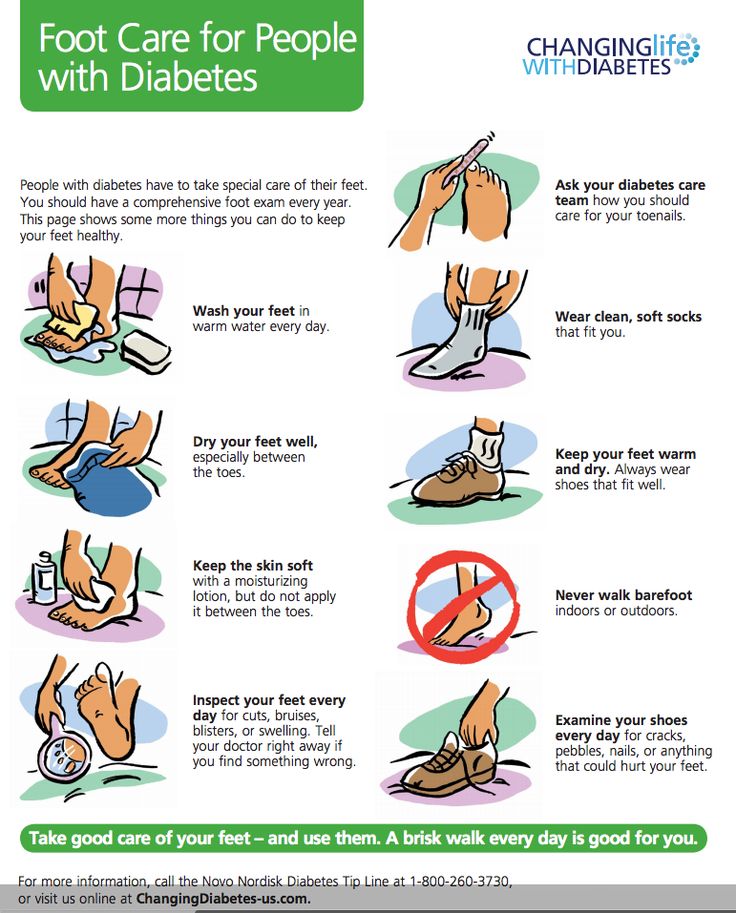
Tip #: Wear Shoes That Fit Properly
“Don’t just go out and buy random shoes,” she warns. Wearing shoes that are ill-fitting or put a lot of pressure on your foot may result in a pressure ulcer. If you don’t know your correct shoe size, have a professional assist you.
You should also steer clear of shoes with pointed or open toes, such as high heels, flip-flops or sandals. Also, wear shoes made of breathable fabrics, like canvas, leather or suede.
- Related post:Foot Problems? Swap Your Shoes
Peripheral Arterial Occlusive Disease
Peripheral arterial occlusive disease is four times more prevalent in diabetics than in non-diabetics.11 The arterial occlusion typically involves the tibial and peroneal arteries but spares the dorsalis pedis artery.12 Smoking, hypertension and hyperlipidemia commonly contribute to the increased prevalence of peripheral arterial occlusive disease in diabetics.13,14
The presence of lower extremity ischemia is suggested by a combination of clinical signs and symptoms plus abnormal results on noninvasive vascular tests. Signs and symptoms may include claudication, pain occurring in the arch or forefoot at rest or during the night, absent popliteal or posterior tibial pulses, thinned or shiny skin, absence of hair on the lower leg and foot, thickened nails, redness of the affected area when the legs are dependent, or dangled, and pallor when the foot is elevated.
The sensitivity and specificity of noninvasive vascular tests are a matter of some controversy. Commonly accepted abnormal values for transcutaneous oxygen measurement, ABI determinations and toe systolic pressure are given in Table 2. The noninvasive tests have been faulted for underestimating the severity of arterial insufficiency.18 If lower extremity ischemia is strongly suspected, arteriography or some other imaging study should be performed to confirm or rule out ischemia.
|
Less than 40 mm Hg |
|
Ankle-brachial index |
Why Is Foot Ulcers Healing Slow
When you have diabetes, several factors can affect your bodys ability to heal ulcers. A diabetic foot ulcer has various causes, often including external ischemia, neuropathy, or both. A few of them include:
- High blood sugar levels
- Immune system deficiency
If you get an ulcer or notice any change in your skin that youre unsure about, consult a doctor, could be a primary doctor or a diabetes specialist. A debridement procedure will be given to the infected area, removing unhealthy tissue from the wound to spur healing. The doctor will also work with you to keep your sore or ulcer from getting infected and becoming more significant.
If the foot ulcer doesnt heal within a month or the infection spreads to the bone, in this case, patients may need other treatments. These can include surgery and hyperbolic oxygen therapy to help the body heal.
