Positioning And Support Surfaces
Preamble: Pressure and compression to soft tissue play a role in the etiology of pressure ulcers. Patient positioning and methods to reduce pressure-related tissue damage are recognized as important treatment components. While there are limited definitive studies, the best current evidence and expert opinion suggest the following guidelines.
Guideline #1.1: Establish a repositioning schedule and avoid positioning patients on a pressure ulcer.
Principle: Pressure ulcers are thought to result from compression of soft tissues against a bony prominence. It is reasonable to assume that pressure on an ulcer can result in delayed healing. Patients should be repositioned to relieve pressure over bony prominences. The exact turning interval is not known and is derived empirically. Reductions in pressure incidence have been achieved, but positioning is not universally effective.
Evidence:
- 1
Clark M. Repositioning to prevent pressure soreswhat is the evidence? Nurs Standard 1998 13: 5664.
- 2
Defloor T. Less frequent turning intervals and yet less pressure ulcers. Tijdschrift voor Gerontologie en Geriatrie 2001 32: 1747.
- 3
Knox DM, Anderson TM, Anderson PS. Effects of different turn intervals on skin of healthy older adults. Adv Wound Care 1994 7: 4856.
- 4
Thomas DR. Are all pressure ulcers avoidable? J Am Med Directors Assoc 2001 2: 297301.
Evidence:
- 1
Thomas DR. Management of pressure ulcers. J Am Med Directors Assoc 2006 7: 4659.
Evidence:
Evidence:
Evidence:
Evidence:
Agreements And Disagreements With Other Studies Or Reviews
We have been unable to identify any network metaanalyses directed at healing pressure ulcers and incorporating both dressings and topical agents. The AHRQ guideline reviewed the evidence for dressings in a series of pairwise comparisons and stated that overall, they did not find substantial evidence to support certain local wound applications over others . The most recent NICE guideline on the prevention and management of pressure ulcers considered all RCT evidence on dressings and separately all RCT evidence on topical agents. NICE recommendations are to not use saline gauze dressings and for the health professional and adult to discuss the type of dressing to use, taking into account pain and tolerance, position of the ulcer, amount of exudate and frequency of dressing change. These recommendations rely heavily on consensus decisions, weakly supported by the evidence, and as such, agree with the findings of this review.
Evidence And Scientific Basis For Guidelines
The panel identified six categories of pressure ulcer treatment: positioning and support surfaces, nutrition, infection, wound bed preparation, dressings, and surgery and adjuvant therapies. Specific guidelines and the underlying principle were developed in each category. Evidence references for each standard are listed and coded. The code abbreviations for the evidence citations were as follows:
| STAT |
-
Lyder CH. Pressure ulcer prevention and management. JAMA 2003 289: 2236.
- 2
Barrois B, Allaert FA, Colin D. A survey of pressure sore prevalence in hospitals in the greater Paris region. J Wound Care 1995 4: 2346.
- 3
Allman RM, Paprade CA, Noel LB, et al. Pressure sores among hospitalized patients. Ann Intern Med 1986 105: 33742.
- 4
Walter JS, Sacks J, Othman R, et al. A database of self-reported secondary medical problems among VA spinal cord injury patients: its role in clinical care and management. J Rehab Res Dev 2002 39: 5361.
- 5
Shiffman RN, Dixon J, Brandt C, Essahihi A, Hsiao A, Michel G, OâConnell R. The GuideLine implementability appraisal : Development and validation of an instrument to identify obstacles to guideline implementation. BMC Med Inform Dec Making 2005 5: 123.
Don’t Miss: Align Probiotic For Ulcerative Colitis
What Is A Stage 4 Bedsore
Stage 4 bedsores are the most severe form of , also called pressure sores, pressure ulcers, or decubitus ulcers. A stage 4 bedsore is characterized by a deep wound that reaches the muscles, ligaments, or even bone. They often cause residents to suffer extreme pain, infection, invasive surgeries, or even death.
A stage 4 bedsore may be an unfortunate sign of . Residents of nursing homes may develop these sores if the staff fails to treat earlier-stage sores.
Thankfully, financial compensation may be available if your loved one develops a stage 4 bedsore while living in a nursing home. Get a free case review to see if you can pursue compensation to help pay for medical treatment.
Victims of stage 4 bedsores can take legal action.
to learn if you can access financial aid and hold abusive nursing homes accountable.
