What Causes Ulcerative Colitis Vs Crohns Disease
Its not entirely known what causes ulcerative colitis or Crohns disease. However, experts believe it has something to do with genetic factors and environmental factors . Your gut microbiomethe bazillion bacteria that live in your digestive tractis thought to have influence as well. In fact, a 2020 study published in the journal Frontiers of Medicine, found that not only was the gut bacteria in people with IBD different from people without IBD, but it was also different between people with ulcerative colitis vs. people with Crohns disease.4
What is known is that something sets off your immune system to mistakenly attack healthy areas of your digestive tract, causing chronic inflammation.
This overreaction of the immune system can also affect areas outside of your digestive system and can include your skin, eyes, and other organs. This can occur with both ulcerative colitis and Crohns disease, but ulcerative colitis is more likely to affect the skin, eyes, and bones, while Crohns disease is more apt to affect the kidneys and gallstones.1
Read Also: What Is Good For Ulcers
Infectious Colitis And Cord Colitis
Infectious colitisdue to a variety of agentsmay clinically mimic UC. However, most cases of infectious colitis demonstrate a histological pattern of acute colitis, which may be diffuse, patchy, or focal, without evidence of chronicity, as evidenced by architectural distortion . Less commonly, chronic infectious colitis may produce a histological pattern of chronic active colitis resembling IBD. Most cases of infectious colitis with the chronic active colitis pattern have no specific diagnostic features on histological examination in such cases, knowledge of the clinical history and correlation with serologic studies or stool cultures are required for diagnosis. However, an important exception is amoebic colitis, in which trophozoites of entamoeba histolytica may be observed in biopsy material showing features of chronic active colitis . Amoebae should always be excluded in biopsies of suspected IBD, as these organisms may not be identified by routine stool studies and because immunosuppressive therapy for presumed IBD may result in fulminant amoebic colitis with perforation .
Amoebic colitis may mimic ulcerative colitis by a manifestation of chronic active colitis with crypt distortion, mild basal lymphoplasmatocysis , and epithelial injury . However, trophozoites of entamoeba histolytica are evident on high magnification .
Read Also: Symptoms Of Crohns Vs Ulcerative Colitis
How Can I Cure Ibs Permanently
There is no permanent and medically known cure for IBS, but there are several tips that serve as treatment options to alleviate or get rid of the symptoms. Lifestyle tips include dietary modifications, high fiber diet , physical exercise, stress management and prescription medications. There is no specific diet for irritable bowel syndrome, and different individuals react differently to different foods.
Also Check: Colon Cancer Symptoms Vs Ulcerative Colitis
What Are The Causes And Symptoms Of Collagenous Colitis
Collagenous colitis is caused by swelling and inflammation due to inflammatory cells traveling to the large, and sometimes small, intestine. If your large intestine is unable to properly reabsorb water, it causes the symptoms of collagenous colitis.
There are many factors that can contribute to collagenous colitis including a potential reaction to bacteria, pollen, or food. Certain medications may be triggers for CC, a list that includes nonsteroidal anti-inflammatory drugs antacids antidepressants diabetes medication and cholesterol medication. Continue reading
Recommended Reading: Foods To Eat To Help Ulcers
What Life With Chronic Intestinal Pseudo Obstruction Is Actually Like
This is reality. I drove my car for the first time since June a few days ago. I had to drive 5 hours to Michigan to see my doctor. Just doing that simple thing has wiped me out. I slept until almost 2PM the day after I got back to Illinois and Ive been running a slight temperature and feel overall awful. My nausea has been a lot worse the past month or two but we switched my nausea med to the IV version so hopefully that will help.
Living with the rare disease, CIPO and Intestinal failure caused by CIPO is difficult. Like really, really difficult. Normally if a patient comes into the ER with extremely dilated loops of bowel with air fluid levels and has symptoms of severe pain, nausea, and vomiting they are treated as an emergency. They are admitted and will have an NG tube placed for decompression and will be NPO and put on IV fluids and pain medicine. Sometimes surgery is required. Luckily for them there is a resolution. An end in sight.