Donât Miss: Boost Vs Ensure Ulcerative Colitis
Also Check: Pain Medicine For Ulcerative Colitis
How To Treat Ulcers
If you do get an ulcer or notice a change in your skin that youâre not sure about, tell your doctor right away. Youâll likely get a procedure called debridement, which removes unhealthy tissue from the wound to spur healing.
Your doctor will also work with you to try to keep your sore or ulcer from getting infected and becoming bigger. Some of the steps they may recommend include:
Clean your ulcer daily. Use soap and water, unless your doctor recommends another cleanser. Donât use hydrogen peroxide or soak your wound in a bath or whirlpool, because this could reduce healing and may boost your odds of infection.
Keep your ulcer bandaged or covered with a wound dressing. While you may have heard that itâs important to âair outâ wounds, experts now know that not covering a wound actually increases the odds of infection and slows healing.
Keep pressure off your ulcer, especially if itâs on your foot. This may mean you need to use crutches, special footwear, a brace, or other devices. Reducing pressure and irritation helps ulcers heal faster.
Use the topical medications your doctor recommends. These may be saline, growth factors, and/or skin substitutes.
Keep your blood sugar under control. In addition to reducing your risk of ulcers, tight blood sugar control helps your body heal existing ulcers.
Zinc To Speed Up The Healing
Zinc-rich foods like eggs, nuts, and legumes can prove to be very beneficial for both your diabetes and diabetic foot ulcers. Zinc promotes the production and secretion of insulin in the body and thus helps to keep blood sugar levels in check. Zinc also hastens the healing of the wound by maintaining the structural integrity of the dermal tissue.
Read Also: Foods To Avoid With Bleeding Ulcer
Keep Your Wound Clean And Covered With The Right Dressings
Wounds heal best when they are clean and moist. So its important to get them clean and covered right away. If you have a new scrape or cut, a basic bandage and antibiotic cream should work just fine.
But if you have wounds that are infected, slow healing or more serious, make an appointment with a doctor to learn what the best wound care is for you. Your doctor will likely recommend different types of diabetic wound care dressings to protect the injury and promote healing.
Common types of dressings for diabetic wound care
- Foam dressings Extremely soft and absorbent, foam dressings are used for wounds that leak or ooze a lot. They also offer added cushioning which can help protect the wound against physical damage.
- Alginate dressing These types of dressings are primarily made from seaweed. They can hold up to twenty times their weight in moisture, making them a great choice for deep wounds and ones with discharge. Another advantage of alginate dressings is that they prevent the growth of new bacteria.
- Hydrogel dressings Hydrogel is a water-based gel designed to keep an area moist. If your wound is dry or covered in dead skin, your doctor may recommend a hydrogel dressing to provide moisture. This can help break down dead tissue and promote cell growth. These types of dressings usually arent used for infected wounds.
Caring For Wounds And Foot Ulcers In Diabetic Patients
The Centers for Disease Control and Prevention reports that there are 30.3 million people living with diabetes in the United States. Diabetes comes with many serious complications, including chronic wounds, nerve damage and foot ulcers.
The American Podiatric Medical Association reports that 15 percent of diabetic patients will develop a foot ulcer. Further, diabetes is the leading cause of nontraumatic, lower-extremity amputations in the U.S. caused by infected wounds and foot ulcers that cannot heal. While difficult to treat, foot ulcers often can be prevented.
Controlling risk factors and monitoring the skin daily is key to minimizing the negative effects of diabetes, said Nancy Estocado, Advanced Wound Care Clinical Coordinator at Sunrise Hospital and Medical Center. For anyone with diabetes, understanding how to prevent and properly address wounds especially foot ulcers is integral to living a healthy life.
You May Like: Foods For Gerd And Ulcers
Treatment For Vascular Ulcers
Its important to note that not all skin ulcers are caused by diabetes, and that even people who dont have diabetes can suffer from chronic wounds. Even people without diabetes can be susceptible to vascular ulcers. Vascular ulcers are caused by problems with the vascular system .
These types of ulcers can happen to people who suffer from veins or arteries that dont function properly, causing blood flow in the legs to be limited. This can lead to an increased risk of wounds that may not heal normally and can become infected.
The Wound Care Center at Harrington also provides full service care for these types of wounds, including on-site X-rays, MRI and lab work.
To make an appointment at the Harrington Wound Care Center, call 248-8105. You can also learn more on our website here.
Coordinated Specialized Care Through A Dedicated Institute
Our orthopaedic specialists work together through our dedicated Penn State Bone and Joint Institute. There, they focus on providing you with multidisciplinary, tailored care and state-of-the-art treatments and technologies. This produces the highest-quality patient outcomes. All physicians at the institute are fellowship-trained and subspecialize in additional niche areas of orthopaedics, including arthritis care and joint arthroplasty .
