How Should I Take Imodium A
Use Imodium A-D exactly as directed on the label, or as prescribed by your doctor.
Imodium A-D is safe when used as directed. TAKING TOO MUCH LOPERAMIDE CAN CAUSE SERIOUS HEART PROBLEMS OR DEATH.
Carefully follow all dosing directions on the medicine label. A safe dose of loperamide is different for an adult than for a child. This medicine doses in children are based on the child’s age.
Take Imodium A-D with a full glass of water. Diarrhea can cause your body to lose fluids and electrolytes. Drink plenty of liquids to keep from getting dehydrated.
The chewable tablet must be chewed before swallowing. Take the chewable tablet on an empty stomach
Shake the oral suspension before you measure a dose. Use the dosing syringe provided, or use a medicine dose-measuring device .
Not all liquid forms of this medicine are the same strengths. Carefully follow all dosing instructions for the medicine you are using.
Store at room temperature away from moisture and heat. Do not allow the liquid medicine to freeze.
Stop taking Imodium A-D and call your doctor if you still have diarrhea after 2 days of treatment, or if you also have stomach bloating.
What Problems Are Associated With Chronic Diarrhea
Healthcare providers will assess a patients symptoms to determine whether or not they are exhibiting acute or chronic diarrhea. Acute diarrhea is defined as watery stool lasting 2 weeks, whereas chronic diarrhea is watery stool lasting longer than 4 weeks. Acute diarrhea is often caused by a virus, but sometimes it is caused by bacteria, in which case it will be treated with antibiotics. Chronic diarrhea, on the other hand, may be due to CD or UC.1,2
Chronic diarrhea often directly impacts a patients nutritional status. Patients experiencing chronic diarrhea are at risk of becoming malnourished, because not enough nutrients can be absorbed by the digestive tract. While it is possible that certain food types can agitate the digestive tract causing chronic diarrhea, it is important for patients to contact their healthcare provider before self-imposing any dietary restrictions.
Patients experiencing chronic diarrhea due to IBD should work with their healthcare providers to develop a treatment plan. One form of management is the use of medications called anti-diarrheals.