Dilated loops of bowel with air fluid levels is the radiographic picture of a bowel obstruction. That is what a bowel obstruction looks like on imaging tests like CT scans and X-rays, MREs and barium follow-throughs. In patients with severe CIPO we live that every day of our lives but there is no fix. No surgery or solution to make it go away like for patients with actual mechanical obstructions or temporary ileus.
Every
day.
Also Check: When Does Ulcerative Colitis Start
Keep Up With Your Checkups
If you have either condition, you’ll need to keep up with your checkups, even if your symptoms start to ease up.
You may also need to get colonoscopies more often and start them at a younger age. A colonoscopy can check for cancer or polyps that need to come out. Experts recommend that you start these tests within 8 to 10 years of developing UC or Crohnâs symptoms, and then typically every 1 to 3 years after that. Your doctor will tell you a schedule that is best for you.
Show Sources
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Don’t Miss: How To Treat Skin Ulcer On Leg
Site Of Inflammation Differs Between Crohns Disease And Ulcerative Colitis
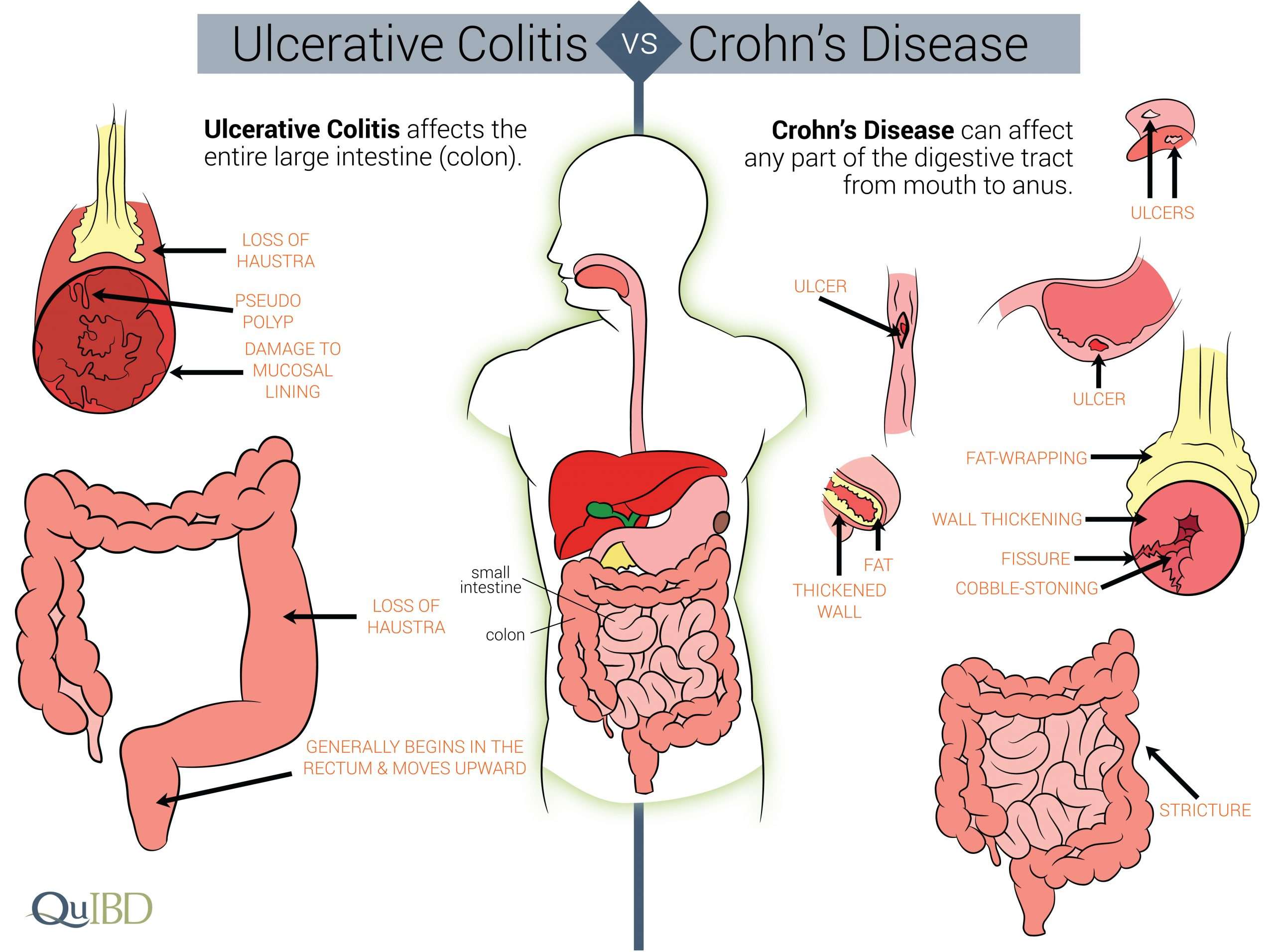
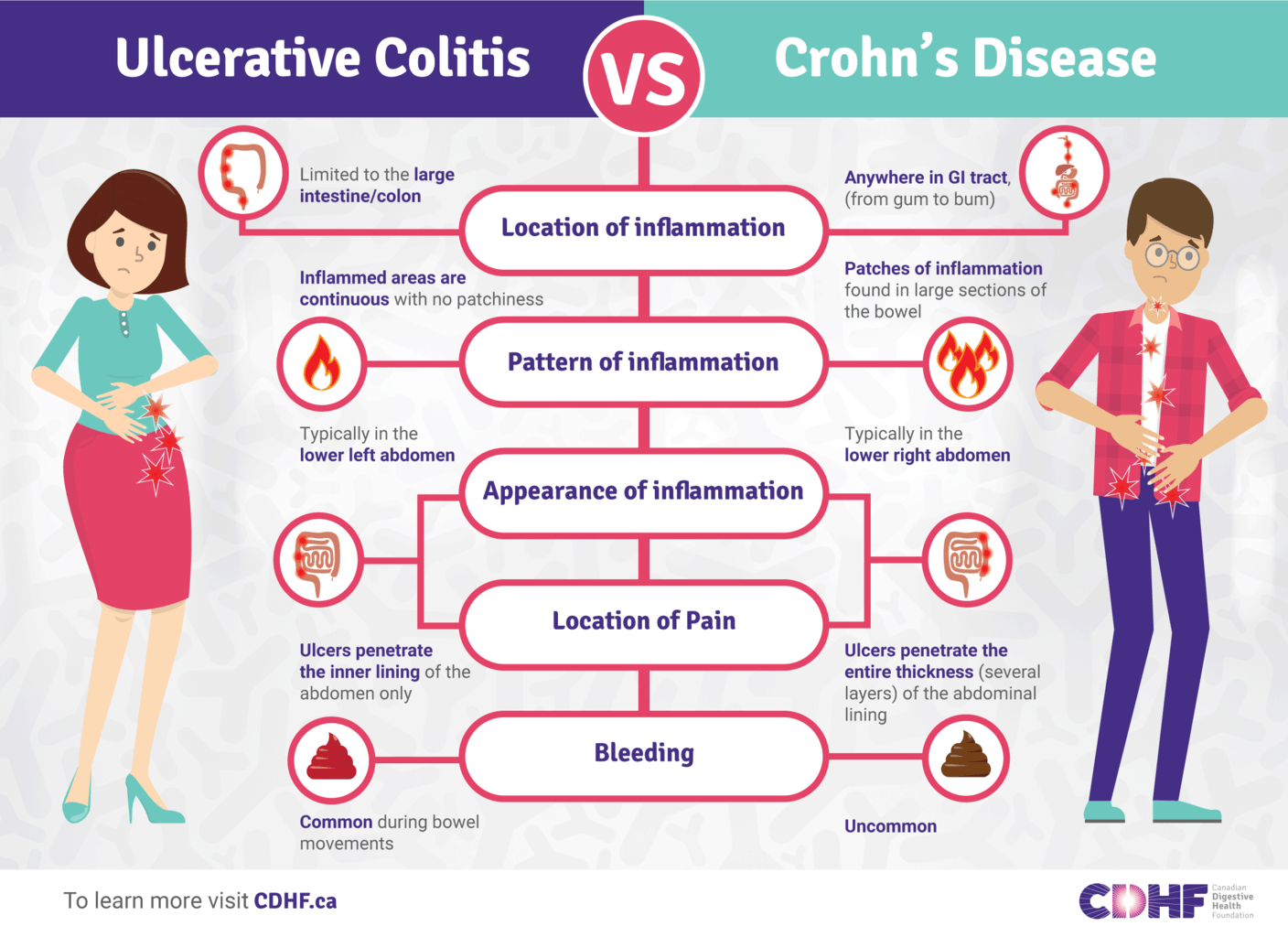
Crohns disease can affect any part of the gastrointestinal tract, including the mouth, esophagus, stomach, small and large intestines, rectum and anus. Ulcerative colitis is located in the colon, usually starting from the rectum. In Crohns disease, inflammation occurs in all layers of the intestinal wall and patches of this inflammation can be scattered throughout the GI tract. In contrast, in ulcerative colitis, inflammation occurs in the innermost lining of the intestinal wall and is a continuous stretch within the colon.
