Living With Uc: Diet Changes
Although it has not been found that diet has an effect on ulcerative colitis, it generally is recommended that patients eliminate any foods that they find are making their symptoms worse. For example, milk in people with UC who are intolerant to the sugar in milk, lactose, may be causing gastrointestinal symptoms such as abdominal bloating, flatulence, and diarrhea, symptoms that may overlap with those of ulcerative colitis. Despite not being the cause of the ulcerative colitis, eliminating milk may improve gastrointestinal symptoms in these people. It is important to be sure that the diet is nutritionally adequate, and this may require the assistance of a dietician.
Donât Miss: Preventing Pressure Ulcers In Nursing Homes
Types Of Ulcerative Colitis
UC can be categorized according to the parts of the GI tract that it affects.
- Ulcerative proctitis. In ulcerative proctitis, only the rectum is inflamed. Its considered a mild form of UC.
- Left-sided colitis. Left-sided colitis causes inflammation in the area between the splenic flexure and the last section of the colon. The last section of the colon, known as the distal colon, includes the descending colon and sigmoid colon. Left-sided colitis is also known as distal ulcerative colitis.
- Proctosigmoiditis. Proctosigmoiditis is a form of left-sided colitis. It causes inflammation in the rectum and sigmoid colon.
Different tests can help a doctor diagnose UC. UC mimics other bowel diseases such as Crohns disease. A doctor will order multiple tests to rule out other conditions.
Tests to diagnose UC often include:
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
You May Like: Ulcerative Colitis Nausea In Morning
How To Prevent Ulcerative Colitis Flare
What are actionable steps you can take to make your symptom-free stretches last as long as possible? and stress management are probably the two biggest things as far as prevention goes, says Cohen. Parsley Health providers and health coaches often work with members who have ulcerative colitis to find a diet that helps them minimize flares and a stress management routine. Below, well dive into some specific ways to optimize your diet with natural remedies and make adjustments to your lifestyle while living with ulcerative colitis.
Read Also: What Should You Eat When You Have Ulcerative Colitis
Acute Severe Ulcerative Colitis
Patients with acute severe ulcerative colitis, defined as six or more bloody bowel movements per day and at least one of the following: pulse rate > 90 beats per min, temperature > 37.8°C, haemoglobin count < 10.5 g/dL, or ESR > 30 mm/h, should be admitted to a tertiary care centre.69 Acute severe ulcerative colitis is associated with significant morbidity and mortality of approximately 1%.138 Patients are initially treated with intravenous corticosteroids to which approximately 65% will respond.139 For patients not responding to intravenous corticosteroids within 3 to 5 days, rescue medical therapy with either ciclosporin or infliximab can be attempted. Both drugs are equally efficacious in acute severe ulcerative colitis.140,141 Delays in surgery can increase postoperative complications and mortality increases significantly after 7 days.142,143 If there is no response to one of these drugs, colectomy should be performed. Further discussion of acute severe ulcerative colitis is in the appendix.
Recommended Reading: What Foods Can You Eat With A Peptic Ulcer
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
How Long Do Ulcerative Colitis Flare
People with ulcerative colitis , a type of inflammatory bowel disease that causes inflammation and sores in the rectum and colon, experience bouts of symptoms or flare-ups, which are unpredictable and can last for days, weeks or even months. Having a treatment plan in place including medication, diet changes and flare-up reduction methods could help shorten a flare.
You May Like: When Does Ulcerative Colitis Develop
Also Check: Does Turmeric Help With Ulcerative Colitis
What Exams And Tests Diagnose Colitis
While unpleasant, the rectal examination is very important. Using a finger, the doctor feels inside the rectum, exploring for any masses or tumors. The color and consistency of stool can be evaluated, and if it is not grossly bloody, can be tested for occult blood .
Laboratory Tests
The history will assist the health-care professional decide the tests to order and what cultures would be appropriate. Blood tests help assess the stability of the patient, and also explore any potential issues associated with colitis.