How Do You Stop Diarrhea With Ulcerative Colitis
4.4/5diarrhea
You may need additional medications to manage specific symptoms of ulcerative colitis. For severe diarrhea, loperamide may be effective. However, use anti-diarrheal medications with great caution and only after talking with your doctor.
Also Know, how long does diarrhea last with colitis? The diarrhea can vary from loose stools to dysentery with grossly bloody and purulent feces. Symptoms arise 8 to 48 hours after ingestion of contaminated food. The illness lasts for 3 to 5 days in patients manifesting with gastroenteritis and 2 to 3 weeks in patients who develop enterocolitis.
Also asked, why do I have diarrhea with ulcerative colitis?
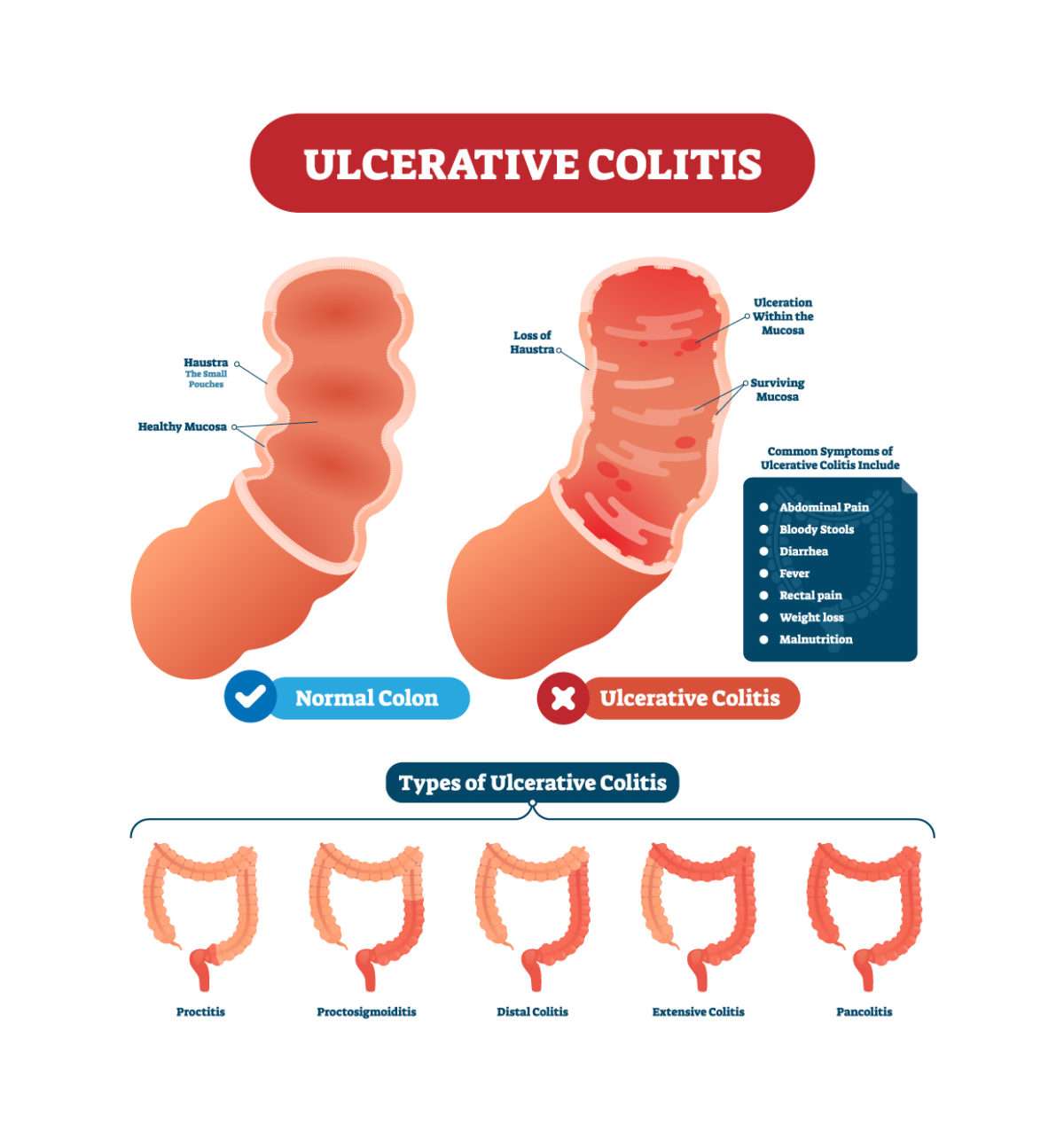
Ulcerative colitis is a chronic inflammatory disease that affects the lining of the large intestine and rectum. People with this condition have tiny ulcers and small abscesses in their colon and rectum that flare up periodically and cause bloody stools and diarrhea.
Can you take Imodium with colitis?
You should not use loperamide if you have ulcerative colitis, bloody or tarry stools, diarrhea with a high fever, or diarrhea caused by antibiotic medication. Loperamide is safe when used as directed. TAKING TOO MUCH LOPERAMIDE CAN CAUSE SERIOUS HEART PROBLEMS OR DEATH.
Also Check: Venous Leg Ulcer Dressing Treatment
Which Drugs Or Supplements Interact With Loperamide
Cholestyramine binds to loperamide in the intestines and prevents its absorption, thereby reducing the effect of loperamide. Therefore, there should be at least a two-hour interval between doses of loperamide and cholestyramine.
Theoretically, some drugs that are used to increase propulsion of intestinal contents could counteract loperamide. Such drugs include bethanechol , cisapride , metoclopramide , and erythromycin.
Prednisone Prednisolone And Methylprednisolone

Prednisone is taken by mouth and is available as:
- an immediate-release tablet
- a delayed-release tablet
- a liquid solution
Its available as a generic drug and as the brand-name drugs Prednisone Intensol and Rayos .
The forms of prednisolone that are FDA approved for UC are:
- immediate-release tablet
- liquid solution
- syrup
You can take any of these forms by mouth. Prednisolone is available as a generic drug and as the brand-name drugs Millipred and Prelone .
