Biomarkers And Microscopic Colitis: An Unmet Need In Clinical Practice
- 1Gastroenterology and Digestive Endoscopy Unit, IRCCS Policlinico San Donato, San Donato Milanese, Italy
- 2Institute of Pathology, Spedali Civili Brescia, Brescia, Italy
- 3Pathology and Cytodiagnostic Unit, IRCCS Policlinico San Donato, San Donato Milanese, Italy
- 4Department of Biomedical Sciences for Health, University of Milan, Milan, Italy
What Are The Causes Of Ulcerative Colitis
We do not yet know what causes this disease. Studies indicate that the inflammation in ulcerative colitis involves a complex interaction of factors: the genes the person has inherited, the immune system, and something in the environment. Foreign substances in the environment may be the direct cause of the inflammation, or they may stimulate the bodys defenses to produce an inflammation that continues without control. In patients with ulcerative colitis, once the patients immune system is turned on, it does not know how to properly turn off. As a result, inflammation damages the intestine and causes the symptoms of ulcerative colitis. One of the major goals of medical therapy is to help patients to better regulate their immune system.
Read Also: Icd 10 Stage 4 Sacral Ulcer
How Is Microscopic Colitis Treated
Treatment can vary depending on your symptoms and how severe they are. They range from dietary and lifestyle changes to over-the-counter and prescription medications. For some people, symptoms flare up and then go away on their own. Some people are able to manage their symptoms well with dietary changes alone, while others may need to use medication intermittently or more frequently.
Common medications include:
- Bulking agents, such as psyllium, to make your poop more solid and slow down its transit time.
- Anti-diarrheals that slow down your bowel contractions, such as loperamide or diphenoxylate.
- Bismuth Subsalicylate for diarrhea, acid reflux, nausea and indigestion.
- Budesonide, a corticosteroid thats absorbed in your colon, where it reduces inflammation.
- Mesalamine, a medication designed to treat ulcerative colitis, for inflammation and pain.
- Bile acid sequestrants , if you have bile acid malabsorption.
If you don’t respond to the above medications, and if your doctor believes there is an autoimmune factor involved, they might suggest additional medications to target your immune response, such as:
Additional recommendations from your doctor may include:
- Adjusting your preexisting medications.
- Identifying your specific food intolerances.
Read Also: How To Treat Ulcerative Colitis Pain
Who Does Microscopic Colitis Affect
Anyone can get it, but its more common in older people and people who were assigned female at birth. Its also more common in people who smoke, and in people who have certain autoimmune diseases, especially celiac disease. Microscopic colitis has traditionally been thought to be less common than other inflammatory bowel diseases. But because it requires a tissue sample to diagnose, its likely underestimated.
Fecal Proteins From Other Leukocytes

Molecules produced by other types of inflammatory cells have been considered, as well. The mast cells are located in the mucosa of different organs and tissues and are the main actors in allergic reactions. The role of mast cells in inflammatory conditions of the gut is not completely understood yet however, it is known that mast cells have an increased propensity to release tryptase in UC . The presence of this enzyme in fecal matter was also studied in CC patients, and detectable levels of fecal tryptase were present in about 50% of CC patients, as compared to 13 and 5% of IBS patients and healthy controls, respectively .
In the same paper, Lettesjö et al. also measured the fecal levels of two potent pro-inflammatory molecules, those being interleukin 1 and tumor necrosis factor -. These cytokines are produced and released primarily by mucosal macrophages but also by many different inflammatory and non-inflammatory cell types. Indeed, their role and overexpression in active IBD is well established , thus suggesting the rationale to test them in MC. Despite this premise, only 18% of patients affected by CC presented with enhanced fecal IL-1 levels, while levels in the other experimental groups were very low or undetectable, and TNF was not detectable in any stool sample .
Read Also: Ulcerative Colitis And Back Pain
Mc Diagnosis Requires Histological Examination Of Colonic Biopsies
Histological assessment of MC needs to be based on stepped biopsies of the colon, with a minimum of two biopsies taken from each of the ascending, transverse and descending/sigmoid colon in separate specimen containers. MC occurs in two histologically distinct forms: collagenous colitis and lymphocytic colitis . In both CC and LC, inflammation in the lamina propria is present throughout the entire colon. The key histological feature distinguishing CC is the presence of a broad subepithelial collagen band, > 10 µm in thickness, immediately underneath the surface epithelium. The key histological feature that distinguishes LC is an increased number of intraepithelial lymphocytes , with > 20 IELs per 100 epithelial cells generally considered diagnostic. Another MC group may also exist, referred to variably in the literature as MC not otherwise specified, paucicellular LC or, most recently, MC incomplete . In patients with MCi, the collagen layer or number of IELs is abnormal, but below the threshold for CC or LC, though there is still inflammation in the lamina propria.