Analysis Of Existing Evidence
The effect of pressure ulcers on patients, nurses, and hospitals is outlined in academic literature. Qaseem et al. find that the prevention of bedsores is much more beneficial than their treatment. First of all, pressure ulcers are dangerous to the health of patients as it is described above. Skin damage and the following infections increase morbidity and mortality, putting patients at increased risk of complications and prolonged length of stay at the hospital .
Second, clinicians also encounter challenges in dealing with bedsores as the latter require adequate assessment and difficult treatment. Prevention, on the other hand, can be performed in steps that have been tested and documented. Finally, the rate of ulcers affects hospitals and units as it is one of the factors of healthcare organizations ratings. The high incidence of bedsores implies the poor quality of service, low rating of the unit, and decreased financial support.
In order to adequately address the issue, it is necessary to understand how pressure ulcers can be measured. According to Fletcher and Hall , nurses may face many challenges due to hospitals having different records of patients with pressure ulcers. Some of the wounds may be called bedsores, while others may have names such as moisture-associated dermatitis or sacral and gluteal lesions .
Don’t Miss: Diet If You Have An Ulcer
Diagnosis Of Bedsores In The Third Stage
Symptoms or a deeper incision generating puffy skin might diagnose bedsores. Your doctor may examine the wounds surface for sensitivity and stages. Staging helps decide the best treatment. Stages 1 and 2 are painful.
Deepness in Wounds stage 3 Bedsores can be defined as a more profound tissue injury. Tunnel wounds penetrate the skin and the underlying tissue but are not confined to bone or muscle.
Review Question: What Are The Most Reliable Techniques/tools To Measure The Dimensions Of A Pressure Ulcer
One systematic review looked at the performance of instruments designed for measuring the dimensions of pressure ulcers. This systematic review was included in the current evidence review and it was subsequently updated to include 1 other study . Overall 13 studies were included in the evidence review.,,,,,,,,,,,, Evidence from these is summarised in the clinical GRADE evidence profile below. The quality of these studies is outlined in .
The OMeara review looked at studies of any design which reported an evaluation of a pressure ulcer measurement instrument as the main focus of the investigation. The authors did not include assessment checklists where the focus was the performance of the tool overall rather than the measurement of pressure ulcer dimensions.
Recommended Reading: Are Eggs Bad For Ulcerative Colitis
Read Also: How To Treat Gum Ulcers
Protect The Periwound Skin
Askina® Barrier Cream acts as a protectant and moisture barrier against maceration caused by incontinence or body fluids, to protect sensitive, fragile skin and severely dry skin, including periwound areas. It is indicated for use on intact skin.
Askina® Barrier Film Swab andAskina® Barrier Film Spray are sterile liquid dressings which form a transparent film when applied to the skin. The film possesses good oxygen and moisture permeability. Both dressings are indicated for use on intact or damaged skin.
Measuring Key Processes Of Care
5.2.1 Why measure key processes of care?
While measuring pressure ulcer rates is the ultimate test of how your facility or unit is performing, pressure ulcer rates are limited in that they do not tell you how to improve care. If your pressure ulcer rate is high, on what specific areas should you focus? To know where to focus improvement efforts, it is important to measure key processes of care. Many important processes of care could be measured in assessing pressure ulcer prevention. We recommend initially looking at no more than three:
- Performance of comprehensive skin assessment within 24 hours of admission.
- Performance of standardized risk assessment within 24 hours of admission.
- Performance of care planning that addresses each deficit on standardized risk assessment.
5.2.2 What data sources should be used in measuring key processes of care?
Much pressure ulcer preventive care may not be documented. Nonetheless, we recommend medical record reviews as the source of data on the performance of key processes of care. While rates may initially be low because of poor documentation, this finding will encourage improved documentation of the care actually being provided.
Tools
Use this tool developed by the Quality Improvement Organization program for abstracting medical record data .
5.2.3 How do we ensure performance of comprehensive skin assessment within 24 hours of admission?
Tools
A sample protocol for checking skin assessments is available in Tools and Resources .
Tools
You May Like: How To Measure Pressure Ulcers
Nursing Home Neglect And Stage 3 Bedsores
When a lack of care causes a resident to develop a stage 3 bedsore, nursing home neglect may have occurred.
Neglect is not the same thing as making a simple, harmless mistake its a life-threatening error or series of errors. Sadly, poorly trained or inattentive staff can provide consistently poor care to residents, which can lead to bedsores.
