Lcerative Colitis Diet Plan
Following an Ulcerative Colitis diet plan is a bit more complicated than something like an IBS plan. The ideal diet for UC patients will vary depending on their symptom severity. For example, during flare-ups, youll want to be gentle on your intestines, eating low-fiber foods. However, when you arent having flare-ups, its healthier and more protective to feed your gut bacteria the fiber it needs.
There is a delicate balance that UC patients need to maintain, and its often a fine line with much back-and-forth from week to week. Your best option is to keep a food journal and log all of your symptoms each day. This way, you can find what works best for you. If you have any questions about how to create a food journal or about other treatments to minimize your UC symptoms, get in touch with the colorectal experts at the Colorectal Clinic of Tampa Bay.
Best Foods To Eat During An Ulcerative Colitis Flare
HomeUlcerative Colitis7 Best foods to eat during an ulcerative colitis flare-ups
Ulcerative colitis is a long-lasting condition that causes inflammation and ulcers in your digestive tract. It usually affects the innermost lining of your large intestine and the rectum. Symptoms of ulcerative colitis develop over time, rather than all of sudden.
The food you eat has a great impact on the severity of your Ulcerative colitis symptoms. If you have ulcerative colitis, you may already identify various foods as triggers. But figuring out what foods to eat is also equally important as the right foods will provide you key nutrients without irritating your digestive tract.
I Have Heard That Fiber Is Good For Ulcerative Colitis What Does Onpoint Say
-
We encourage you to eat a medium/high fiber diet when you are not experiencing a flare up. A high fiber diet is almost always encouraged in all adults, part of maintaining a healthy gut as well
-
If you decide to increase your fiber intake, increase it gradually, even if you are not having GI or IBD issues presently
-
You may find a “Low Residue” approach helpful. We have seen it work well for some people
-
Increase or be aware of hydration and fluid intake. Try to drink at least 64 oz of water per day
-
Some studies show that a higher fiber diet can improve IBD conditions
Recommended Reading: What Is Best Medicine For Ulcer
What To Eat On An Ulcerative Colitis Diet During Remission:
What you should eat on an Ulcerative Colitis diet plan is very individual but lets get acquainted with what it takes to be on an Ulcerative Colitis diet plan when your disease is not active:
What You Can Eat on an Ulcerative Colitis Diet.
-
Eat a variety of vegetables and fruits.
-
Select the refined grains. These have been milled to remove the bran and germ, may increase symptoms.
-
Include protein-rich foods.
-
Get enough calcium.
-
Drink plenty of fluids.
Your Ulcerative Colitis diet plan can even be more liberal when your symptoms subside but remember to:
-
Go Slowly. Gradually add more foods back into your diet. Shift to whole grains and those colorful veggies and fruits. Start with small amounts of these foods. If your symptoms act up, add that item to your potential list of trigger foods. You can try eating that food at a later time.
-
Eat 5 or 6 small meals per day. Go easy on your GI tract. Large meals can flare your symptoms and make you feel bloated.
-
Stay well hydrated. Sip on water throughout the day. As you add back in fiber, getting enough to drink is important. Fiber without adequate fluid intake can lead to constipation.
-
Avoid your trigger foods. Focus on the foods you can eat and enjoy. Create a list of substitutions for your trigger foods.
Dietary Advice For Ulcerative Colitis
Please note, this page is printable by selecting the normal print options on your computer.
What is Ulcerative Colitis?
Ulcerative Colitis is a form of Inflammatory Bowel Disease . IBD is a term used to cover a number of inflammatory conditions of the gastrointestinal tract. UC causes inflammation in the large bowel and can affect the rectum, part of, or the entire colon. If you have UC this diet sheet may help you.
Can diet help?
Diet is not a cause of UC however diet can help to relieve symptoms such as diarrhoea during a flare up and maintain good health including healthy bones. You may find as time goes by you begin to notice that certain foods aggravate your symptoms of UC and so they are best avoided. However, do not remove whole food groups as this could mean you lose some vital nutrients. The main food groups are demonstrated below in the Eatwell Guide.
What foods are beneficial for UC during a flare up?
Soluble FibreDietary fibre can be categorised into two forms, soluble and insoluble. Soluble fibre is partially digested in the large intestine to form a glue like substance, which helps to produce soft/formed stools, without causing inflammation. Examples of foods rich in soluble fibre are:
- Oats e.g. Porridge oats/Ready Brek ®, oatcakes
- The body of fruits and vegetables e.g. peeled apples and pears, tinned fruit, peeled root vegetables such as carrots, parsnips, turnip
What foods may worsen UC during a flare up?
Dairy foods
Spicy foods and fatty foods
Also Check: Herbal Tea For Ulcerative Colitis
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
Dietary Habits Of Uc Cases And Controls
No significant difference was observed between cases and controls in terms of dietary habits including regular meal pattern, chewing efficiency, fluid consumption during meals, fried foods intake, and fatty meals intake. This was also the case when we compared the distribution of subjects in terms of above-mentioned variables across quartiles of IPD score .
Table 2. Distribution of patients with ulcerative colitis and controls in terms of dietary habits across quartiles of inflammatory potential of the diet score.
Don’t Miss: Ulcerative Colitis Lower Back Pain
What Should I Eat If I Have Ulcerative Colitis
If you have ulcerative colitis, you should eat a healthy, well-balanced diet. Talk with your doctor about a healthy eating plan.