What Are The Risk Factors Of Ulcerative Colitis
It is estimated that as many as one million Americans have IBD with that number evenly split between Crohns disease and ulcerative colitis. Males and females appear to be affected equally. The usual age of diagnosis with ulcerative colitis is in the mid-30s, although the disease can occur at any age. Men are more likely than women to be diagnosed with ulcerative colitis in their 50s and 60s. The incidence is greater in whites than non-whites, and a higher incidence is found in Jews than in non-Jews.
IBD tends to run in families. Studies have shown that up to 20 percent of patients with ulcerative colitis will have a close relative with either Crohns disease or ulcerative colitis. There is no way to predict which, if any, family members will develop ulcerative colitis.
Don’t Miss: What Do You Do For A Stomach Ulcer
What Is The Difference Between Collagenous Colitis And Lymphocytic Colitis
Microscopic colitis is an inflammatory bowel disease that usually starts in the colon or rectum, although it is not the same condition as Crohns disease or ulcerative colitis. It gets its name from the fact that inflammation can only be seen under a microscope during an endoscopy.
There are two forms of microscopic colitis: collagenous colitis and lymphocytic colitis. Although the two forms share many similarities under the umbrella of microscopic colitis, there are a few key differences.
Allergic Colitis In Infants
Allergic colitis is a condition that can occur in some infants who are breastfeeding. The only symptom thats usually found is blood in the stool.
This condition may result from a food allergy, but the cause is not well understood. Tests such as endoscopy arent usually done but the diagnosis is based on the occurrence of bloody stools.
The bloody stools normally resolve on their own, but the possibility of a food allergy should be looked into. This includes removing foods from the breastfeeding parents diet. Usually this begins with removing dairy products for several weeks and seeing if that makes any difference.
Other foods that commonly cause allergies might also be stopped if the bloody stools dont improve. In some cases, a special formula might be recommended for feeding.
You May Like: Low Residue Diet For Ulcerative Colitis
How Is Lymphocytic Colitis Diagnosed
You may need to see a gastroenterologist. This is a doctor with special training to treat problems of the digestive tract.
Your healthcare provider will ask you about your health history and your symptoms. Your healthcare provider will give you an exam, including an exam of your belly .
Your healthcare provider will rule out other causes of your diarrhea. These can include an infection or another inflammatory bowel disease.
Your healthcare provider will also do other tests. These may include:
- Blood tests, to check for anemia and infection
- Tests for celiac disease
- Stool analysis, to check for inflammation or infection
- Imaging tests of the intestines. These include a CT scan, MRI, or an upper GI series.
You may also need a colonoscopy. This test looks at the lining of your colon and rectum. It uses a light and a tiny camera.
The colon often looks normal on a colonoscopy. During the colonoscopy, your healthcare provider can take out tissue samples of your colon. Then he or she will look at it under a microscope to tell if you have lymphocytic colitis.
Similar Symptoms With Important Differences: Colitis Vs Ibs
The main symptoms of colitis are ongoing diarrhea and pain in the stomach. Some people will feel very tired or even exhausted, and they may also lose weight and find that their appetite goes down. Sufferers of the ulcerative type may find that when they pass a bowel movement, they also pass blood or mucus however, blood is not present in microscopic colitis.
Irritable bowel sufferers can have ongoing diarrhea as a key symptom, but they may also swing from diarrhea to constipation or only ever have constipation. Unlike colitis, IBS does not cause bleeding as the bowel itself is intact, so even a severe bout of IBS does not damage the gut. Weight loss and fatigue are also not symptoms of IBS, but stomach pain definitely is, along with bloating and an urgent need to get to a bathroom.
Usually IBS sufferers only experience bowel and stomach symptoms, but colitis can cause problems with other parts of the body such as painful swelling of the joints, eye or skin irritation and mouth ulcers. If the condition is very severe, patients can also have a high temperature or fast heartbeat.
Colitis is similar to IBS in that it can come and go over time. Patients with both disorders might refer to a flare-up when their symptoms are particularly bad, but they will usually have times when they feel much better and the symptoms are in remission.
