Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Which Dressings Or Topical Agents Are The Most Effective For Healing Pressure Ulcers
Dressings and topical agents for treating pressure ulcers
Review question
We reviewed the evidence about the effects of dressings and topical agents on pressure ulcer healing. There are many different dressings and topical agents available, and we wanted to find out which were the most effective.
Background
Pressure ulcers, also known as bedsores, decubitus ulcers and pressure injuries, are wounds involving the skin and sometimes the tissue that lies underneath. Pressure ulcers can be painful, may become infected and affect peopleâs quality of life. People at risk of developing pressure ulcers include those with limited mobility â such as older people and people with short-term or long-term medical conditions â and people with spinal cord injuries. In 2004 the total yearly cost of treating pressure ulcers in the UK was estimated as being GBP 1.4 to 2.1 billion, which was equivalent to 4% of the total National Health Service expenditure.
Study characteristics
In July 2016 we searched for randomised controlled trials looking at dressings and topical agents for treating pressure ulcers and that gave results for complete wound healing. We found 51 studies involving a total of 2947 people. Thirty-nine of these studies, involving 2127 people, gave results we could bring together in a network meta-analysis comparing 21 different treatments. Most participants in the trials were older people three of the 39 trials involved participants with spinal cord injuries.
Key results
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Read Also: Treating Leg Ulcers With Sugar
Appendix 2 Glossary Of Nma Terms
Armspecific outcomes/armlevel data: raw outcome data or risk) for each arm of the trial .
Assumptions for NMA: in common with all metaanalysis, the true treatment effect across trials is assumed to be described by a fixedeffect or randomeffects model. Additionally, transitivity is assumed and, concurrently, exchangeability and consistency.
Baseline risk: the absolute risk of the outcome in the ‘control’ group. This is affected by the presence of prognostic factors. Some authors have used the baseline risk as a proxy effect modifier, but in general the effect estimate is independent of the baseline risk on the other hand, the absolute risk difference depends on baseline risk.
Bayesian approach: the explicit quantitative use of external evidence in the design, monitoring, analysis, interpretation of a healthcare evaluation. In the Bayesian paradigm, prior beliefs about parameters in the models are specified and factored into the estimation. Posterior distributions of model parameters are then derived from the prior information and the observed data. In NMA, it is common to use noninformative priors for effect estimates.
Coherence/consistency: the direct effect estimate is the same as the sum of the indirect effect estimates.
Contrast/comparison/studylevel data: outcome data for the comparison .
Credible interval : the 95% credible interval is the range within which the mean value lies with posterior probability of 95%.
Studylevel data: see contrast.
How Are Pressure Sores Diagnosed
Your doctor will do a physical exam to look at the sores. They will examine the size and depth of the sore and look to see if blood or fluid is oozing from the sore. Your doctor will check to see if your sore has a bad smell. They also will check for additional sores.
Testing may help to diagnose pressure sores or their complications. These tests might include a blood test. Another test would be to take a sample of the tissue from the sore. This is done by scraping or cutting it from the sore. That sample is sent to the lab for examination.
Don’t Miss: How Do I Know If I Have A Peptic Ulcer
Quality Of The Evidence
We have explored the application of a new approach to GRADE analysis, alongside NMA in STATA . We applied the GRADE approach separately to effect estimates for different contrasts and to the ranking of interventions, but the two aspects are closely interrelated and, in this review, are a consequence of the sparse network and the high risk of bias through much of the network. The effect estimates were exemplified by contrasts of interventions versus saline gauze.
Across the network as a whole, the evidence was of very low certainty. There was overall high risk of bias and overlap of the ranking probability distributions, and no clearcut results. The evidence was of such poor quality that we consider it inappropriate to focus on which treatments had the highest probabilities of healing .
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Don’t Miss: Food To Avoid For Ulcer Patient
What Are The Stages Of Pressure Sores
You may know pressure sores by their more common name: bed sores. They happen when you lie or sit in one position too long and the weight of your body against the surface of the bed or chair cuts off blood supply. You might get them if youre on bed rest or in a wheelchair.
Your doctor may talk about the stage of your pressure sores. The stages are based on how deep the sores are, which can affect their treatment.
If found early, there’s a good chance these sores will heal in a few days, with little fuss or pain. Without treatment, they can get worse.
ishonestNo.353 – Pores
You’ll know theyre better when the sore gets smaller and pink tissue shows up along the sides.
