Can I Get Surgery For My Ulcerative Colitis
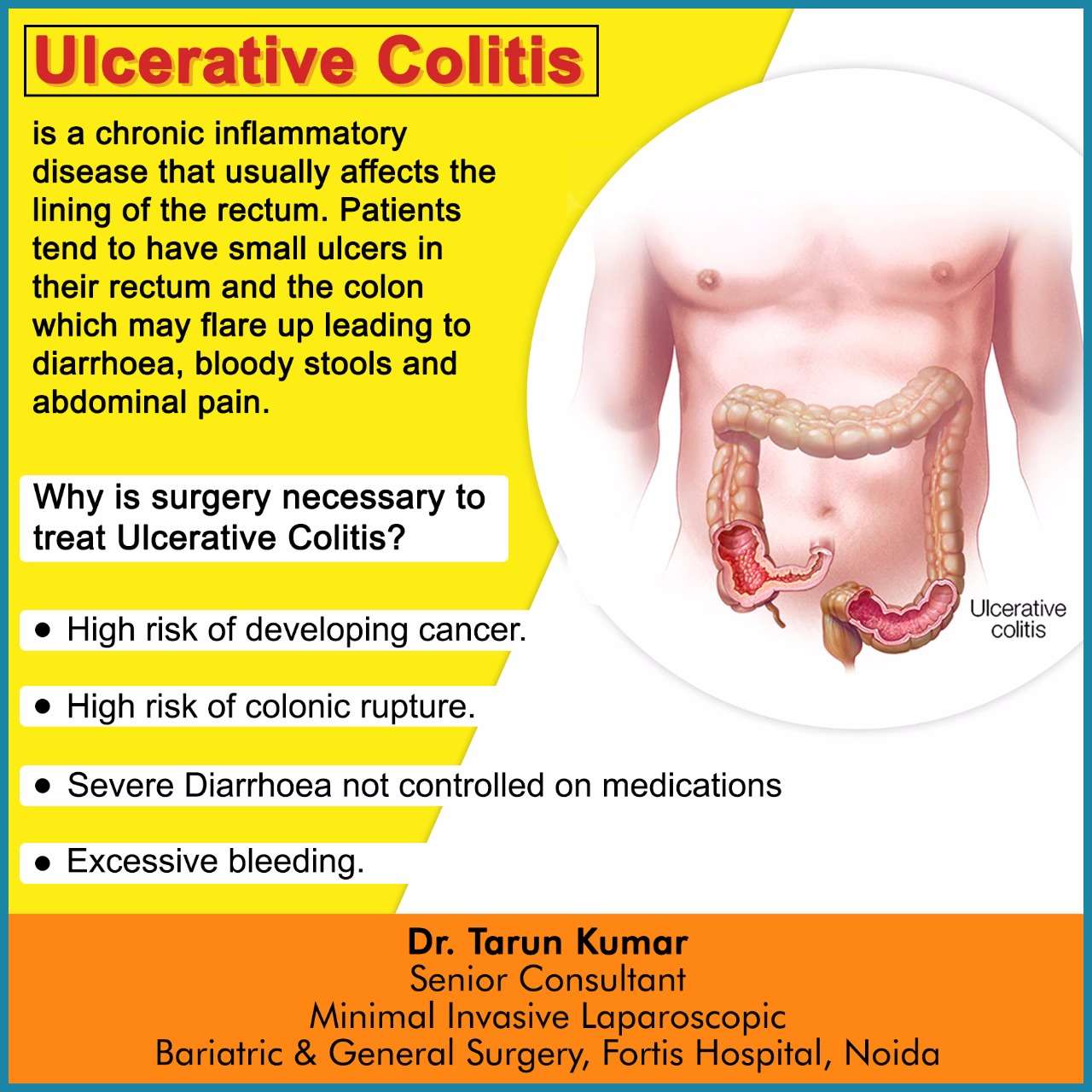
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Speak With Your Doctor
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Tags: IBD
Please note:This article outlines 11 tips to help you prevent an ulcerative colitis flare, and is based on one patients experience. Nothing in this article is meant to replace any advice you have received from your doctor.This article was contributed by Ms. Wanni Z. Below is her story.
