Description Of The Intervention
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
-
absorb and contain exudate without leakage or strikethrough, in order to maintain a wound that is moist but not macerated
-
achieve freedom from particulate contaminants or toxic chemicals left in the wound
-
provide thermal insulation, in order to maintain the optimum temperature for healing
-
allow permeability to water, but not bacteria
-
optimise the pH of the wound
-
minimise wound infection and avoid excessive slough
-
avoid wound trauma on dressing removal
-
accommodate the need for frequent dressing changes
-
provide pain relief and
-
be comfortable.
There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.
Absorbent dressings are applied directly to the wound and may be used as secondary absorbent layers in the management of heavily exuding wounds. Examples include Primapore , Mepore and absorbent cotton gauze .
Topical agents
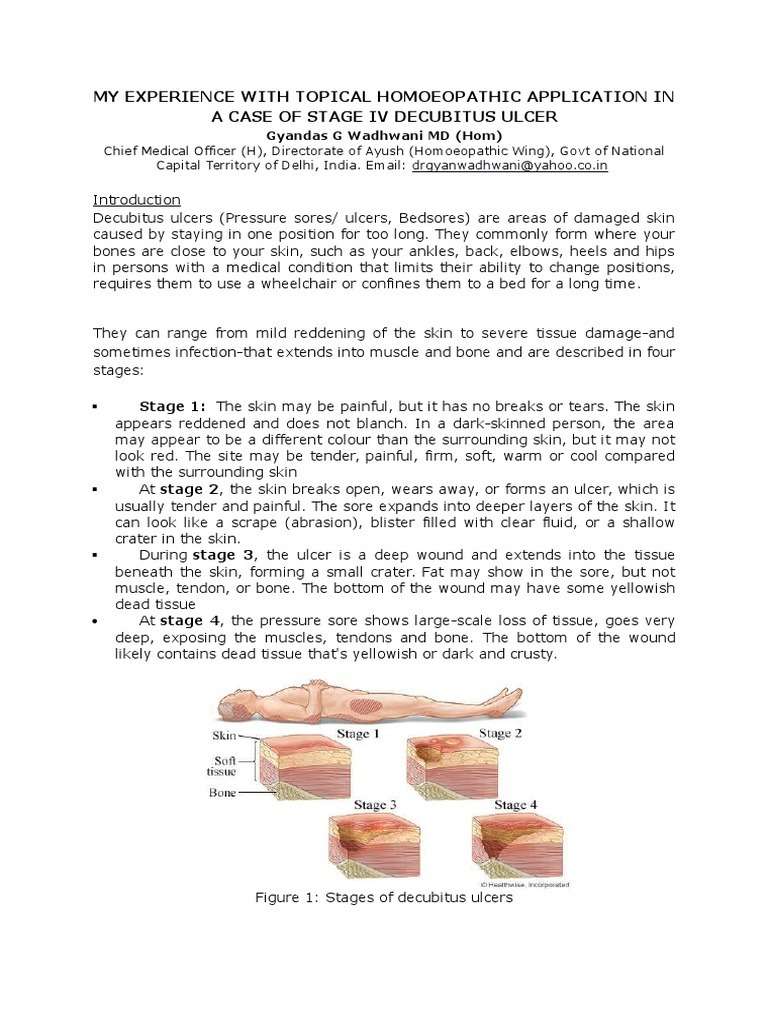
Stage Iii And Iv Ulcers Full Thickness Skin Loss With Visible Underlying Tissues
Full thickness decubitus ulcers have underlying muscle, bone and/or adipose tissue visible and typically require highly absorbent dressings to manage exudate. Hydrofiber dressings are made from soft, absorbent material that transforms into a gel when it comes in contact with wound drainage. This gelling action traps bacteria and maintains optimal levels of moisture within the wound for healing. Calcium alginate dressings are made from seaweed fibers that have been formed into a loose fleece. The fibers are entangled so that the dressing becomes stronger when it becomes soaked with blood or drainage. Calcium alginate sheets can be placed on surface wounds while ribbons are used to pack deep tunneling ulcers. Both hydrofiber and calcium alginate dressings require a secondary dressing to hold them close to the wound bed .
Common Causes For Decubitus Ulcer
Shearing and Friction: If a bedridden person is pulled or dragged from his or her bed it causes friction and stretches the skin muscles. Blood circulation of the skin gets marred which causes the damage.
Moisture: Skin is very sensitive at this stage. Perspiration, bed-wetting or feces leads to furthermore chances of bed sores.
Lack of Movement: People, who have been bedridden for a prolonged period of time due to severe medical conditions, bear the brunt. Being in a same position without any movement is one of the main reasons for bed sores.
Lack of Nutrition: A good diet can help you fight this condition easily. Due to lack of proteins, vitamins and other required substances in the body, the patient suffers moreover.
Age: An elderly person is mainly affected because youth is not on his side. The thin skin and failing bodily functions deteriorates the chances of revival.
Lack of Sensation: An injury which leaves you without sensation is another reason for bed sores. This lack of sensation does not allow you to determine the immensity of the pressure applied on the skin.