Nursing home neglect often goes hand-in-hand with another issue: understaffing in long-term care facilities. When there are less staff members available, residents may have to wait long hours before their health care needs are addressed.
In chronically understaffed nursing homes, care problems can go unresolved for months making it more likely for bedsores to develop.
Understaffing may lead to stage 3 bedsores, as caretakers are:
- Less likely to notice or treat bedsores in their early stages
- At a greater risk of forgetting to care for every resident
- More likely to leave a resident in bed or a wheelchair for too long
Has your loved one suffered from a stage 3 bedsore?Get a free case review to get justice.
Stage 3 Bedsore Diagnostic Issues
It may not always be possible to diagnose a stage 3 bedsore. Bedsores are considered unstageable if theres too much slough or eschar around them. Doctors will not be able to tell how deep the sore goes until these are removed.
Doctors may not even want to remove the eschar in some cases. For example, eschar that develops on bedsores near the heel signal that the sore is repairing itself.
Thankfully, doctors can often treat severe bedsores even if they cannot assign them a stage. The key is to seek medical attention as soon as possible.
You May Like: Managing Ulcerative Colitis Flare Ups
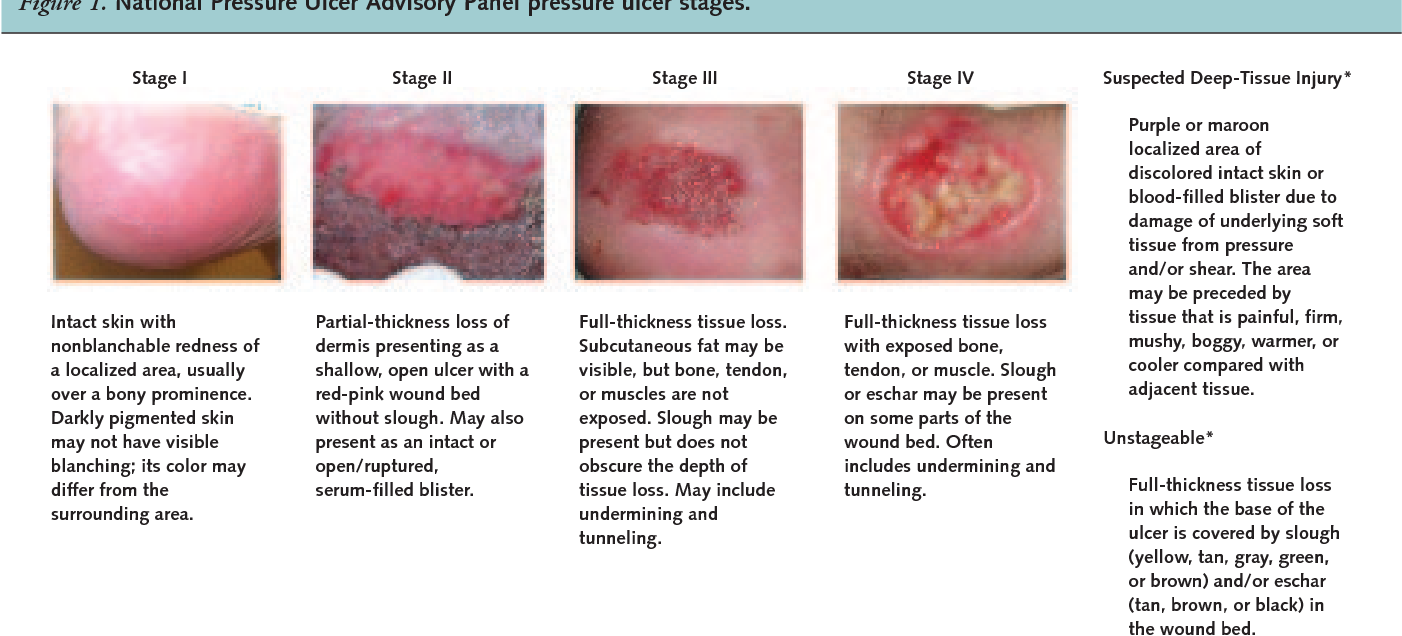
How To Identify A Stage Three Pressure Ulcer
When identifying a stage three ulcer, youll see a stark difference compared to stage one and two. During stage one, tissue injury is just beginning, but is not yet markedly visible. In stage two pressure injury development, the skin will open, forming a visible ulcer. Health care professionals and patients may see a small abrasion, a blood-filled blister or a dip in the skin. Tissue damage may become apparent, causing serious issues if not dealt with quickly.
