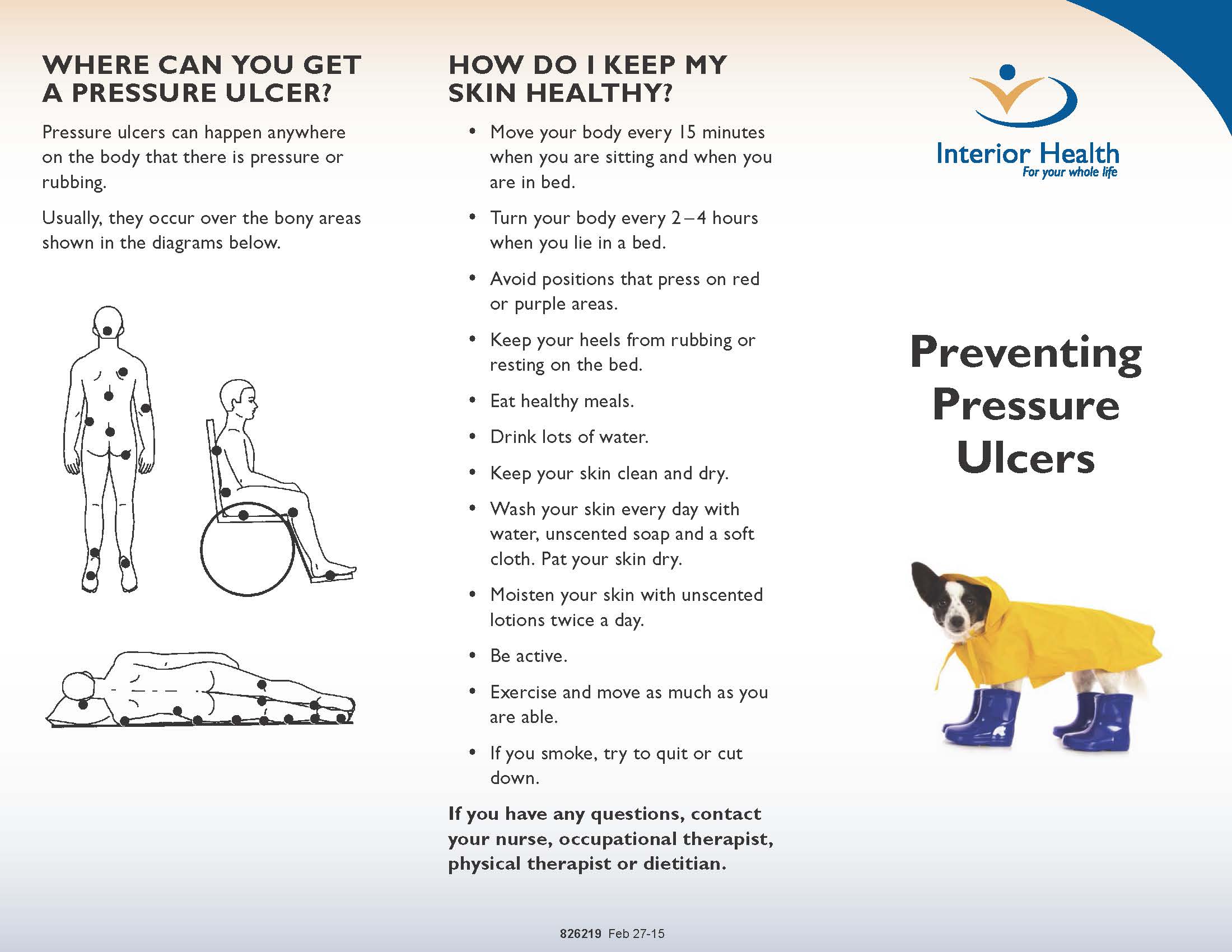
Description Of The Condition

A pressure ulcer is “a localised injury to skin or underlying tissue usually over a bony prominence as a result of pressure or pressure in combination with shear” . PUs occur when the soft tissue is compressed between a bony prominence and an external surface for a prolonged period of time.
PU classification systems provide an accurate and consistent means by which the severity and level of tissue injury of a PU can be described and documented .The words ‘stage’ , ‘grade’, and ‘category’ are used interchangeably to describe the levels of softâtissue injury. The original staging system includes Stages 1 to 4. Stage 1 reflects persistent nonâblanching erythema of the skin . Stage 2 involves partialâthickness skin loss . Stage 3 reflects fullâthickness skin loss involving damage, or necrosis, of subcutaneous tissue, whereas in Stage 4 the damage extends to the underlying bone, tendon or joint capsule. However, more recently, two additional classifications have been identified, namely: ‘unclassified/unstageable’ and ‘deep tissue injury’ . PUs are associated with pain, an increased risk of infection and sepsis, longer hospital stays, higher hospitalisation costs and mortality .
Read Also: Corneal Ulcer Dog Home Remedy
Which Interventions Are The Most Important
Pressure ulcers usually heal very slowly, and may come back. That’s why it’s so important to make sure they don’t develop in the first place. People who are confined to a wheelchair or have to stay in bed for a long time often say that they can feel parts of their body becoming sore. It’s important to pay attention to what they say, to quickly reduce pressure on their skin, and regularly change the position they sit or lie in.
Observing which parts of the body are most susceptible to pressure, as well as the positions that put the most pressure on them, can help you get an idea of what sort of relief might be helpful. For example, lying down puts much less pressure on your backside than sitting in a chair. If you use a wheelchair, you can find out what helps to reduce the pressure and then make that your routine.
It’s also important to try to move if possible even if you have to lie in bed or sit in a wheelchair. If you are able to sit up, leave the bed, or even walk a few steps with a bit of help, its a good idea to do that as often as possible.
Was The Allocation Sequence Adequately Generated
Low risk of bias
The investigators describe a random component in the sequence generation process such as: referring to a random number table using a computer random number generator coin tossing shuffling cards or envelopes throwing dice drawing of lots.
High risk of bias
The investigators describe a nonârandom component in the sequence generation process. Usually, the description would involve some systematic, nonârandom approach, for example: sequence generated by odd or even date of birth sequence generated by some rule based on date of admission sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process to permit judgment of low or high risk of bias.
You May Like: What To Eat And Drink If You Have An Ulcer
Repositioning To Prevent Pressure Ulcers
Pressure ulcers, also called pressure injury, pressure sores, decubitus ulcers and bed sores are caused by pressure, rubbing or friction at the weightâbearing bony points of the body . A pressure ulcer is characterised by an area of localised injury to the skin or underlying tissue over a bony prominence that results from pressure or shearing, or a combination of both. Pressure ulcers most commonly occur in the elderly, or those who are immobile, either when in bed or sitting. Repositioning is one strategy used alongside other preventative strategies to relieve pressure, and so prevent development of pressure ulcers. Repositioning involves moving the person into a different position to remove or redistribute pressure from a particular part of the body.
We identified three studies which recruited 502 people. Evidence to support the use of repositioning to prevent pressure ulcers is low in volume and quality and we still do not know if particular positions or frequencies of repositioning reduce pressure ulcer development. None of the trials reported on pain or quality of life. There is a need for further research to measure the effects of repositioning on pressure ulcer development and to find the best repositioning regimen in terms of frequency and position. It is important to emphasise that this lack of evidence showing that repositioning is effective or which repositioning regimen is the best does not mean that repositioning is ineffective.