Also Check: Best Way To Heal Stomach Ulcers
Overall Completeness And Applicability Of Evidence
The network is sparse, in terms of the total number of participants, the total number of wounds healed, the number of studies per contrast, the size of the constituent studies and the duration of followup: 21 of 27 direct contrasts were informed by only one study and the average number of events per mixed treatment contrast was around four. The median study size was 41 and several studies had zero events. The duration of followup was relatively short for most studies : only 3/39 studies in the network had a followup duration of 16 weeks or more.
In parallel we conducted a second NMA, grouping together some classes of dressings. We had hoped that the group network would provide more power in the analysis, but in practice too many data were excluded from the network, and the network was also unbalanced, being dominated by the advanced dressing versus basic dressing contrast, which involved about 55% of the participants in the group network. The group network provided equally uncertain evidence and the findings are not discussed further here, but are reported in for the interested reader.
Risk Of Bias In Included Studies
Risk of bias for all included studies is summarised in . In order to represent ‘very high’ risk of bias, we have used two columns so very high risk of bias occurs when the cell is red in the final column .
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
We judged only one of the 51 studies to be at low risk of bias and ten to have unclear risk of bias . We judged 14 studies to be at very high risk of bias, that is, to have high risk of bias for two or more domains . We assessed the rest of the studies at high risk of bias. We grouped the low and unclear categories together.
*Studies marked with an asterisk were not included in the individual network.
Also Check: Can Food Allergies Cause Ulcerative Colitis
Nma Of Treatments For Healing Pressure Ulcers
We found 51 randomized trials, and 39 could be linked to form a network joining 21 treatments in about 3000 participants . There were 13 different dressings and 6 topical agents and 2 other linking interventions .
We got results for 210 comparisons covering every pair of treatments and were also able to obtain the rank order of treatments .
To make interpretation easier, we focused on the results for the 20 comparisons with saline gauze, and the rank order of all the treatments in the network for healing.
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
Don’t Miss: Venous Leg Ulcer Dressing Treatment
Was The Treatment Allocation Adequately Concealed
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation sequentially numbered drug containers of identical appearance sequentially numbered, opaque, sealed envelopes.
High risk of bias
Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on using an open random allocation schedule assignment envelopes were used without appropriate safeguards alternation or rotation date of birth case record number any other explicitly unconcealed procedure.
Unclear risk of bias
Insufficient information provided to permit judgement of low or high risk of bias. This is usually the case if the method of concealment is not described or is not described in sufficient detail to allow a definitive judgement, for example if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed.
Dressings And Topical Agents To Treat The Pressure Ulcers
Bedsores are injuries of the skin and underlying tissue, resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as heels, ankles, hips and tailbone.
The most common sites are: sacrum, coccyx, heels, hips, elbows, knees, ankles, back of shoulders and the back of the cranium. For people who use a wheelchair, pressure sores often occur on skin over the following sites: tailbone or buttocks, shoulder blades and spine, back of arms and legs Pressure ulcers have a large impact on those aJected the ulcers can be painful and may become seriously infected or malodorous. There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.Classification:
You May Like: Natural Enemas For Ulcerative Colitis
Risk Factors For Decubitus Ulcer
The following are the risk factors for decubitus ulcer:
In older persons with functional limitations :
Facility dependent factors
Deep tissue involvement with SIRS,osteomyelitis and/or threat to limb or life
- Clindamycin plus ceftriaxone
- Clindamycin plus gentamicin
- Vancomycin
- Given for 2-12 weeks prolonged oral treatment required for bone and joint infections after initial intravenous therapy
Summary Of Main Results
We have successfully conducted a network metaanalysis of dressings and topical agents for healing pressure ulcers. Alongside the analysis we have applied a new method of GRADE assessment , which allows us to view the results in the light of our certainty in their findings. Using this approach, we found the majority of the evidence to be of low or very low certainty, and was mainly downgraded for risk of bias and imprecision . This level of uncertainty within the totality of the dataset impacts on all subsequent interpretation of its outputs.
This review includes 51 RCTs involving a total of 2964 participants, comparing 39 different dressings or topical agents for the healing of pressure ulcers. Most of the studies were in older participants, but four included participants with spinal cord injuries and one was in younger people said to be chronically ill or physically disabled. Seventeen studies included participants mainly with Stage 2 pressure ulcers and 15 mainly had Stage 3 pressure ulcers 13 studies investigated treatment of ulcers with a mean duration of less than three months.
We treated each topical agent as a separate intervention, but initially grouped dressings by class as described in the . The network involved 39 studies in 2116 participants, encompassing 21 different interventions in 27 direct contrasts and these informed 210 mixed treatment contrasts.
Recommended Reading: Stomach Ulcer And Weight Loss
Stage 4 Pressure Ulcers
- Helps to prevent biofilm formation
- Reduces healing time
It moistens wound dressings and dissolves encrusted bandages or wound dressings during dressing changes.