- A complete blood count will assess the red blood cell count, the white blood cell count, and the number of platelets.
- The red blood cell count will help define the amount of bleeding.
- White blood cell counts elevate when the body is undergoing physical , physiological, or emotional stress.
- Platelets help blood to clot, so knowing the platelet number in a patient with bleeding may be useful.
Colonoscopy
Recommended Reading: How To Eat With Ulcerative Colitis
Make Sure Youre Getting Enough Probiotics And Prebiotics
Whether you take probiotics tablets, eat fermented vegetables or other fermented products, or take kefir, I personally try to intake something with probiotics and prebiotics at least a few times a week. My personal favourite is a kefir smoothie its an excellent combination of probiotics and prebiotics! Learn more about how to choose the right probiotics here.
You May Like: Foods To Avoid With Peptic Ulcer
Easing Symptoms During A Flare
The below suggestions can also help ease symptoms or help keep your body healthy during a flare-up.
Drink water: In UC, the large intestine can have a hard time absorbing water and salt, which can contribute to diarrhea and dehydration. Drinking plenty of water or an electrolyte replacement drink can help avoid dehydration if youre experiencing a flare.
Eat plain, easy-to-digest foods: During a UC flare, its common to lose your appetite. To keep your energy levels up and avoid malnutrition and weight loss, its important to continue to fuel your body with food. Unfortunately, fruits and vegetables, particularly when raw, are bothersome for many people with UC. Avoid fatty and greasy foods as well. Your doctor may also suggest meal replacement drinks if youre losing weight from UC flare-ups.
Get some exercise: If youre experiencing symptoms like stomach pain and diarrhea, exercise may sound like the last thing you want to do. But in addition to the well-known mood and health-boosting benefits of exercise, a workout can also have specific benefits for UC symptoms. Uncontrolled inflammation in the intestinal tract leads to UC symptoms. Exercise has an anti-inflammatory effect that can help these symptoms.
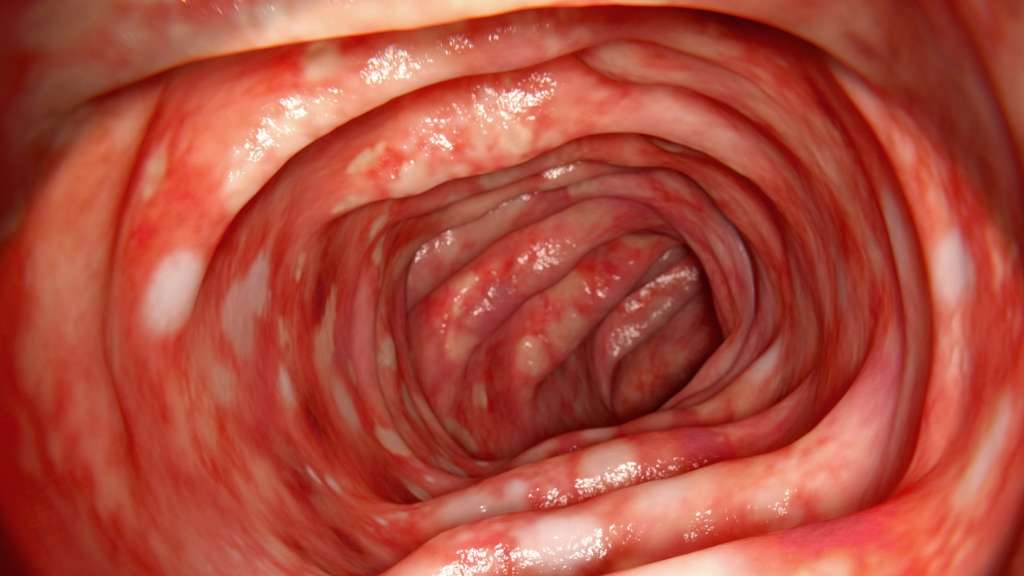
Signs Of Possible Colitis
General signs of colitis can include:
- Intense pain
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
You May Like: Ulcerative Colitis And Mental Health
Ulcerative Colitis Inflammation And How To Prevent It
Inflammation is one of those hot topic terms for diet and health. One of those words that gets thrown around all the time by health professionals, commercials, and wellness products. You know you should be avoiding it, and perhaps you know that there are foods and behaviors that help reduce it, but what is inflammation, why does it happen, and how is it related to ulcerative colitis?