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
Read Also: What Kind Of Yogurt Is Good For Ulcers
How To Prevent Ulcerative Colitis Flare
What are actionable steps you can take to make your symptom-free stretches last as long as possible? and stress management are probably the two biggest things as far as prevention goes, says Cohen. Parsley Health providers and health coaches often work with members who have ulcerative colitis to find a diet that helps them minimize flares and a stress management routine. Below, well dive into some specific ways to optimize your diet with natural remedies and make adjustments to your lifestyle while living with ulcerative colitis.
Recommended Reading: Can You Drink Coffee With Ulcerative Colitis
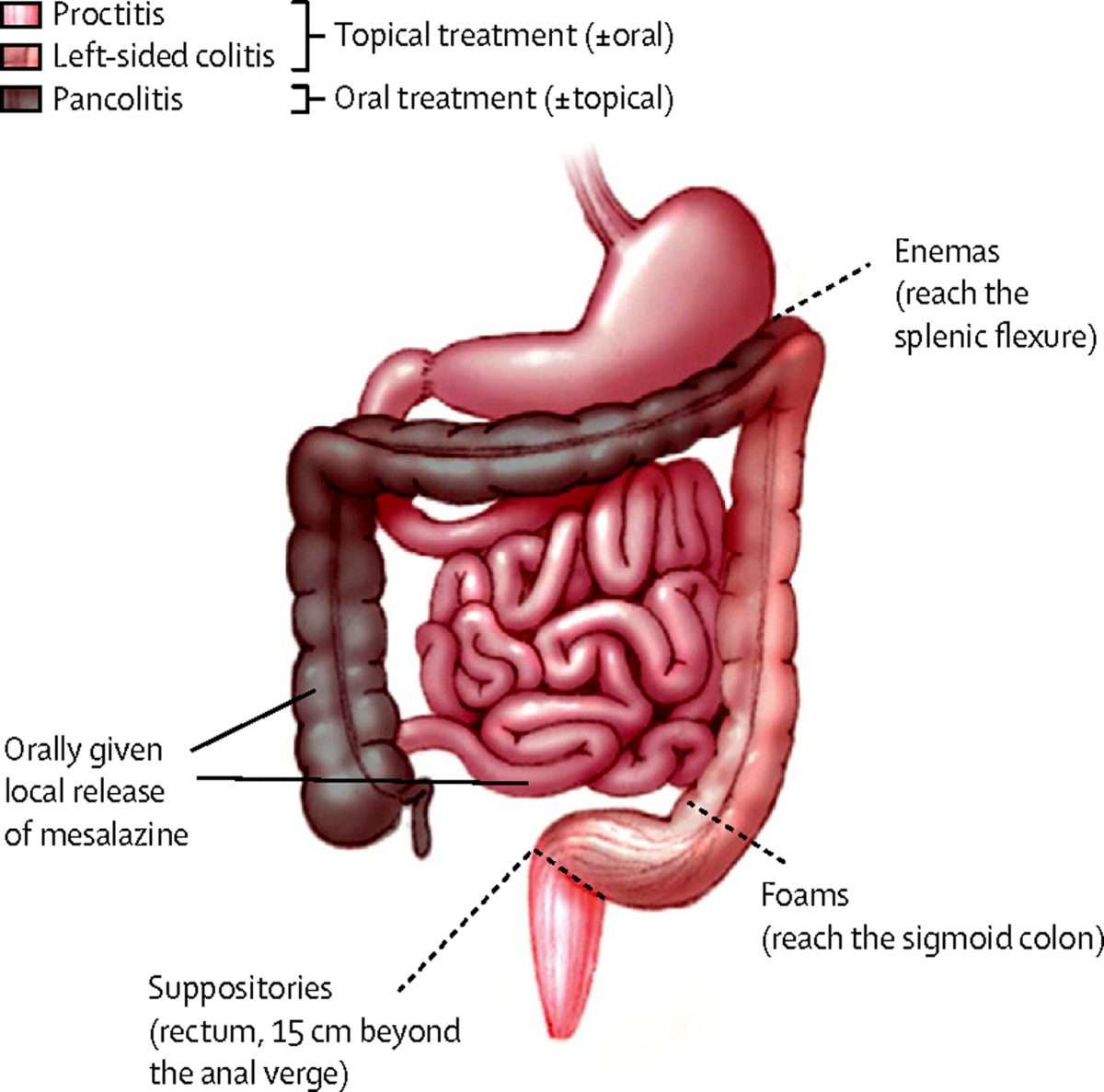
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
Also Check: Signs And Symptoms Of Peptic Ulcer
What Triggers An Ulcerative Colitis Flare
Triggers of ulcerative colitis flare-ups vary from person to person. It is helpful to identify factors that trigger or worsen your symptoms in order to try and avoid them. You may want to use a symptom diary or tracking app. Some of the most common include:
- **Diet. **Certain foods may trigger flares or worsen symptoms. Try to identify any foods that impact your ulcerative colitis.