Methylprednisolone comes in two forms:
- oral tablet
- injectable medication
Its available as a generic drug and as the brand-name drugs Medrol and Depo-Medrol .
Side effects, complications, and interactions
When given in high doses, the side effects of these drugs are practically indistinguishable. The more common side effects can include:
- increased blood sugar levels
Immunomodulators are drugs that decrease the bodys response to its own immune system. The result is lowered inflammation throughout your body.
Immunomodulators may reduce the number of UC flare-ups you have and help you stay symptom-free longer.
Theyre generally prescribed to people whose symptoms havent been managed with 5-ASA drugs and corticosteroids. However, these drugs may take several months to start working.
The Food and Drug Administration hasnt approved immunomodulators for the treatment of UC.
However, theyre well supported in medical literature as useful options, and your doctor may still prescribe them. This is known as off-label drug use.
You May Like: Is Alcohol Bad For Ulcerative Colitis
Diagnosis Of Ulcerative Colitis
X-rays of the abdomen taken after barium is given by enema do not require any special preparation . These x-rays usually can show a blockage or paralysis… read more ) may indicate the severity and extent of the disease but are not done when the disease is active, such as during a flare-up, because of the risk of causing a perforation. Other x-rays of the abdomen may also be taken.
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Don’t Miss: Doctors Specializing In Ulcerative Colitis
Cured My Uc Through Imodium Ad And Diet
Meet Ben:
I dont use Facebook or Twitter, my life was hell. I hope some people get relief trying what I am doing. I hope this helps.
Some more about Ben:
Raising a family, weight lifting, going to the beach. I live in Melbourne Beach Florida. I am a workaholic that is just now figuring out how to live. Recently I learned about laws of attraction and am applying it to all aspects of life.
Symptoms:
None, from what I have read even in remission your colon should be inflamed, mine is not.
What Causes Crohns Disease
Theres no known cause of Crohns disease. Certain factors may increase your risk of developing the condition, including:
- Autoimmune disease: Bacteria in the digestive tract may cause the bodys immune system to attack your healthy cells.
- Genes: Inflammatory bowel disease often runs in families. If you have a parent, sibling or other family member with Crohns, you may be at an increased risk of also having it. There are several specific mutations to your genes that can predispose people to developing Crohns disease.
- Smoking: Cigarette smoking could as much as double your risk of Crohns disease.
You May Like: Over The Counter For Ulcers
Drugs That Target Inflammation
Most people with UC take prescription drugs called aminosalicylates that tame inflammation in the gut. These include balsalazide , mesalamine , olsalazine , and sulfasalazine . Which one you take, and whether it is taken by mouth or as an enema or suppository, depend on the area of your colon that’s affected. As long as you avoid your triggers, these may be enough if your disease is mild to moderate.
You may need something else if your condition is more severe or if those standard treatments stop working. Your doctor may consider other medicines. Some people may also need surgery.
Tap Into ‘good’ Bacteria
Antibiotics can trigger flares. If your UC gets worse while you take them, tell your doctor. Some scientists think antibiotics cause issues because they kill “good” bacteria in your gut that aid digestion. Although research is limited, there is some evidence that probiotics, which contain these bacteria, along with other medications may be helpful, but this has not been proved.
12
Some flare symptoms are very serious. Get medical help right away if you have:
- A high fever
- Constant, heavy diarrhea
- New or more blood in your stool, or any blood clots
Also get help if you feel like you’re going to faint or you vomit over and over.
13
Recommended Reading: Foods To Avoid With Peptic Ulcer
Complications Of Ulcerative Colitis
Although people with ulcerative colitis commonly have minor liver dysfunction, only about 1 to 3% have symptoms of liver disease, which vary from mild to severe. Severe liver disease can include inflammation of the liver , inflammation of the bile ducts , which narrow and eventually close, and replacement of functional liver tissue with scar tissue . Inflammation of the bile ducts may appear many years before any intestinal symptoms of ulcerative colitis. The inflammation greatly increases the risk of cancer of the bile ducts and also seems to be associated with a sharp increase in the risk of colon cancer.