Also Check: Stage 2 Pressure Ulcer Treatment Dressing
Taking Pressure Off Your Foot Ulcer
Foot ulcers are partly caused by too much pressure on one part of your foot.
Your provider may ask you to wear special shoes, a brace, or a special cast. You may need to use a wheelchair or crutches until the ulcer has healed. These devices will take the pressure off of the ulcer area. This will help speed healing.
Sometimes putting pressure on the healing ulcer for even a few minutes can reverse the healing that happened the whole rest of the day.
Be sure to wear shoes that do not put a lot of pressure on only one part of your foot.
- Wear shoes made of canvas, leather, or suede. Don’t wear shoes made of plastic or other materials that don’t allow air to pass in and out of the shoe.
- Wear shoes you can adjust easily. They should have laces, Velcro, or buckles.
- Wear shoes that fit properly and are not too tight. You may need a special shoe made to fit your foot.
- Don’t wear shoes with pointed or open toes, such as high heels, flip-flops, or sandals.
Diabetic Foot Ulcer Symptoms
Normally a wound or sore on the skin would cause pain. But the same loss of feeling in the feet that often contributes to the development of a diabetic foot ulcer means that theres often no pain associated with the ulcer. This can make it difficult for people to realize that an ulcer is even there in the early stages, when treatment is most effective.
Aside from pain, another sign to look for is discharge or drainage from the wound in the socks. Ulcers that have been present for some time and that have become infected may also cause an unpleasant odor.
Read Also: What Do I Take For An Ulcer
Tip #: Dont Walk Around Barefoot
Get Help Now:TriHealth Wound Healing
This is especially important for people who have diabetic neuropathy, which is nerve damage in the body that develops from high blood sugar levels caused by diabetes. Ive had patients step on needles and hard objects, metals impregnated into their foot, and theyll never know, Dr. Masturzo points out.
Its Been Longer Than Four Weeks
If wounds dont heal within a month, they are considered chronic wounds. While its possible for chronic wounds to heal on their own, its best to get a doctors help to identify why the wound isnt healing and provide treatment.
Our Wound Healing Center offers advanced treatments for severe and chronic diabetic wounds
Read Also: Icd 10 Stage 3 Pressure Ulcer Sacrum
Wound Care And Dressings
Care for your wound as instructed by your provider. Other instructions may include:
- Keep your blood sugar level under good control. This helps you heal faster and helps your body fight infections.
- Keep the ulcer clean and bandaged.
- Cleanse the wound daily, using a wound dressing or bandage.
- Try to reduce pressure on the healing ulcer.
- Do not walk barefoot unless your provider tells you it is OK.
Find And Treat Cuts Scrapes And Other Wounds Immediately
If you treat new wounds right away, you can start caring for them before things get bad. So as soon as you find a cut or sore:
Of course, if you dont know you have a wound, you cant treat it quickly. So if you suffer from neuropathy, keep an eye out for new wounds. Check your hands and feet daily, and dont forget to check between your toes.
Wearing white socks can help, too. If you see a red spot or a place where your sock is sticking to your skin, check your foot to see if you have a wound thats new or not healing.
Read Also: Can Ulcers Give You Headaches
Diabetic Foot Ulcer: Treatment And Prevention
Estimates are that by 2030 there will be 550 million individuals with diabetes in the world. Because almost a quarter of all people with diabetes will develop a foot ulcer at some point, health care workers need to know the best practices for diabetic foot ulcer prevention and treatment.
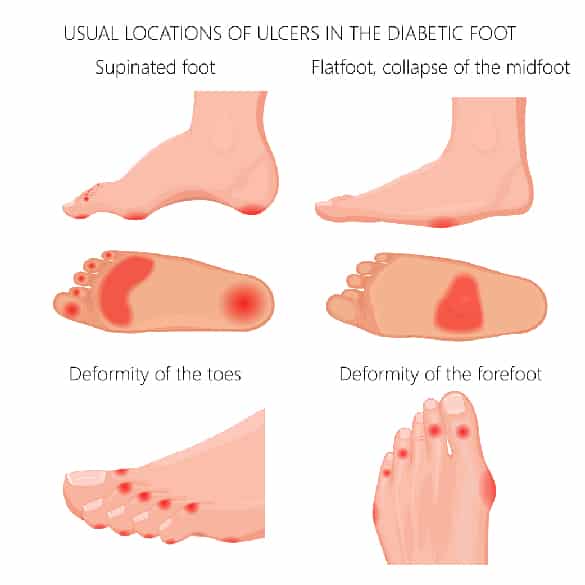
Determining which diabetic foot ulcer type is important to determine an effective treatment. Here are the different types of these wounds:
- Neuropathic ulcers arise when the nerve damage from diabetic neuropathy causes the individual with diabetes to not feel pain from an injury, which often leads to the ulcer progressing substantially before the person is even aware of it. Foot and toe deformities, corns, calluses and areas repetitive stress are likely places of injury. Footwear can not only hide these issues, but can exacerbate the injury if the shoe is ill-fitting.