However, stage three pressure ulcers are worse, extending down into the tissueparticularly where more adipose tissue is presentand often showing exposed fat. Stage three pressure ulcers may not even cause incredible pain. As can happen with deep tissue damage, they may progress quickly because they do not signal pain for the patient.
Here are some signs to keep in mind when monitoring for a stage three pressure ulcer:
- The skin has developed a crater, and might even include visible adipose tissue.
- The sore has a foul odor.
- The sore is oozing clear liquid, pus or blood.
- The sore may be covered by slough, but not in a way that destroys tissue visibility.
Symptoms Of Stage 3 And Stage 4 Pressure Ulcers
Stages 3 and 4 pressure ulcers have deeper involvement of underlying tissue with more extensive destruction. Stage 3 involves the full thickness of the skin and may extend into the subcutaneous tissue layer granulation tissue and epibole are often present. At this stage, there may be undermining and/or tunneling that makes the wound much larger than it may seem on the surface. Stage 4 pressure ulcers are the deepest, extending into the muscle, tendon, ligament, cartilage or even bone.
Figure 1: Stage 4 sacral pressure ulcerFigure 2: Stage 3 pressure ulcer on hip
Also Check: Foods To Avoid With Peptic Ulcer
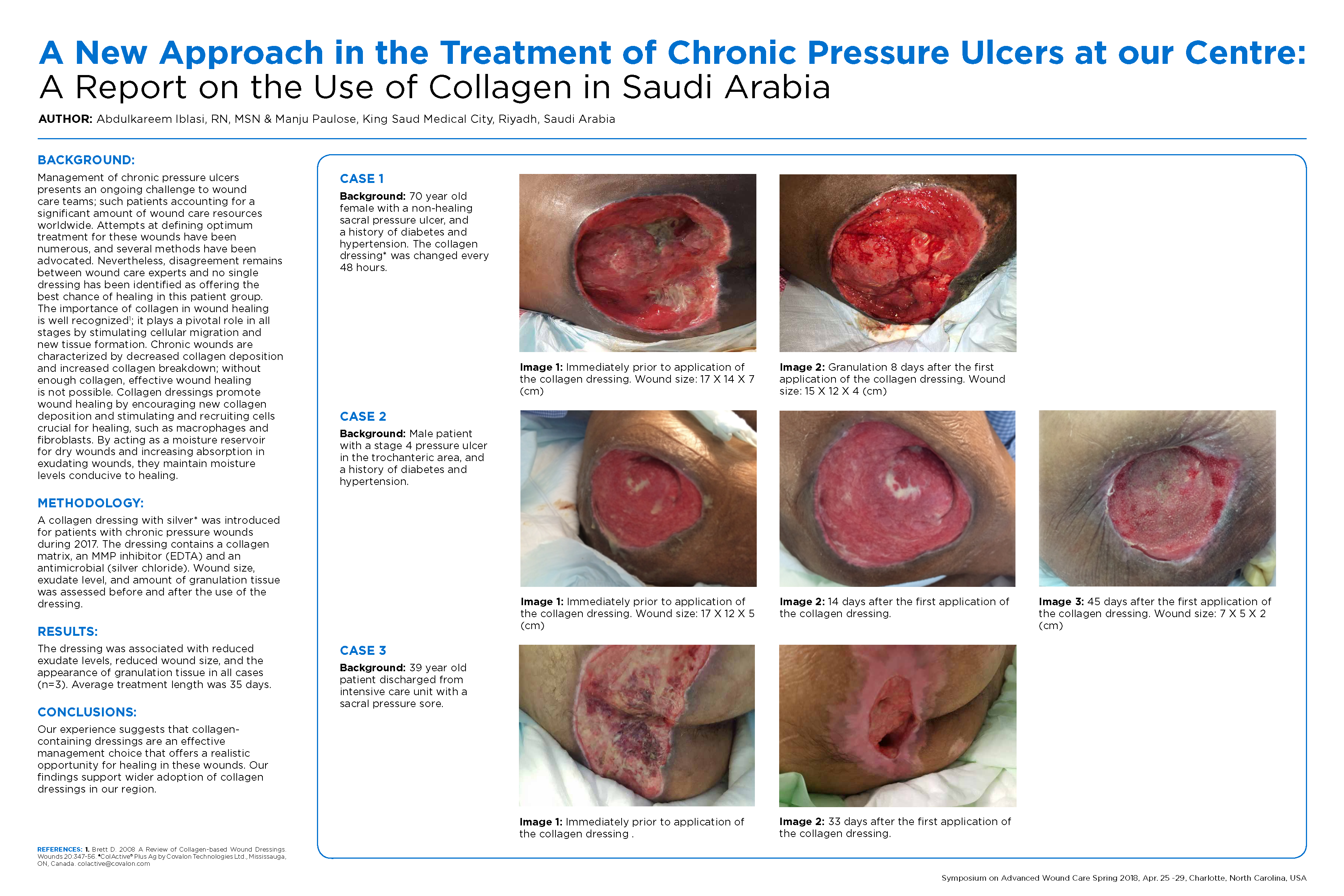
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
What Are Stage 3 Bedsores
Bedsores, also known as pressure ulcers or decubitus ulcers, are broken down into four stages based on their severity. Stage 3 bedsores have burrowed past the dermis and reached the subcutaneous tissue beneath.