Don’t Miss: How To Heal Ulcerative Colitis With Food
What Kind Of Doctor Diagnoses And Treats Colitis
Most often colitis is treated by a primary health care provider or internal-medicine specialist, especially when the colitis is first diagnosed and the cause is uncertain. Once the cause is found, that health care provider may be the only person needed to continue care. Should there be a need for further investigation and diagnostic testing, specialists may be consulted, such as a gastroenterologist. If an infection is the cause of colitis, an infectious-disease specialist may be consulted. In some cases, other specialists may be involved in treatment, such as surgeons and interventional radiologists.
Patient history
Follow Up With Your Doctor
You may only need at-home or short-term care for some kinds of colitis. But UC is a condition youâll have for the rest of your life. And it affects everyone in a different way. Youâll need to work with your doctor to find a treatment plan that works for you.
No matter whatâs causing your symptoms, get medical care right away if you have:
- Watery diarrhea for more than a few days
- Heavy, ongoing diarrhea
Read Also: Ways To Prevent Pressure Ulcers In Hospitals
Getting To A Diagnosis
Theres no doubt that IBD can significantly decrease quality of life, between uncomfortable symptoms and frequent bathroom visits. IBD can even lead to scar tissue and increase the risk of colon cancer.
If you experience any unusual symptoms, its important to call your doctor. You may be referred to a gastroenterologist for IBD testing, such as a colonoscopy, sigmoidoscopy, or a CT scan. Your doctor may also order blood and fecal testing. Diagnosing the specific form of IBD will lead to more effective therapies.
Commitment to daily treatment and lifestyle changes can help minimize symptoms, achieve remission, and avoid complications.
Regardless of your diagnosis, Healthlines free app, IBD Healthline, can connect you with people who understand. Meet others living with Crohns and ulcerative colitis through one-on-one messaging and live group discussions. Plus, youll have expert-approved information on managing IBD at your fingertips. Download the app for iPhone or Android.
Treatments For Ibs And Ibd
Treatment is very different for IBS and IBD. If you have IBD, you will take medications that lower the inflammation in the GI tract such as anti-inflammatory medications, biologic agents, and immunomodulators which can reduce the damage IBD is causing.
Treatment of IBS is different. You and your providers will focus on treating the specific symptoms you are having. Changes to your diet and exercise habits are a good first step.
Heres a few examples of some foods to avoid when you have IBS:
If diarrhea is one of your main IBS symptoms, you might take medications that reduce the diarrhea, such as rifamixin and eluxadoline . If you are more often constipated, you might take medications that help keep the GI tract moving, such as lubiprostone , linaclotide , or plecanatide .
You might also need treatment of stress, anxiety, or depression with medications or therapy if you and your provider think this is playing a role in your IBS.
Read Also: Foods To Avoid During Ulcerative Colitis Flare Up
Main Difference Colitis Vs Ulcerative Colitis
Colitis and ulcerative colitis are two medical conditions which affect the colon. These two terms often used interchangeably since they share similar signs and symptoms. But, it is important to distinguish the difference between them in order to make an accurate diagnosis and treatment. The main difference between colitis and ulcerative colitis is that ulcerative colitis is one form of colitis which results in the chronic inflammation of colonic mucosa and rectum giving rise to ulceration and bleeding.
1. What is Colitis ? Causes, Signs and Symptoms, Diagnosis, and Treatment
2. What is Ulcerative Colitis? Causes, Signs and Symptoms, Diagnosis, and Treatment
3. What is the difference between Colitis and Ulcerative Colitis?
What Causes Ulcerative Colitis Vs Crohns Disease
Its not entirely known what causes ulcerative colitis or Crohns disease. However, experts believe it has something to do with genetic factors and environmental factors . Your gut microbiomethe bazillion bacteria that live in your digestive tractis thought to have influence as well. In fact, a 2020 study published in the journal Frontiers of Medicine, found that not only was the gut bacteria in people with IBD different from people without IBD, but it was also different between people with ulcerative colitis vs. people with Crohns disease.4
What is known is that something sets off your immune system to mistakenly attack healthy areas of your digestive tract, causing chronic inflammation.
