Conditions Of The Skin
The second most common non-GI symptom of ulcerative colitis is skin inflammation, which can manifest as a number of skin conditions. The most common being an ulcerating skin problem called pyoderma gangrenosum, says Rubin, which is often caused by injury or trauma to your skin.
A lot of times people think they nicked themselves shaving their legs, but it doesnt get better, he says. It doesnt respond to just treating the bowel it may need treatment that works both on the bowel and on the skin. For difficult cases, your doctor may refer you to a dermatologist with expertise in these conditions.
Joint Pain And Ibd: Whats The Connection
People with inflammatory bowel disease Crohns disease and ulcerative colitis may experience joint pain as an extraintestinal symptom of their condition that is, a symptom occurring outside the intestines. Nearly one-third of people with IBD have joint pain due to comorbid arthritis.
If you are living with IBD and experience joint pain, reduced range of motion, or stiffness, read on to find out how joint pain and IBD are related and how to manage the two conditions.
He Had Recurring Pain For Nearly A Decade
The pain woke the 52-year-old physician from a dead sleep. It was as if all the muscles in his right leg, from those in the buttock down his thigh to the very bottom of his calf, were on fire. He shifted slightly to see if he could find a more comfortable position. There was a jag of pain, and he almost cried out. He glanced at the clock: 4 a.m. In just three hours he would have to get up. He had a full day of patients to see. Massage didnt help. He couldnt get comfortable lying flat, so finally he moved to the living room, to a recliner. Only then, and only by lying completely still, did he manage to get the pain to abate. He drifted off, but never for long. The searing pain in his leg and buttock slowly eased, and by the time his alarm went off, he could stand and walk though his muscles still ached and he had to baby his right leg, causing a limp.
Between patients, he arranged to see his own doctor. Hed had pain off and on in his buttocks, one side or the other, for more than a year. The pain was in the middle of each cheek and was worse when he was sitting and at the end of the day. Walking to and from his car on the way home was brutal. And then, as mysteriously as it came, it would disappear only to come back a week or two later.
Recommended Reading: Does Ulcerative Colitis Make You Tired
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
Whats The Connection Between Ibd And Joint Pain
IBD and inflammatory arthritis are both thought to be autoimmune conditions, in which the bodys immune system mistakenly mounts an attack on its own healthy tissues. Its common for two or more autoimmune diseases to occur at the same time. For instance, rheumatoid arthritis is a typical comorbidity for people with IBD. Other types of arthritis, such as enteropathic spondylitis, are also associated with gastrointestinal disease.
Read Also: Tnf Alpha Inhibitors For Ulcerative Colitis
Favorite Ulcerative Colitis Blogger
Sam Cleasby created her blog in 2013 to raise awareness of IBD and her struggles with self-esteem. Cleasby also has a radio show on BBC Radio Sheffield in which she shares about modern family life, including relationships, disability, nutrition, and kids. You can subscribe to her blog via email or follow her on or .
Sex Pregnancy And Ankylosing Spondylitis
Sex may be painful if you have ankylosing spondylitis. If it is, try taking some painkillers beforehand and experiment with different positions.
Ankylosing spondylitis can make you feel tired, so its important your partner understands how your condition affects you. Good communication can help you maintain an active sex life and counselling can sometimes benefit both partners.
Its fine to use the contraceptive pill if you have ankylosing spondylitis, but you should tell your doctor youre taking it.
If youre thinking of starting a family, its very important for both men and women with ankylosing spondylitis to discuss medication with a doctor beforehand.
Some drugs such as methotrexate should be stopped several months before a woman tries to get pregnant. Latest research suggests its safe for men to take methotrexate when trying for a baby with their partner.
Biological therapies seem to be safe in the earlier stages of pregnancy but are then stopped later in pregnancy.
If you become pregnant while using a conventional DMARD such as methotrexate or a biological therapy, discuss this with your rheumatology team as soon as possible.
Usually, pregnancy doesnt cause any special problems for the mother or baby, though the symptoms of ankylosing spondylitis may not ease during pregnancy. If your spine is very stiff, it may not be possible to have an epidural during childbirth. This is an injection into the back that stops people feeling pain in part of the body.
Don’t Miss: What Do I Take For An Ulcer
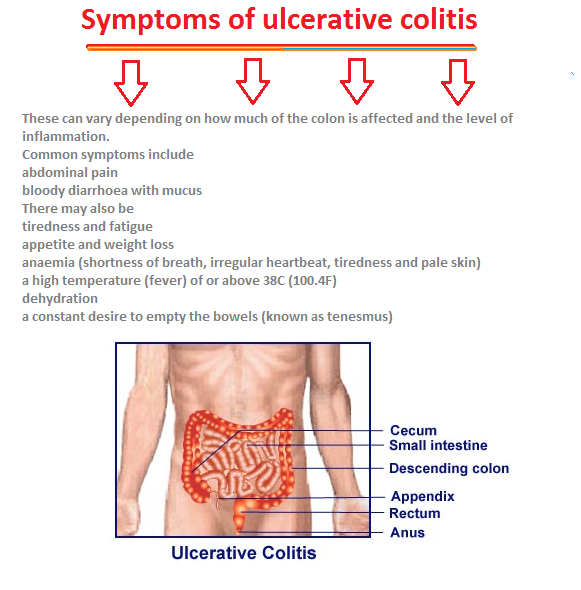
What Are The Causes And Risk Factors Of Ulcerative Colitis
Ulcerative colitis is believed to be caused by an abnormal response by your bodys immune system.