Colitis Update: Collagenous Colitis Pancolitis Crohns Disease Vs Ulcerative Colitis Infectious Colitis
Written byBel Marra HealthPublished onFebruary 17, 2018
Colitis refers to the inflammation of the colon, more commonly known as the large intestine. The inflammation could be the result of an allergic reaction, infection, an inflammatory bowel disease, or due to a reduction in blood supplya condition called ischemic colitis. Infectious colitis is usually caused by a virus, parasite, or bacteria and colitis that results from inflammatory bowel disease, including collagenous colitis, pancolitis and Crohns disease.
Colitis is a fairly common condition. One in 1,000 Americans suffers from it. The age of most patients who report colitis ranges from 15 to 35. Among the various forms of colitis, ulcerative colitis is the most common.In order to build awareness, we featured several articles including one on Crohns disease vs. ulcerative colitis, so our readers can understand how the two are different.
You May Like: How To Get Rid Of Tongue Ulcers
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Difficulties In Diagnosis Of Uc
As UC-associated dysplasia may occur in endoscopically normal mucosa, extensive biopsy sampling is necessary to confidently exclude the possibility of dysplasia. In order to exclude dysplasia with 90% confidence, a minimum of 33 well-oriented jumbo forceps biopsies are required 56 such biopsies are required to achieve a 95% level of confidence . This is the rationale for surveillance programs including periodic colonoscopic examination with protocol biopsies to detect dysplasia, which has now become the standard of care for surveillance in IBD patients .
In addition to sampling error, histological evaluation of dysplasia suffers from problems of diagnostic reproducibility. Few studies have evaluated inter-observer agreement in the diagnosis of UC-associated dysplasia , none of which assessed inter-observer agreement in the context of clinical outcome, the ultimate standard of diagnosis.
You May Like: How Do They Treat Stomach Ulcers
Also Check: Foam Dressing For Pressure Ulcer
How Are Ulcerative Colitis And Crohn’s Disease Similar
- Both diseases often develop in teenagers and young adults although the disease can occur at any age
- Ulcerative colitis and Crohn’s disease affect men and women equally