This overreaction of the immune system can also affect areas outside of your digestive system and can include your skin, eyes, and other organs. This can occur with both ulcerative colitis and Crohns disease, but ulcerative colitis is more likely to affect the skin, eyes, and bones, while Crohns disease is more apt to affect the kidneys and gallstones.1
Read Also: What Is Good For Ulcers
You May Like: Can Ulcerative Colitis Cause Fever
Pitfalls And Errors In The Diagnosis Of Microscopic Colitis
The motivation degree of the involved physicians is essential in the diagnosis of microscopic colitis. The gastroenterologist should refer every patient with chronic watery diarrhea to perform a colonoscopy in spite of the benign course of the disease and the absence of alarm symptoms or signs. The endoscopist should take multiple stepwise biopsy samples of the colonic mucosa despite that the mucosa looked macroscopically normal. Finally, the pathologist should be motivated to use objective histological criteria to make the diagnosis.
Differences Between Ulcerative Colitis And Crohns Disease
The differences between ulcerative colitis and Crohns disease are:
- In Crohns disease, there are healthy parts of the intestine mixed in between inflamed areas. Ulcerative colitis, on the other hand, is continuous inflammation of the colon
- Ulcerative colitis only affects the inner most lining of the colon while Crohns disease can occur in all the layers of the bowel walls
Dont Miss: Ulcerative Colitis Flare Up Treatment Guidelines
Read Also: Prevention Of Diabetic Foot Ulcer
Getting The Right Diagnosis
Your doctor will ask about the type and timing of your symptoms. Theyâll probably feel your belly to see if itâs tender. Let them know about any medications that you take and if anyone in your family has ever had IBD or other digestive issues.
Everything you tell your doctor gives them clues about other tests you might need, such as:
Stool samples and bloodwork. Your poop and blood can reveal signs of infection or inflammation. Blood tests can also show low levels of iron. Thatâs called anemia. It can happen when colitis causes a lot of bleeding in your colon.
Imaging. Your doctor may take pictures inside your colon or rectum. They might use a special liquid called barium for some tests. Thatâs a substance thatâll coat your colon to help it show up better on X-rays.
You may also need:
- Magnetic resonance imaging scans
- Computed tomography scans
Endoscopic tests. An endoscope is a camera attached to a thin, bendy tube. Your doctor can use it to look at your lower colon and rectum or entire colon .
Tissue biopsy. Your doctor may remove some tissue during a colonoscopy or sigmoidoscopy. A lab technician will use a microscope to check for signs of inflammation or other abnormal cells.
Clinical And Histological Diagnostic Criteria
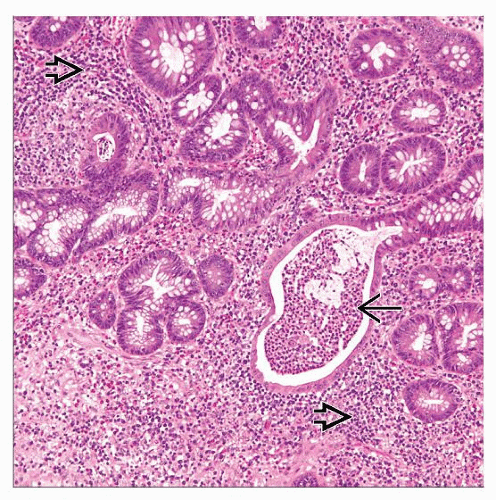
The diagnosis of both CC and LC is based on a compatible clinical picture and well-established objective histological criteria. Clinical criteria include chronic or recurrent watery diarrhea of at least 1-month duration, and grossly normal or slightly abnormal full colonoscopy. The histological criteria are: increased chronic inflammatory infiltrate in the lamina propria increased number of intraepithelial lymphocytes and damage of surface epithelium, with flattening of epithelial cells and/or epithelial loss and detachment, and minimal crypt architecture distortion. Histological diagnosis of CC requires the additional presence of an abnormal surface subepithelial collagen layer with a thickness 10 µm, which entraps superficial capillaries and with an irregular lacy appearance of the lower edge of the basement membrane . A number of IEL higher than 20 lymphocytes per 100 epithelial cells in the absence of a thickened subepithelial collagen layer is necessary to diagnose LC . Immunohistochemistry for tenascin expression is used in doubtful cases, since it allows a better detection of the thickened subepithelial collagen layer .
There are no significant differences in clinical presentation between CC and LC. However, there are sex differences between both entities. In CC there is a clear female predominance, which is not as marked in LC . , Median age at diagnosis in the different population-based studies ranges from 58 to 68 years in CC, and 59 to 70 years in LC. ,
Recommended Reading: Nurses Role In Pressure Ulcer Prevention