Ulcerative colitis is a disease that affects the large intestine or colon. It is defined by the irritation and swelling caused by inflammation. In fact, its considered to be an inflammatory bowel disease. Unfortunately, theres currently no cure for ulcerative colitis, but the right treatments and lifestyle behaviors can help you feel like you have a handle of the condition. Reducing or preventing inflammation is a major step in improving the symptoms and suffering associated with ulcerative colitis.
Can Probiotics Prevent Flares In Ulcerative Colitis
Its a well-known fact that probiotics promote healthy bacteria in the gut and work to strengthen the immune system. These popular gut health supplements are also proving to be effective in preventing flares in UC.
Ulcerative Colitis is a disorder where aggressive luminal bacteria attack the mucosa causing inflammation. Probiotics, on the other hand, can help alter the existing bacterial environment to promote less aggressive and more anti-inflammatory bacteria.
Experts also agree that any therapy or treatment that works at the level of the mucosa should be considered, since Ulcerative Colitis is a mucosal disease.
New Research on Probiotics and Ulcerative Colitis:
Escherichia coli Nissle is a non-pathogenic strain of E. coli that rivals some of the top medications for the treatment of UC. In a number of large clinical trials, researchers compared it to the medical drug mesalamine and was found to be just as effective for both inducing and maintaining remission over a 1-year period.
VSL#3 is another potent probiotic that has shown to be effective for those with UC. It has a combination of the following strains: Bifidobacterium breve, B. longum, B. infantis, Lactobacillus acidophilus, L. plantarum, L. paracasei, L. bulgaricus, and Streptococcus thermophilus.This study of 32 UCpatients showed 77% of the patients went into remission after VSL#3 was administered for 6 weeks. *Consult a physician before using this medical food grade supplement.
Also Check: What Is Good For Ulcer Pain
Prevention By Lifestyle Adjustments
Ulcerative colitis can also be prevented by medication-free ways. Following a strict ulcerative colitis diet plan, for example, can reduce the frequency of painful experiences dealing with this disease.
Proper hydration also helps prevent ulcerative colitis. You should try to drink a lot of water every day, and avoid drinks such as coffee, alcohol and carbonated beverages, which may make your diarrhea worse.
Individuals with ulcerative colitis, or any inflammatory bowel disease for that matter, tend to stray from exercising, but this shouldnt be the case. Exercising can help control your ulcerative colitis symptoms and avoid diarrhea. Tai chi, yoga, breathing exercises and other simple activities should be done regularly to stay healthy.
Learning how to manage your stress may also help alleviate the signs and symptoms ulcerative colitis may bring about. A lot of stress may cause your regular digestive process to change, causing the stomach to produce more acids and empty at a slower pace. Some ways to reduce or control stress may be through exercises, relaxation and simple activities you could do any day, like listening to soothing music or reading a good book.
Natural Remedies For Uc Flares
Natural remedies are being studied, but none have been proven yet. The National Center for Complementary and Integrative Health notes that supplementing your standard treatments with meditation may be beneficial during a UC flare-up to help reduce symptoms, and that prebiotics and probiotics have shown promise in bringing about remission and helping people stay in remission when added to usual care.
Still, ulcerative colitis is a chronic, incurable condition, and symptoms may reappear unpredictably.