- The symptoms of ulcerative colitis and Crohn’s disease are very similar
-
The causes of both UC and Crohn’s disease are not known and both diseases have similar types of contributing factors such as environmental, genetic and an inappropriate response by the body’s immune system
Crohns Disease And Ulcerative Colitis Overview
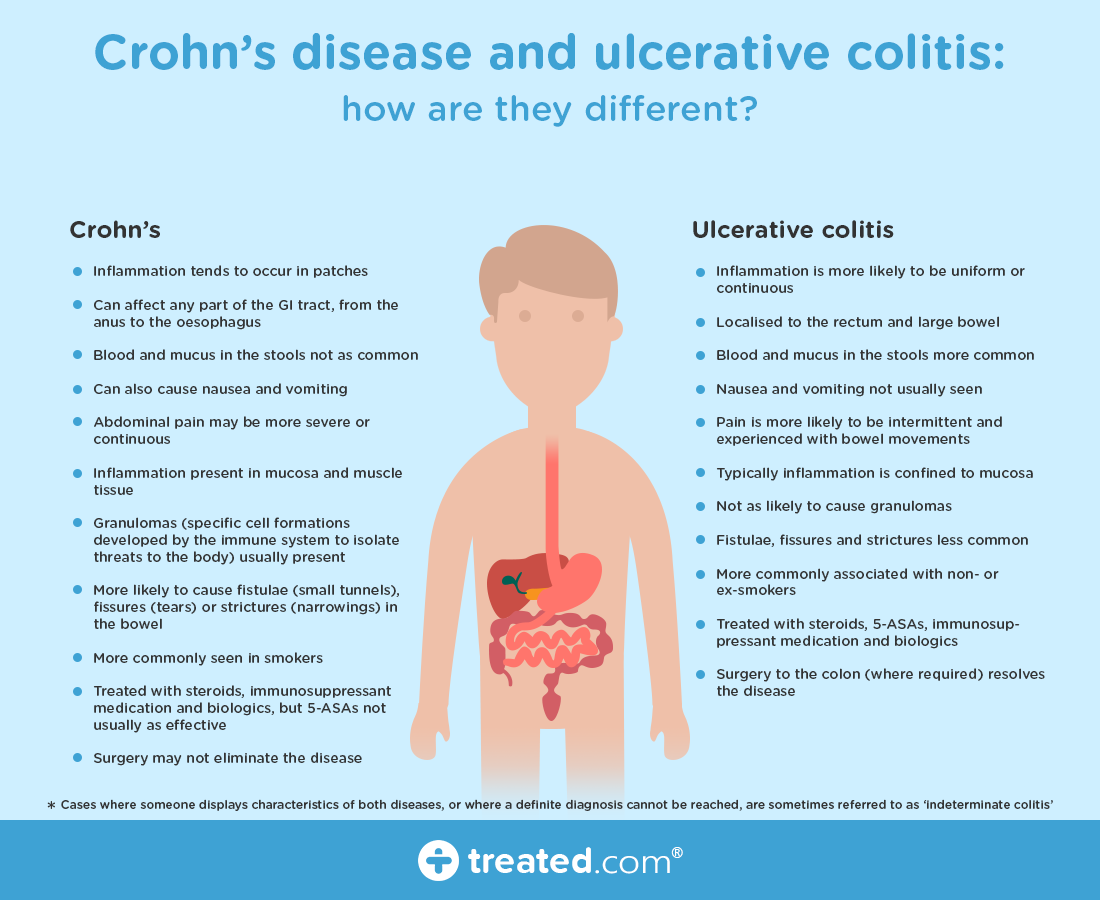
Crohns disease and ulcerative colitis are the two most common forms of inflammatory bowel disease . Crohns disease and ulcerative colitis can be treated, but there is no cure. UC and Crohns are separate diseases, but they both involve chronic inflammation of the digestive tract. People with IBD may have long periods of good health known as remission and periods of active symptoms known as relapses or flares. Symptoms vary among people with Crohns disease and ulcerative colitis, but most experience abdominal pain and cramping, diarrhea, nausea, vomiting, and fatigue.
Crohns disease and ulcerative colitis are not fatal, and on average, people with IBD have similar lifespans as people without either condition.
Both Crohns disease and ulcerative colitis are immune-mediated diseases, meaning the bodys immune response does not work as it should. In IBD, the immune system has an abnormal response, causing chronic inflammation and damage in the gastrointestinal tract. Read more about the causesof IBD.
You May Like: How Do You Heal Leg Ulcers
You May Like: What Is A Duodenal Ulcer And How Is It Caused
What Is Irritable Bowel Syndrome And Ulcerative Colitis
Irritable bowel syndrome and ulcerative colitis which is an inflammatory bowel disease are two medical conditions associated with the gastrointestinal system. The main difference between irritable bowel syndrome and inflammatory bowel disease is that the former is a non-inflammatory type of disease and the latter is a chronic inflammatory condition.
The major cause of IBS is disturbance in how the central nervous system and the gut interact and is aggravated by the emotional stress. Ulcerative colitis which is an IBD is caused by an abnormal response from the defense system of our body , mistaking healthy cells and bacteria in the gut for dangerous foreign agents.
More Information About Ulcerative Colitis
The following are some English-language resources that may be useful. Please note that THE MANUAL is not responsible for the content of these resources.