How Can I Tell If I Have A Pressure Sore
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
You May Like: What Are The Symptoms Of An Ulcer In Your Stomach
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
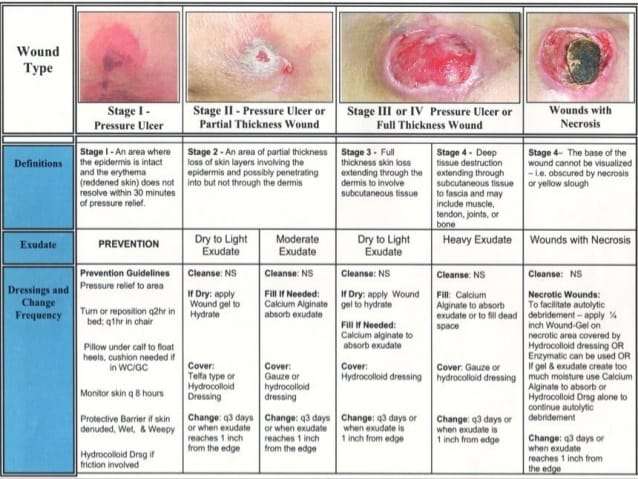
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Selecting The Right Medical Tape For Sacral Pressure Ulcers Management
While substantial guidance is available for dressing selection, most clinical guidelines fail to discuss the importance of medical tape in sacral ulcer management. Sacral ulcers pose unique challenges in wound management, and the medical tape must be up to the task. Sacral ulcers are often subjected to excessive moisture and soiling from perspiration, urine, and fecal matter. The sacral area is subject to substantial friction and shear forces, as well. Each time the patient repositions themselves , the sacral area takes the brunt of this movement. Lastly, the sacral region is not uniform in shape. And sacral ulcers also tend have irregular borders. Dressings must be cut to fit the wounds, and tape must be able to provide a secure border on all sides.
If you care for someone who has or is at risk for sacral pressure ulcer, contact Hy-Tape for free sample.
References
1. Therattil PJ, Pastor C, Granick MS. Sacral pressure ulcer. Eplasty. 2013 13:ic18-ic18.
2. Bryant R, Nix D. Acute and chronic wounds: Current management concepts. Elsevier Health Sciences 2015.
Read Also: L Glutamine Ulcerative Colitis Dosage
Stages Of Pressure Ulcers And Treatment
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
Living With Pressure Sores
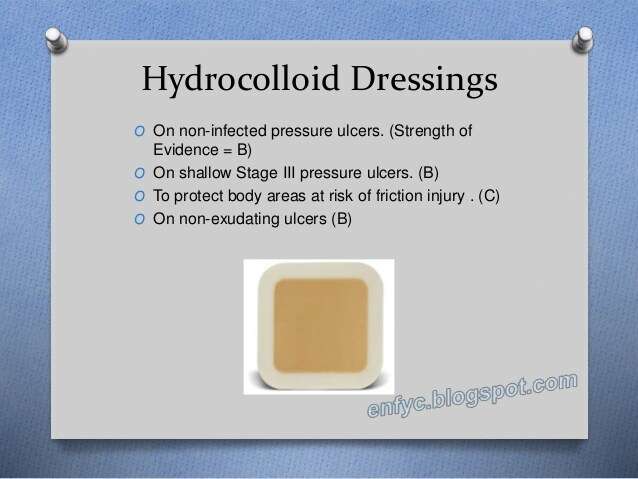
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Also Check: Can Diverticulitis Cause Ulcerative Colitis
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
Management Of Sacral Ulcers Varies By Ulcer Stage
It is important to properly stage pressure ulcers for several reasons, but two of the most important are for prognosis and management planning. Stage 1 and stage 2 pressure ulcers heal by regenerating tissue in the wound. Stage 3 and stage 4 pressure ulcers, on the other hand, heal through scar formation, which means the borders of the wound contract as it heals.
For Stage 1 sacral ulcers, the primary goal of therapy is to ensure adequate tissue perfusion and to protect the wound from further damage.2 This means preventing the sacrum from chronically squeezing the skin and preventing blood flow to the area. The goal of therapy for Stage 2 ulcers is to encourage tissue regeneration and protect the wound surface. For stage 3 or 4 ulcers, management efforts are focused on promoting tissue granulation and epithelialization.
You May Like: Wound Care Treatment For Diabetic Foot Ulcer
Pressure Ulcers: Debridement And Dressings
- Charles F von Gunten MD
- Frank Ferris MD
Background Fast Fact #40 discussed the staging and prevention of pressure ulcers this Fast Fact discusses their management. The first step in deciding how to manage pressure ulcers is an assessment of whether the wound is likely to heal. If the patient has a prognosis of months to years, adequate nutrition, and blood flow to the tissue, then healing is possible. If the patient has a prognosis of days to weeks, anorexia/cachexia, and/or the wound has inadequate perfusion, then symptom control alone is appropriate and uncomfortable/burdensome treatments are not appropriate.
Debridement Always provide adequate analgesia! Necrotic tissue must be removed for ulcer healing surgical debridement is the fastest and most effective method when there is healthy surrounding tissue. Note: If the patient is close to dying, and/or the wound will never heal, then debridement should not be attempted. Debridement gels are applied onto an ulcer under an occlusive dressing , are available for ulcers that do not require surgery or when surgical debridement is incomplete. These products come with or without enzymes to encourage autolytic or enzymatic debridement. For minimally necrotic ulcers, occlusive dressings such as DuoDerm, changed weekly, promote autolysis.
References
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
Read Also: Can I Eat Oatmeal With Ulcerative Colitis