Pressure Ulcers Vs Bedsores
Pressure Ulcers are also known as Bedsores, Decubitus Ulcers, Pressure Sores, or Pressure Injuries. However, while Pressure Ulcers can develop during prolonged surgery or a hospital stay, a Bedsore generally develops on a person who has been immobile for long periods. It can be someone confined to a wheelchair or who cannot get out of bed.
Prevention Of Pressure Ulcers: Nurses Sole Responsibility
| Paper Type: Free Essay |
Pressure ulcer is a major health problem. According to previous 10 years nationwide studies, 10% to 15% of the general population suffers from chronic pressure ulcers. In addition, Reddy, Gill and Rochon approximated 60,000 patients every year will die from hospital acquired pressure ulcers and the treatment of these wounds costs approximately $11 billion per year. These findings are significant in some areas such as patients in intensive care units, critical care units and nursing home residents. These situations cost patient in terms of suffering, impaired quality of life, reduced independence and even increased morbidity and mortality. The patients delay in hospital discharge and decrease the efficiency and efficacy of health services. The health industry is also concerned about lack of sources, work force hours to manage the problem. Various industries and government agencies are disconcerted to either treat these ulcers in early intervention or encourage prevention . However, a good quality care is important in preventing these sores and nurses come at front to provide this care. In identifying the nurses attitude towards care and perception of barriers in that case may solve this situation.
Search strategy
If you need assistance with writing your essay, our professional essay writing service is here to help!
Nurses knowledge and attitude
Use of appliances in practice
Hospital policy
Patients status
Establishment Of A Pressure Ulcer Specialist Nurse
A specialist nurse dedicated to pressure ulcer prevention was established at the hospital for a period of 2 years with funds from TrygFonden, a Danish foundation to promote safety. Together with the steering committee, the specialist nurse had overall responsibility for implementation of the guidelines in clinical practice in all 50 departments at the hospital and for the establishment of an internal organisation to support implementation. The specialist nurse also became a consultant that every nurse or nurse assistant at the hospital could contact for supervision and specialist advice in the prevention and treatment of pressure ulcers and other skin damage, such as incontinence-associated dermatitis.
The pressure ulcer nurse was very visible in the departments at OUH and arranged training and bedside instruction in the treatment of pressure ulcers. In 2016, the role of pressure ulcer specialist nurse was made permanent.
Recommended Reading: Can Ulcers Cause Heart Palpitations
Initiating The Prevention Emergency Project
Informal discussions between nursing leaders about the need for action on pressure ulcers in the ED began in 2015 and the situation was monitored carefully during 2016 and 2017. By the spring of 2018, it was clear that the ED would benefit from direct intervention, therefore ED nursing leaders and the head of innovation at KUH collaborated with Mölnlycke Health Care AB of Sweden, a manufacturer of protective bed surfaces, to plan, launch and implement a new model of care capable of preventing pressure ulcers, improving patientsâ experiences and enhancing staff satisfaction.
The PEP started with a literature review of best practice related to pressure ulcer prevention in EDs, a consultation with an external expert on pressure injury prevention and wound healing, study visits to progressive US hospitals, and extensive interviews and workshops with ED nurses to understand the challenges and realities of workflow in the department.
The review demonstrated that the four main elements of best practice in pressure ulcer prevention in EDs were:
-
⢠Adaptation and routine use of a pressure injury risk assessment tool for every patient.
-
⢠Use of preventive bed surfaces, such as dynamic air mattresses or pressure-relieving equipment to redistribute pressure from sensitive tissue areas for at-risk patients.
-
⢠Intentional rounding of at-risk patients at regular intervals.
-
⢠Easy access to prophylactic dressings such as heel and sacral covers, and incontinence pads.
Treatments For Pressure Ulcers
Treatments for pressure ulcers depend on how severe they are.
For some people, they’re an inconvenience that needs basic nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning.
Ways to stop pressure ulcers getting worse and help them heal include:
- applying dressings that speed up the healing process and may help to relieve pressure
- moving and regularly changing your position
- using specially designed static foam mattresses or cushions, or dynamic mattresses and cushions that have a pump to provide a constant flow of air
- eating a healthy, balanced diet
- a procedure to clean the wound and remove damaged tissue
Surgery to remove damaged tissue and close the wound is sometimes used in the most serious cases.
Read more about the treatments for pressure ulcers.
You May Like: How To Gain Weight With Ulcerative Colitis
Counting Days With No Pressure Ulcers
Manual registration of days without pressure ulcers was established in each department. This method was dependent on the nurses and nurse assistants registering patients with pressure ulcers every day. Every time a department achieved 200, 300, 400 or 500 days without pressure ulcers, they celebrated the achievement . The celebration was shared on the hospital’s internet site with photographs to inspire staff in other departments. The aim of this method was not to compare the individual departments, because they had different patient populations with different risks.
Pressure Ulcer Nursing Care Plans
A pressure ulcer is a localized skin injury where tissues are compressed between bony prominences and hard surfaces such as a mattress. They are caused by pressure in combination with friction, shearing forces, and moisture. The pressure compresses small blood vessels and leads to impaired tissue perfusion. The reduction of blood flow causes tissue hypoxia leading to cellular death.
Don’t Miss: Does Gluten Affect Ulcerative Colitis
When To Get Medical Advice
If you’re in hospital or a care home, tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer. It’ll probably continue to get worse if nothing is done about it.