Prontosan® Gel X proper wound cleansing is essential. The use of Prontosan® Wound Gel X provides long-lasting cleansing and decontamination of the wound bed between dressing changes.
Prontosan® Debridement Pad has been designed to support the wound bed preparation when used in conjunction with Prontosan® Wound Irrigation Solution.
Was The Allocation Sequence Randomly Generated
Low risk of bias
The investigators describe a random component in the sequence generation process, such as referring to a random number table using a computer random number generator tossing a coin shuffling cards or envelopes throwing dice drawing of lots.
High risk of bias
The investigators describe a nonrandom component in the sequence generation process. Usually, the description would involve some systematic, nonrandom approach, for example sequence generated by odd or even date of birth sequence generated by some rule based on date of admission sequence generated by some rule based on hospital or clinic record number.
Unclear risk of bias
Insufficient information about the sequence generation process provided to permit judgement of low or high risk of bias.
Also Check: Does Ulcerative Colitis Make You Tired
Criteria For Considering Studies For This Review
Types of studies
We included published and unpublished randomised controlled trials , irrespective of language of report. We did not identify any crossover trials, but we would have included them only if they reported outcome data at the end of the first treatment period and prior to crossover. We excluded studies using quasirandom methods of allocation . We highlighted trials in which three or more interventions were randomised.
Types of participants
We included studies that recruited people with a diagnosis of pressure ulcer, Stage 2 and above , managed in any care setting. We excluded studies that only recruited people with Stage 1 ulcers as these are not open wounds requiring dressings.
We accepted study authors’ definitions of what they classed as Stage 2 or above, unless it was clear that they included wounds with unbroken skin. Where authors used grading scales other than NPUAP, we attempted to map to the NPUAP scale.
Types of interventions
Interventions of direct interest
The interventions in this section were all those that can be directly applied as dressings or topical agents to open pressure ulcers. We presented results for these interventions and included them in summary tables. In the context of a network of competing treatments, there are no ‘comparators’.
Some of the interventions we considered were as follows:
Supplementary intervention set
Terminology
Types of outcome measures
Primary outcomes
-
the proportion of wounds healed
-
time to complete healing .
Stage 2 Pressure Ulcers
- Helps to prevent biofilm formation
- Reduces healing time
It moistens wound dressings and dissolves encrusted bandages or wound dressings during dressing changes.
Prontosan® Gel X proper wound cleansing is essential. The use of Prontosan® Wound Gel X provides long-lasting cleansing and decontamination of the wound bed between dressing changes.
Prontosan® Debridement Pad has been designed to support the wound bed preparation when used in conjunction with Prontosan® Wound Irrigation Solution.
You May Like: Is Green Tea Good For Ulcers
How The Intervention Might Work
Animal experiments conducted over 40 years ago suggested that acute wounds heal more quickly when their surfaces are kept moist rather than left to dry and scab . A moist environment is thought to provide optimal conditions for the cells involved in the healing process, as well as allowing autolytic debridement , which is thought to be an important part of the healing pathway .
The desire to maintain a moist wound environment is a key driver for the use of wound dressings and related topical agents. Whilst a moist environment at the wound site has been shown to aid the rate of epithelialisation in superficial wounds, excess moisture at the wound site can cause maceration of the surrounding skin , and it has also been suggested that dressings that permit fluid to accumulate might predispose wounds to infection . Wound treatments vary in their level of absorbency, so that a very wet wound can be treated with an absorbent dressing to draw excess moisture away and avoid skin damage, whilst a drier wound can be treated with a more occlusive dressing or a hydrogel to maintain a moist environment.
Some dressings are now also formulated with an ‘active’ ingredient .
Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin < 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
Recommended Reading: Foam Dressings For Pressure Ulcer Prevention
Essentials Of Decubitus Ulcer Care
Risk Assessment
1. Consider all bed- or chair-bound persons, or those whose ability to reposition is impaired, to be at risk for pressure ulcers.
2. Select and use a method of risk assessment, such as the Norton Scale or the Braden Scale, that ensures systematic evaluation of individual risk factors.
3. Assess all at-risk patients at the time of admission to health care facilities and at regular intervals thereafter.
4. Identify all individual risk factors to directspecific preventive treatments. Modify care according to the individual factors for proper Decubitus Ulcer Care.
Nutritional status
Malnutrition is frequently cited as a risk factor for the presence, development and non-healing of Decubitus Ulcers. Nutritional status influences the integrity of the skin and support structures, and a lack of vitamins and trace elements may predispose the patient to increased risk of pressure damage. Emaciated and obese people have also been associated with being at a higher risk.
Best practice entails monitoring the nutritional status of individuals as part of a holistic assessment procedure and as an ongoing process throughout an individuals episode of care. Initially, this assessment should include documentation and monitoring of the following factors for proper Decubitus Ulcer Care:
- current weight and height
- usual eating habits
- recent changes in eating habits and intake.
Skin Care and Early Treatment
5. Avoid massage over bony prominences.
Education
2. Include information on:
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
Recommended Reading: Best Thing To Take For Stomach Ulcer Pain