What Questions Should I Ask My Doctor
If you have Crohns disease, you may want to ask your healthcare provider:
- Why did I get Crohns disease?
- What form of Crohns disease do I have?
- Whats the best treatment for this disease type?
- How can I prevent flare-ups?
- If I have a genetic form, what steps can my family members take to lower their risk of Crohns disease?
- Should I make any dietary changes?
- What medications should I avoid?
- Should I take supplements?
- Should I get tested for anemia?
- Do I need to cut out alcohol?
- Should I look out for signs of complications?
A note from Cleveland Clinic
Crohns disease flare-ups are unpredictable and can disrupt your daily life. Talk to your healthcare provider about the steps you can take to keep the disease in check. With the right treatment and lifestyle changes, you can manage symptoms, avoid complications and live an active life.
You May Like: How You Know If You Have A Stomach Ulcer
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
Give Yourself Some Tlc
Stress doesn’t cause UC, but it makes symptoms and flares worse for some people. If it affects you, try meditation, breathing exercises, or a massage. You could also see a pro to try biofeedback, hypnotherapy, or a type of counseling called cognitive behavioral therapy, which helps you learn new ways to handle problems. Being active helps, too. Try yoga, tai chi, or other low-impact exercises like walking.
10
Recommended Reading: Can Stress Cause Flare Up Ulcerative Colitis
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
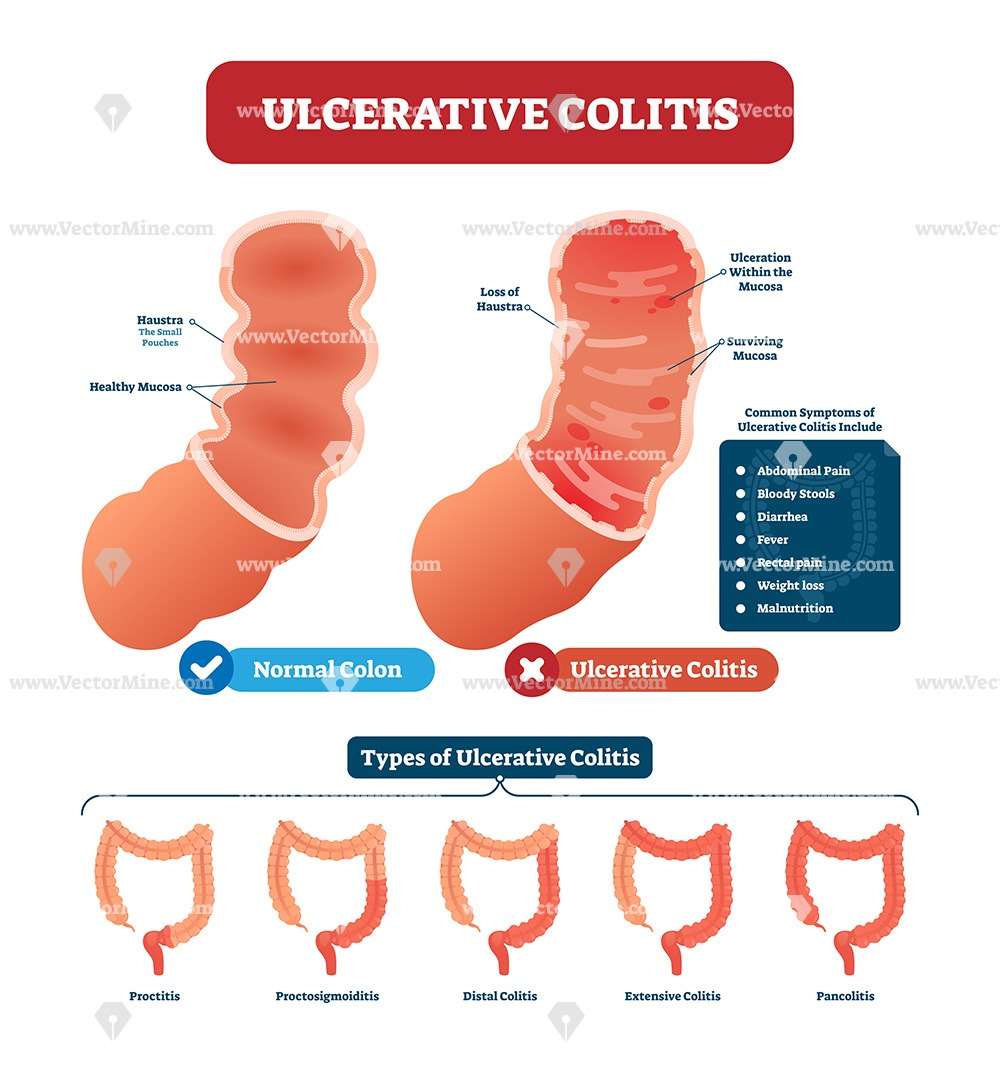
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Also Check: Best Supplement For Gastric Ulcers In Horses
Before Taking This Medicine
You should not use Imodium A-D if you are allergic to loperamide, or if you have:
-
stomach pain without diarrhea
Ask your doctor before using Imodium A-D to treat diarrhea caused by Clostridium difficile.