- Medications. Pain relieving medications such as non-steroidal anti-inflammatories or antibiotics can worsen symptoms of ulcerative colitis
- Not taking medication as prescribed. Missing ulcerative colitis medications or taking an incorrect dose can lead to a flare-up.
- Stress. In some people, stress may impact ulcerative colitis symptoms.
What Happens If You Don’t Treat Colitis
Colitis is usually a temporary condition that resolves on its own in a few days to a week. It can, however, be a sign of a more serious condition such as ulcerative colitis, Crohns disease, autoimmune disorders, metabolic disorders, circulation problems, heart problems, or radiation injury. It can also be a sign of a serious infection, such as a potentially fatal E. coli gut infection or amoebic dysentery. If the symptoms become severe or last longer than a week, its time to talk to a doctor.
Recommended Reading: What Is A Gastric Ulcer And What Is Its Cause
What Causes Inflammatory Bowel Disease
It is not yet known exactly what causes Crohns disease and ulcerative colitis. These diseases seem to run in families, which means that genetics play a role. Many researchers believe that inflammatory bowel diseases are caused by a problem with the immune system. Normally, the immune system protects your body from infection. In people who have an inflammatory bowel disease, the immune system mistakes food, healthy bacteria, and other substances for an infection. This causes the immune system to attack the cells of the intestine, which leads to inflammation.
Dont Miss: How To Cure Gastritis And Ulcers Naturally
Dietary Recommendations For Ulcerative Colitis
There are different dietary recommendations for each stage of Ulcerative Colitis, active and remission. Recommendations mainly revolve around the amount of dietary fiber in your diet. During a flare its best to minimize the amount of fiber in your diet, whereas during remission fiber can be a beneficial part of your diet. Fiber is a tough nutrient for the gut to digest so during a flare, when the gut is already stressed, fiber can aggravate the symptoms of Ulcerative Colitis. Fiber also adds residue to stool, which should be avoided to allow the bowels to rest and heal. This is specifically true for insoluble fiber, which does not dissolve, and moves through your GI tract unchanged. Consuming fiber during a flare can increase bloating, gas, diarrhea, and abdominal pain, and may even lead to intestinal blockage.
Active
When UC is active, let your bowel rest as much as possible. Therefore, we recommend a low fiber, low residue diet:
- Low fiber fruit: bananas, cooked fruit, canned fruit
- Non-cruciferous vegetables: asparagus, potatoes, cucumbers, carrots
- Refined grain products: white pasta, white rice, white bread
- Lean protein: fish, chicken, lean pork, eggs, tofu
Recommended Reading: How Long Do Ulcers Take To Heal
What Does Having A Flare Mean
Asked by: Norris Lebsack
Answer: The definition of flare is a worsening of the disease process. If you have arthritis, you’ve probably experienced a flare at one time or another your disease seems to be well under control for a while, then suddenly your joints become inflamed and painful. You may experience general malaise and fatigue.
What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
Recommended Reading: How To Treat Oral Ulcers
How Do I Know If My Uc Has Gone Into Remission
UC doesn’t have a cure. Instead, the goal of any treatment plan is to send the disease into remission.
When UC is in remission, you don’t experience as many symptoms and start to feel better. If your UC medications and lifestyle changes work well for you, remission may last for months or even years. There are several different kinds of remission:
- Clinical remission: When a patient isn’t experiencing symptoms and may feel better.
- Endoscopic remission: Testing of the intestinal lining shows no inflammation
- Biochemical remission: Blood and stool tests show no sign of inflammation
- Surgical remission: When UC goes into remission after surgery to treat it
- Histologic remission: When both clinical and endoscopic tests didn’t show signs of UC
With UC, it can feel like life revolves around symptoms. If UC symptoms keep coming back, it can be a sign that medications aren’t working. Consider taking part in a clinical trial researching an investigational treatment option for people living with UC.