- Ischemic ulcers or arterial ulcers as they are sometimes called may occur due to lack of blood flow to the extremity. When an ulcer occurs as the result of an injury to the extremity, the lack of blood flow makes these ulcers difficult to heal.
- Neuroischemic ulcers occur in individuals with both neuropathy and poor arterial blood flow and are the most difficult to heal.
- Infected wounds occur in about half of patients with a diabetic foot ulcer and require particularly close care.
Research Design And Methods
The precise date of ulcer onset is often difficult to determine, especially for those ulcers that are long established or of which the patient was unaware. It was for this reason that a prospective decision had been taken to document ulcer onset simply by calendar month. For the purposes of calculating the ulcer duration at referral, the date of onset was taken as the 15th day of that month. For ulcers that started in the same month that they were first seen, the date of onset was taken as the 15th day of the month if they were seen after that date. For ulcers first seen in the first half of the month of onset, ulcer duration was arbitrarily taken as 7 days.
Usual clinical management for neuropathic ulcers relies on regular debridement to remove surrounding callus, combined with offloading. The principle of offloading was to adjust footwear to ensure that continued trauma to the ulcerated area was minimized, but the method adopted had to comply with that which was both safe and acceptable to each patient. The method of choice of offloading of neuropathic ulcers on the plantar surface of the foot was the use of irremovable padded fiberglass slippers and, less frequently, with below-the-knee irremovable casts. Patients who were judged unsafe in casts, or who refused to wear them, were managed with removable orthoses , with the aim of achieving the most effective offloading practicable.
Read Also: How Can Ulcers Be Treated
Etiology Of Foot Ulceration
The etiology of diabetic foot ulcers usually has many components.4,7 A recent multicenter study8 attributed 63 percent of diabetic foot ulcers to the critical triad of peripheral sensory neuropathy, trauma, and deformity. Other factors in ulceration are ischemia, callus formation, and edema. Although infection is rarely implicated in the etiology of diabetic foot ulcers, the ulcers are susceptible to infection once the wound is present. Many of the risk factors for foot ulcer are also predisposing factors for amputation, because ulcers are primary causes leading to amputation.5,7,9 Recognized risk factors for diabetic foot ulceration are listed in Table 1.4
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
What Types Of Physicians Specialize In Treating Diabetic Foot Ulcers
The doctors that are qualified to treat diabetic foot ulcers include wound care specialists, orthopedic surgeons, vascular surgeons, and endocrinologists.
- Wound care specialists are clinicians who have received specialized training in caring for and treating all wounds, both acute and chronic. One of the most treated wounds are diabetic wounds. The percentage of these wounds that become stubborn and refuse to heal is high. This creates an issue with the patients quality of life.
- Podiatrists are foot health specialists who are specially trained in treating all injuries and illnesses pertaining to the feet, including the diagnosis and treatment of diabetic ulcers.
- Orthopedic surgeons can offer prevention measures to patients who have diabetic foot ulcers. Long-term protection of the feet is provided to patients by Orthopedists subscribing footwear that will protect them in the future. The surgeon can also correct bunions, hammertoes, and deformities in the feet to avoid the formation of an ulcer.
- A vascular surgeon does not directly treat diabetic foot ulcers. They are involved in the treatment of peripheral arterial disease, which is a critical catalyst for the impediment of blood flow to the lower legs and feet.
- Endocrinologists are specially trained physicians who address several conditions, including diabetes. An endocrinologist will be the doctor who will make referrals to the other specialists mentioned here.
Recommended Reading: Does Type 2 Diabetes Need Insulin
Recommended Reading: Symptoms Of A Bleeding Ulcer In Your Stomach
What Are Neurotrophic Ulcers
Neurotrophic ulcers occur primarily in people with diabetes, although they can affect anyone who has impaired sensation in their feet. They can be found anywhere on your feet, but they usually develop on the parts of your feet and toes that are most sensitive to weight .
Neurotrophic ulcers dont cause pain. But they can be serious if they arent treated promptly or they dont respond to treatment.
A neurotrophic ulcer might be the following colors:
- Any combination of those colors.
The thin borders of the ulcers are punched out, meaning that theyre taller than the surrounding tissues.