Stage 3 bedsores pose a high risk of infection and can take months to heal from. Some pressure sores may even progress to the fourth and most dangerous stage without proper treatment.
Nursing homes that hire enough well-trained staff can often provide the care needed to prevent serious bedsores. If a nursing home resident develops a stage 3 bedsore, it may mean the facility is not properly caring for them.
Thankfully, there are ways to get help if your loved one develops a stage 3 bedsore. For example, loved ones can access medical care to keep a residents bedsore from worsening. They may also be able to take legal action against the nursing home to get compensation for treatment costs.
You May Like: Medical Management Of Ulcerative Colitis
Stage 3 Pressure Ulcers
- Helps to prevent biofilm formation
- Reduces healing time
It moistens wound dressings and dissolves encrusted bandages or wound dressings during dressing changes.
Prontosan® Gel X proper wound cleansing is essential. The use of Prontosan® Wound Gel X provides long-lasting cleansing and decontamination of the wound bed between dressing changes.
Prontosan® Debridement Pad has been designed to support the wound bed preparation when used in conjunction with Prontosan® Wound Irrigation Solution.
What Do I Do If I Have Questions
- Ask your doctor to explain anything you do not understand.
- This treatment cannot restore normal sensation in areas that have lost sensation because of the SCI.
- Ask for information that explains in detail all the possible risks and benefits of the treatment.
Read Also: Can You Feel A Stomach Ulcer
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Diagnosing A Stage 3 Bedsore
A medical professional relies on a bedsores appearance to diagnose its stage.
Stage 3 bedsores have the following characteristics:
- Black or rotten outer edges
- Crater-like indentation
- Dead, yellowish tissue
- Visible fat tissues
Stage 3 bedsores are quite deep, but tendons, ligaments, muscles, and/or bones will not be visible. If they are, the patient likely has a stage 4 bedsore. That said, health care providers may not be able to properly stage every severe bedsore.
Two complications may delay a stage 3 bedsore diagnosis:
- Deep tissue injuries: A deep tissue injury occurs when there is no open wound but the tissues beneath a patients skin are damaged.
- Unstageable injuries: If a doctor cannot see the base of the sore due to slough or eschar in the wound bed, they cannot make a diagnosis.
Even if a bedsore cannot be staged, doctors can still recommend treatments to start the healing process.
Donât Miss: Whatâs The Signs Of An Ulcer
You May Like: What Foods Not To Eat If You Have An Ulcer
What Are The Benefits Of This Treatment
It can take several months of bedrest for a severe wound to heal on its own. All pressure must be off the area while in bed, which can be very hard to do on an ongoing basis. If pressure is put on the area while in bed, it can delay healing or make the wound worse. Plus, there is an increased risk of infection with any open wound. The longer the wound is open, the longer the higher risk continues. If an infection develops, there is a risk that it can spread and become life-threatening.
The obvious benefit of this treatment is that the wound can heal much quicker than it would without the treatment. Your doctor can explain all your benefits, but here are a few of the benefits:
- Much less time needed for bedrest
- Lowered risk for infection
- Increased independence to enjoy meaningful activities
- Lowered healthcare costs