Ulcerative colitis symptoms may cause some people to lose their appetite and eat less, and they may not get enough nutrients. In children, a lack of nutrients may play a role in problems with growth and development.
Researchers have not found that specific foods cause ulcerative colitis symptoms, although healthier diets appear to be associated with less risk of developing IBD. Researchers have not found that specific foods worsen ulcerative colitis. Talk with your doctor about any foods that seem to be related to your symptoms. Your doctor may suggest keeping a food diary to help identify foods that seem to make your symptoms worse.
Depending on your symptoms and the medicines you take, your doctor may recommend changes to your diet. Your doctor may also recommend dietary supplements.
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Don’t Miss: Foods Bad For Ulcerative Colitis
List Of Foods To Eat To Keep Colitis From Flaring Up
Colitis is an inflammatory bowel disease. There are several types of colitis, depending on the location of the inflammation. Symptoms vary but commonly include abdominal cramps, bloating, constipation and diarrhea. There’s really no nutritional therapy for colitis, nor is there a cure. But learning to strike a balance between getting the nutrients you need and avoiding the foods that seem to trigger your symptoms can help you manage the condition.
Video of the Day
Can Ulcerative Colitis Be Healed
However, there is no cure for ulcerative colitis, and treatments can help you feel better, decrease your inflammation, and return you to your daily routine. Furthermore, the treatment is tailored to each persons unique needs, so it also varies depending on how severe the illness and how severe the individual is. Medications are typically used by healthcare providers to treat this disease.
Don’t Miss: What Are The Signs Of A Bleeding Stomach Ulcer
Are There Common Foods To Avoid If You Have Ulcerative Colitis
Okay, so weve established that there are no surefire foods to avoid that will reduce or eliminate ulcerative colitis symptoms. But there are some foods that you could try to avoid during a flare-up until your bowels calm down. Those include:
Many people hail fiber as a magical nutrient that can lower your risk of developing heart disease, type 2 diabetes, and potentially offer some protection against Crohns disease flaresanother type of IBD. And, well, loading up on fiber can aid in all of those things.
However, some people with ulcerative colitis may want to avoid a high-fiber diet, depending on their symptoms, according to the Crohns & Colitis Foundation. If diarrhea is a hallmark of your ulcerative colitis, you may want to eat less insoluble fiber because it moves food through the intestine quicklywhich only makes the problem worse. To reduce your insoluble fiber intake, you may want to lay off beans and other legumes like chickpeas or lentils, cruciferous vegetables like cauliflower or kale, nuts, and whole wheat flour in your diet to see if your symptoms improve3.
Initially, the low-FODMAP diet is very restrictive: The idea is to cut out all FODMAPs before slowly reintroducing some to determine which you can tolerate. So, its important to work with your health team when making any dietary change to avoid nutritional deficiencies.
Food Preparation And Meal Planning

While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Also Check: Signs Of Having A Stomach Ulcer
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
What Causes Ulcerative Colitis
The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitiscan run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress, and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.
Also Check: What Can You Eat If You Have Ulcerative Colitis
What Can Worsen Ulcerative Colitis
Foods To Avoid During Flares
Diet doesnt cause flares, but your food choices can make symptoms worse if your IBD becomes active.
How foods affect people who are flaring varies from person to person. But here are some of the foods that may worsen symptoms of a flare and cause complications:
- Fatty foods
- Beverages containing alcohol or caffeine.
- Sugar alcohols used to sweeten in sugar-free foods
- Raw fruits and vegetables
- Whole grain and high-fiber breads and cereals
- Dried fruit
- Fruits with seeds and skins
You May Like: Pressure Ulcer Care At Home
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
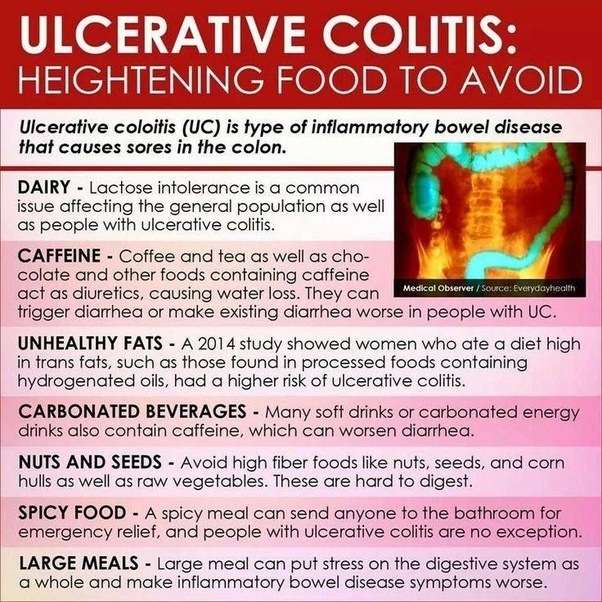
The Worst Foods For Those With Ulcerative Colitis
Ulcerative colitis is an inflammatory chronic disease of the colon and rectum where ulcers develop inside the lining of the large intestine. It is an inflammatory bowel disease along with Crohns Disease which causes a multitude of painful and unpleasant symptoms. Since dietary habits can contribute to ulcerative colitis symptoms, lets look at the worst foods for those with ulcerative colitis.
Recommended Reading: Offloading The Diabetic Foot For Ulcer Prevention And Healing
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!