Ask a doctor before using this medicine if you are pregnant or breastfeeding.
You should not breast-feed while you are using loperamide.
Youre Drinking Caffeine Or Alcohol
Coffee, tea, and sodas can make UC flare-ups worse, says Yun, because caffeine is a stimulant that can get your intestines going not what you need when you have diarrhea. The same goes for beer, wine, and liquor. People with active UC symptoms should consider skipping caffeinated and alcoholic drinks.
Read Also: Ulcerative Colitis Is It Deadly
What Is An Anti
Chronic diarrhea is a common symptom reported by patients with IBD.3 This can be extremely uncomfortable and negatively impact a patients health and quality of life. Anti-diarrheal medications can be helpful in long-term management of the disease. However, it is important to note that anti-diarrheals will not treat the underlying cause of the diarrhea, which is inflammation in the digestive tract due to IBD. This inflammation can only be treated with medications that specifically target the disease itself, such as aminosalicylates,immunomodulators, corticosteroids, antibiotics, and/or biologic therapies. Over-the-counter symptom management medications such as anti-diarrheals should never be used to replace those IBD medications, only to supplement them. Although anti-diarrheals will not treat the underlying cause of the diarrhea, they may help to mask the symptom and improve a persons quality of life on a day-to-day basis.
An anti-diarrheal is a medication that provides symptomatic relief of diarrhea. The most common anti-diarrheal is loperamide, also known as Imodium. Loperamide is an over-the-counter medication that can be useful in decreasing bowel movement frequency by effectively slowing down the digestive process. This allows for the better absorption of nutrients through the digestive tract. Loperamide also increases the anal sphincter tone at rest. Some other forms of anti-diarrheals, such as diphenoxylate/atropine , are only available with a prescription.1,3
Talk With Your Doctor
Many drugs can help reduce your UC symptoms.
Your doctor will suggest medications based on factors such as your overall health and the severity of your condition. You may need to try a few medications before you find a treatment plan that works for you.
If taking one medication doesnt reduce your symptoms enough, your doctor may add a second medication that makes the first one more effective.
It may take some time, but your doctor will work with you to find the right medications to help relieve your UC symptoms.
You May Like: Ulcerative Colitis Surgery Pros And Cons
Youre Not Avoiding Trigger Foods
Theres no food or food group that causes or cures ulcerative colitis, Yun explains. But many people with UC say that certain foods either bring on symptoms or make them worse.
During a flare-up, your doctor may recommend adjustments to your diet. This can mean avoiding foods that trigger symptoms such as bloating, diarrhea, or cramping. For example, dairy products can be particularly irritating for people who have both UC and lactose intolerance.
Aside from dairy, common trigger foods include beans, whole grains, nuts, seeds, some raw fruits and vegetables, high-fat foods, sugary foods, and sugar alcohols. If youre trying an elimination diet to determine which of these foods you need to avoid, keep a food diary, and always work with a healthcare practitioner to ensure youre getting all the nutrients you need.