Also Check: Foods That Prevent Stomach Ulcers
You May Like: Is Ulcerative Colitis A Gastrointestinal Disease
Daily Life For People With Ibd
People with IBD lead useful and productive lives, even though they need to take medications. When they are not experiencing a flare-up of their disease, they feel quite well and are often free of symptoms.People with IBD can marry, enjoy sexual activity and have children. They can hold down jobs, care for families and enjoy sport and recreational activities.Even though there is currently no cure for IBD, medical therapy has improved the health and quality of life of most people with Crohns disease and ulcerative colitis. Research underway today may lead to further improvements in medical and surgical treatment, and even a cure.
Manage Symptoms Of Ulcerative Colitis Flare
How to deal with colitis flare-up can be approached different ways. Some people have reported that herbal remedies help manage their symptoms. Probiotics, the spice turmeric, and the herb boswellia have been used to control ulcerative colitis. Studies have also shown that gingko biloba has been effective in treating colitis in rodents.
Since stress has been linked to the disease, exercises like yoga and meditation are often recommended to patients. At the same time, certain foods have a higher chance of aggravating those who suffer from ulcerative colitis, so obviously avoiding such food items is a good idea. Some examples of foods to stay away from are, whole-grain bread, whole-grain pasta, beans, raw vegetables, and dried fruit. Keeping a diary of what you eat can often help you pinpoint what causes a flare-up.
A diary or journal can also help when you are taking medications. For example, if you experience a flare-up while taking an over-the-counter medication, discuss an alternative with your doctor and/or pharmacist.
When it comes to controlling ulcerative colitis flare-up, it can take time. Some people will have multiple triggers and wont be able to make all the necessary lifestyle adjustments all at once. Sometimes, just a few changes can make a huge difference though. The following simple steps have proved to help many people tame their flare-ups:
- Drinking small amounts of water throughout the day
- Reducing fatty foods
Also Check: Do You Still Have Ulcerative Colitis After Colectomy
Keep A Food And Symptom Journal
A key part of preventing flare-ups is knowing your personal ulcerative colitis triggers, which can vary from person to person. Some people are triggered by gluten and dairy, while some people arentso its important to identify what specific foods trigger you, says Cohen. Keeping up a food and symptom journal can be really helpful.
Start jotting down what you eat and drink in a notebook so you can identify foods and beverages that may be causing flares to occur. If you start to see a pattern emerge, you can try eliminating that food/drink for a while to see if you get some relief. Parsley Health doctors and health coaches can guide you through the appropriate way to eliminate and reintroduce foods and help you identify triggers.
Also Check: What To Do If You Have Ulcerative Colitis
Good Bacteria Might Help You Feel Better
UC has been linked to harmful bacteria in the gut. Probiotics are beneficial bacteria that help get rid of bad germs. Adding these supplements to your treatment could help keep you in remission.
No all probiotics are the same, however, and not all of them have evidence to show they can help with UC. People should speak to their doctor before using this option.
Don’t Miss: Low Dose Naltrexone Ulcerative Colitis
More Drugs That Work On Your Immune System
Other types of medicines for ulcerative colitis target your immune system, too. Your doctor may call these immunomodulators. They may be good options if 5-ASAs and corticosteroids havenât worked well for you.
The most common ones are azathioprine , mercaptopurine , and cyclosporine . Due to the risk of side effects, doctors usually save cyclosporine for people who donât have success with other meds. They may also try methotrexate paired with folic acid.
Ozanimod is an oral medication and is the first sphingosine 1-phosphate receptor modulator approved for patients with moderately to severely active UC.
The goal is to lower inflammation in your colon.
These drugs can have side effects. They can damage your liver and make you more likely to get skin cancers, lymphoma, and infections. If you take them, your doctor will test your blood and check you for skin cancer regularly.
Cyclosporine is especially strong, but it works fast. Your doctor might prescribe it to get a severe flare under control, and then give you 6-MP or azathioprine afterward. The drug may cause kidney problems, gout, infections, and high blood pressure.
It can take several months for some of these drugs to work. So your doctor may give you a faster-acting medicine, like a low dose of a corticosteroid, to help in the meantime.