Your immune system is supposed to defend you against harmful invasive bacteria and viruses. But in some people, the immune system mistakenly attacks the bodys own tissue.
While we dont know exactly what causes ulcerative colitis, there are two leading theories:
Experts believe that ulcerative colitis develops because of a combination of environmental factors and genetic predisposition.
Fatty cold-water fish such as mackerel, tuna, salmon, sardines, and herring are rich sources of omega-3 fatty acids.
Editor’s Picks
How To Treat Pain
There are various treatment options for UC, and the best approach for a person will depend on the severity of their symptoms. Over-the-counter medications can sometimes help relieve the pain that UC can cause. However, severe cases require stronger pain relievers.
Medications for the treatment of UC include:
Also Check: What Makes Ulcerative Colitis Worse
Reducing Your Arthritis Risk When You Have Ulcerative Colitis
Arthritis is the most common complication outside the gut for people with ulcerative colitis. These dos and donts will help you protect your joints.
As if gut pain from ulcerative colitis werent enough, as many as 30 percent of people with an inflammatory bowel disease , including ulcerative colitis, will develop problems with their joints, according to the Crohns and Colitis Foundation. Indeed, arthritis is the most common complication that occurs beyond the intestines.
Although its not fully understood, there seems to be a link between the gut and joints, says Harry D. Fischer, MD, the chief of rheumatology at Lenox Hill Hospital in New York City. For example, a bacterial infection in the digestive tract can cause a reactive type of arthritis, he notes. In addition, both arthritis and ulcerative colitis have a genetic component.
According to the Crohns and Colitis Foundation, people with ulcerative colitis tend to have one of three forms of arthritis:
- Peripheral arthritis , which affects large joints such as the knees, ankles, elbows, or wrists when IBD is properly treated and controlled, PA joint pain and symptoms typically improve
- Axial arthritis, which causes pain and stiffness in the spine and lower back
- Ankylosing spondylitis, a more severe type of arthritis that affects the spine and can lead to joint damage. Its an uncommon complication that affects between 2 and 3 percent of people with IBD.
Skin Joint Or Eye Problems
When you have UC, the lining of your large intestine gets inflamed and sets off your symptoms. For some people, this inflammation also shows up in other body parts during a flare. Experts arent sure why.
You could have symptoms like:
Let your doctor know whenever you get new UC symptoms. That way, they can change your treatment plan if needed.
Recommended Reading: Over The Counter Remedies For Ulcers
Pain From Inflammatory Bowel Disease
Pain is a big one! People living with IBD often feel misunderstood by their friends and family members and even the healthcare professionals they look to for information. Because IBD is often invisible, loved ones don’t understand that pain plays a major role in the day to day and that your entire body can hurt, not just your stomach.
Treatment Options For Joint Pain In Ibd
You have several options for managing joint pain in IBD. Some treatments can help address the underlying inflammation, while others may help to manage symptoms or complications. Most arthritis associated with IBD will correlate with the activity of ones colitis and will respond to treatment. You may still have arthritis of the smaller joints of the hands and feet, even when the colitis is in remission.
Don’t Miss: What Can I Do To Relieve Stomach Ulcer Pain
What Causes Ulcerative Colitis
Unfortunately the cause of ulcerative colitis is unknown, although both genetic and the environmental causes have been proposed.
Most patients with ulcerative colitis do not have anyone else in the family with ulcerative colitis. However up to 20 percent of patients with ulcerative colitis have at least one relative with either ulcerative colitis or Crohn’s disease. The genes involved in ulcerative colitis are not as well understood as in Crohn’s disease, and there are no commercially available genetic tests we currently recommend for the diagnosis of ulcerative colitis.
The increase in ulcerative colitis in some populations around the world has led some researchers to believe there may be environmental causes for ulcerative colitis. Infections and diet are among other potential environmental causes for ulcerative colitis however there is not enough information in this field to make any firm conclusions. There is still much to learn in these areas and research is ongoing to determine the cause of ulcerative colitis.