What Tea Is Good For Colitis
Teas high in antioxidants, such as green tea, may help reduce swelling and pain of the intestinal tissues. Colitis is often associated with an increase in substances, called reactive oxygen species , which easily react with oxygen and can damage tissues and worsen inflammation. Infections, ischemia , radiation, and inflammatory conditions all increase the amount of these substances. Antioxidants neutralize reactive oxygen species by reacting with them before they react with molecules in the bodys tissues, minimizing the damage they do. While reactive oxygen species do not cause colitis, they can make the condition more unpleasant.
Also Check: Wound Care Treatment For Diabetic Foot Ulcer
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you havent been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If youve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
Also Check: How To Cure Ulcerative Proctitis
When To Call Your Doctor About A Flare
Flares come with different levels of intensity. You may be able to manage a mild flare-up of symptoms on your own. But a more severe flare may be a warning sign of an ulcerative colitis complication that needs immediate attention.
Theodore J. Saclarides, MD, a colon and rectal surgeon at Rush University Medical Group in Chicago, suggests calling your doctor if you have any of these ulcerative colitis symptoms:
- Severe abdominal pain that lasts more than 24 hours
- A decrease in bowel movements along with abdominal pain
- Abdominal pain with a high fever
- Blood during a bowel movement that is too thick to see through
Editor’s Picks
Recommended Reading: Does Ulcerative Colitis Cause Hair Loss
Inflammatory Bowel Disease Treatment
The goal of treatment is to get rid of the inflammation that causes your symptoms. Many types of medicine can help reduce inflammation. Talk to your doctor about anti-inflammatory drugs and drugs that suppress the immune system. Some medicines are needed only during flare-ups. You may need long-term medicines to suppress your immune system. Depending on your symptoms, your doctor may also recommend these medicines and supplements:
- Vitamin supplements
In severe cases of inflammatory bowel disease, you may need to go to the hospital for intravenous fluids or surgery.
During your treatment, you will most likely be treated by a team of doctors. This team may include your family physician, a gastroenterologist , and, possibly, a surgeon.
Limit Your Fiber Intake
Fiber contributes to bowel regularity and bowel health, but too much fiber can also trigger UC flare-ups.
Try to stick to foods that have no more than 2 grams of fiber per serving. Low fiber foods include:
- refined carbohydrates such as white rice, white pasta, and white bread
- some cooked fruits
- juice with no pulp
Instead of eating raw vegetables, steam, bake, or roast your vegetables. Cooking vegetables results in some fiber loss.
Read Also: Best Probiotic For Stomach Ulcers
How To Stop Ulcerative Colitis Flare
Ulcerative colitis is a type of disease that leads to inflammation in the large intestine. This is one of the two main forms of inflammatory bowel disease the other being Crohns disease.
The inflammation along the gut lining seen in Ulcerative colitis can vary in severity and can appear at any point along the large bowel.
A key feature of Ulcerative colitis it presents as a relapsing and remitting disease. This is where symptoms reduce or disappear for a period of time. This can be followed by a flare-up where symptoms increase in severity.
How to stop or calm down Ulcerative colitis is an important part of its long-term management.
What Causes Ulcerative Colitis
The exact cause of ulcerative colitis is unknown. The following are factors that can contribute to the disease:
- Genetics: People who have first-degree relatives with UC are at increased risk of UC.
- Immune response: Autoimmune disorders can cause your immune system to attack the cells in your body instead of defending them.
- Environmental factors:
Read Also: How To Prevent Pressure Ulcers Nursing
Common Triggers Of Ulcerative Colitis Flare
The symptoms of ulcerative colitis flare-up are not pleasant and often force people to retreat socially. They fear being too far away from a washroom. How long do colitis flare-ups last? Ulcerative colitis flare-up duration can be a few days or several weeks. Sometimes, it depends on the trigger.
Here are some common triggers of the disease:
- Hormone fluctuations during pregnancy
Understanding the triggers and knowing how to stop a colitis flare-up gives those who are diagnosed with the disease the confidence to enjoy normal activities, including a full social life.
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
You May Like: When Does Ulcerative Colitis Start