-
Crohns and Colitis Foundation of America: General information on Crohn disease and ulcerative colitis, including access to support services
-
United Ostomy Associations of America : Information and support resources for people who live with an ostomy
Read Also: What Foods Are Good For Ulcers And Gastritis
What Is The Process For Diagnosing Irritable Bowel Syndrome
When diagnosing your condition, the doctor will work to rule out other illnesses first. A physical exam and health history will be conducted, and you may be tested for Celiac disease or gluten intolerance if one of your recurrent symptoms is diarrhea. If no other illness is detected, the doctor will consider the longevity and degree of your abdominal pain and will examine your stool and defecation habits. These measures, known as the Rome and Manning criteria respectively, will help to accurately diagnose your IBS condition.
Can Ibs Turn Into Crohns Disease
There is no medical evidence that irritable bowel syndrome progresses to any other sickness or disease like Crohns disease or even results in any aggravating medical conditions outside of the regular symptoms. Irritable Bowel Syndrome is a syndrome and a functional disorder that changes the way the bowel functions. It is not a progressive disease.
Recommended Reading: Ulcerative Colitis Diet During Flare
How Can I Tell If I Have Ulcerative Colitis Or Crohns Disease
Its important that you, your healthcare provider, and a GI specialist work together closely to figure out whats causing your symptoms. This is especially important since the symptoms of Crohns disease and ulcerative colitis can be similar. Your providers may check blood work and a stool sample. To get an accurate diagnosis, your GI specialist may do a colonoscopy, where a camera is pushed into the colon. Your provider will look at the inside of the colon and take tissue samples, which are important for making the right diagnosis. Your providers might get a CT scan or an MRI of your abdomen to check for complications related to your condition.
Treatment Options For Ulcerative Colitis
Ulcerative colitis involves more than just medications and symptoms. It is a life changing condition that you are learning to manage, and it represents only part of your story. As you continue your journey with ulcerative colitis while in college, there may be many questions that you will have to navigate in order to help make your experience rewarding. This Campus Connection website will cover some helpful tips and information that you should know before, and during college, and offers a way for you to potentially connect with others like you.
Read our Living with Ulcerative Colitis brochure to learn more about the disease, treatment and daily living.
- Campus Connection
Read Also: Over The Counter Meds For Ulcers
Protagonist Therapeutics Announces Topline Data From Phase 2 Ideal Study Of Pn
PN-943 achieved 27.5% clinical remission with a delta of 13% versus placebo, with strong concordance across all key proxies including histological and endoscopic endpoints for efficacy, in the twice daily 150 mg dose arm
Achieved clinical proof-of-concept and validation for oral, gut-restricted approach for ulcerative colitis via blockade of the alpha-4-beta-7-integrin pathway
Plans underway for a registrational Phase 3 study anchored around twice daily 150 mg dose of PN-943, pending regulatory guidance
Protagonist to host a conference call today at 6:00 p.m. ET
NEWARK, Calif., April 25, 2022 /PRNewswire/ — Protagonist Therapeutics today announced topline results from the Phase 2 IDEAL study evaluating PN-943 in patients with moderate-to-severe ulcerative colitis .
“The oral, gut-restricted agent PN-943 appears to exert similar effects at the twice daily 150 mg dose in comparison to the approved injectable alpha-4-beta-7-integrin antibody drug and its mechanism of action,” said Bruce Sands, M.D., M.S., the Dr. Burrill B. Crohn Professor of Medicine at the Icahn School of Medicine at Mount Sinai, principal investigator for the IDEAL study and consultant to Protagonist. “There is a clear unmet need and strong clinical benefit for patients with an oral agent working through such a proven IBD specific mechanism, and the IDEAL study results provide good rationale for moving PN-943 forward in a Phase 3 registrational study.”
Summary of Key Results
About Protagonist
Contacts
Infectious Colitis: Causes Symptoms And Treatment Tips
The term infectious colitis sounds awful, and it can be. Infectious colitis is inflammation of the main part of the large intestine and can lead to sudden lower abdominal pain. In some cases, the pain can be severe.While inflammation is a common medical term and may not seem all that serious, the reality is that when left untreated, it can lead to complications and has the potential to be deadly.
Read Also: What To Eat With An Ulcerative Colitis Flare Up
Read Also: Is Nexium Good For Ulcers
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Read Also: How To Reduce Bloating With Ulcerative Colitis