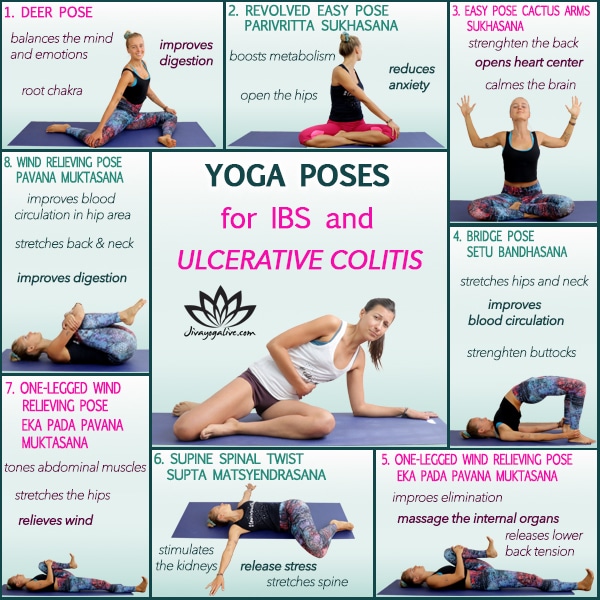
Home Remedies For Uc Joint Pain
Just like other aspects of your UC, joint pain is sometimes one that you can help keep under control at home. According to Dr. Keller, keeping your joints moving can make all the difference. Exercise therapy, such as gentle water exercises developed for arthritis, can help with the pain, she says. And when you are sitting or standing, pay special attention to your posture. A physical therapist can help you develop an exercise program and observe your posture to help you move correctly.
Given that this all comes down to controlling inflammation, adding anti-inflammatory supplements such as turmeric to your diet may also be helpful. Curcumin is the active ingredient in turmeric and has been shown to improve inflammation related to both inflammatory arthritis and UC. In a 2021 review published in Complementary Therapies in Medicine, curcumin supplementation was associated with decreases in inflammatory markers in adults with rheumatoid arthritis and UC in comparison to a control group.
And dont forget about the variety of topical pain relievers that are now available over the counter. They are divided into different types based on how they work on your pain. Your pharmacist can help you navigate the options and choose the one that is right for you.
UC and Joint Pain: Crohns and Colitis Foundation. Arthritis and Joint Pain.
Recommended Reading: Colitis Vs Ulcerative Colitis Symptoms
Joint Pain: The Most Common Non
About 30 percent of people with ulcerative colitis experience joint pain, according to the Crohns and Colitis Foundation, making it the most common non-GI symptom of the disease. Joint pain often occurs in the knees, ankles, elbows, and wrists. Its usually joint pain thats symmetrical, meaning both knees or both ankles, says Dr. Rubin. This type of joint pain tends to parallel bowel activityso if you fix the intestine, the joint pain goes away.
However, ulcerative colitis is also related to inflammatory joint conditions that affect your spine, like ankylosing spondylitis. This type of joint pain can be independent of your bowelso your bowel can be completely in remission, and your back or your pelvis is inflamed, and you can have joint damage, says Rubin.
The good news: Some medications used to treat ulcerative colitis are also used to treat inflammatory joint conditions like ankylosing spondylitis. Its not that fixing the bowel makes these joints betterits that the medication that works on the bowel also works on these joint conditions, says Rubin. So if youre experiencing joint pain, its important to work with your doctor to understand what type of joint pain you have and get proper treatment. In some cases it may be necessary to see a doctor who specializes in the joints, a rheumatologist, to work with your IBD doctor.
How Do I Spot The Signs And Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are abdominal pain and diarrhea, which often contains blood or pus.
Symptoms of the disease typically develop gradually and come and go.
Periods without active disease known as remission may last for months or even years.
Over time, ulcerative colitis can progress to cover more of the colon. This typically leads to more severe disease and greater symptoms.
If left untreated, UC can also lead to a number of complications:
Don’t Miss: What Does An Ulcer Feel Like In Your Stomach
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Faqs About Unlock Your Hip Flexors
Q: How is this different from other hip flexibility programs?
A: What makes Ricks program unique is knowing how to unravel the tricky layers of tension with the very difficult psoas muscle in order to effectively loosen and train it.
Ricks one-of-a-kind sequential flow is your surest path to looser, stronger and healthier hips.
Q: Why are you selling this so cheap? Whats the catch?
A: There is none. Were so pleased with the number of our customers who have made the investment in this program and have enjoyed life-changing results.
Our aim is to make this available to as many guys as possible, firstly to welcome more people to our CriticalBench.com audience and secondly because were celebrating hitting a quarter million fans on Facebook.
Q: How long will it take me to do the program?
A: The program is designed to take between 10-15 minutes in total to complete.
We recommended adding the program as a daily practice to get the best results over a longer period of time. You may wish to add this program before or after your regular gym session or use it independently.
Q: How long until I see results?
A: Although everyone is different and results may vary, we know from experience how quickly its possible to feel and see a difference.
For some it may be as soon as their first session for others it may take a few sessions to really start seeing the benefits. Again, it depends on the body in question.
Q: Who is this program suitable for?
Q: Are the exercises hard to perform?
Don’t Miss: Snack Ideas For Ulcerative Colitis
Back Pain And Ulcerative Colitis
| | |
Research indicates that nearly 25 percent of people with inflammatory bowel disease including ulcerative colitis and Crohns disease experience chronic lower back pain. Ankylosing spondylitis and axial arthritis both of which can cause back pain are two common causes of back pain for people with UC.
That said, a doctor may not suspect that a person with back pain has UC unless they also experience gastrointestinal symptoms. If you do experience back pain, its important to let your doctor know even if you dont suspect its related to UC. They will be able to determine the cause of your pain and work with you to find the best way of managing it.
A person having backaches may not realize theyre related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.