You should be regularly monitored and offered advice and treatment to reduce the risk of pressure ulcers, but sometimes they can develop even with the highest standards of care.
If you’re recovering from illness or surgery at home, or you’re caring for someone confined to bed or who is a wheelchair user, contact your GP surgery if you think you or the person you’re caring for might have a pressure ulcer.
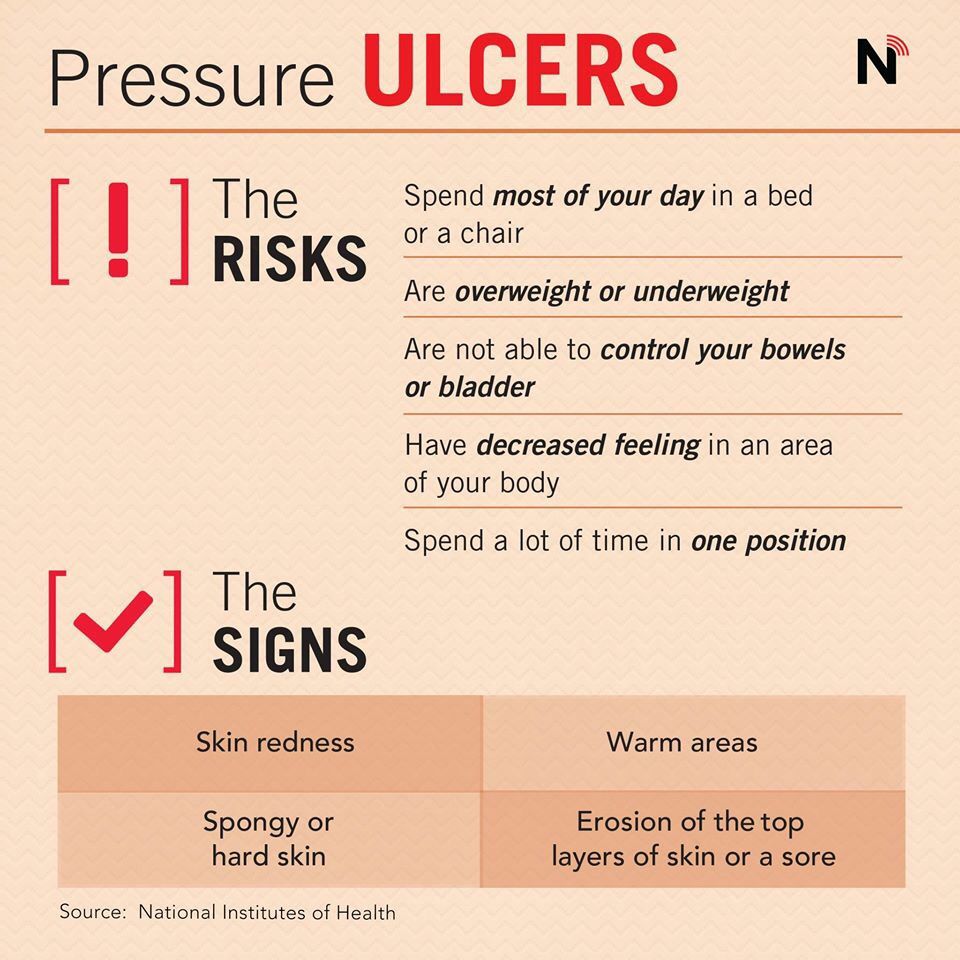
Get medical advice immediately if there is:
- red, swollen skin
- pus coming from the pressure ulcer or wound
- cold skin and a fast heartbeat
- severe or worsening pain
- a high temperature
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
Guidelines For Pressure Ulcer Prevention
The pressure ulcer guidelines for the southern Denmark region are based on the Braden scale , the pressure ulcer bundle from the safer hospital programme and the EPUAP guidelines . The guidelines prescribe early risk assessment of pressure damage and describes prevention methods and how to document observations and preventive actions .
The pressure ulcer bundle from the Danish Safer Hospital Programme states:
Also Check: How Do You Heal An Ulcer
Pressure Ulcer Prevention Theme Days
Every year since 2014 the hospital has arranged a theme day with a focus on pressure ulcer prevention. The programme consists of presentations from different departments at OUH and presentations about clinical topics from the pressure ulcer specialist nurse. Since 2016 colleagues from primary care have been invited to attend, and during the past 3 years there have been presentations from primary care staff. In 2016 a theme day for clinicians from the other five hospitals and primary healthcare areas in the southern Denmark region was held. In 2018, OUH hosted a presentation by Professor Dimitri Beeckman, President-Elect of EPUAP.
The Important Nursing Role In Bedsore Prevention
- May 29, 2017
- Filed under: medical malpractice, hospitals, nursing homes, patient safety
In my career as a Houston medical malpractice attorney, I have represented numerous clients who were seriously injured as a result of pressure ulcers.
Pressure ulcers are also known as bedsores or decubitus ulcers. The National Pressure Ulcer Advisory Panel defines them as a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear. Bedsores sometimes may be present with intact skin, but also commonly are very painful open ulcers.
The pressure injury staging scale
The standard of care requires doctors and nurses to identify, and document in the medical records, pressure injuries according to a staging system that is based on the degree of tissue damage.
Stage I Pressure Injury: Non-blanchable erythema of intact skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple or maroon discoloration these may indicate deep tissue pressure injury.
Stage II Pressure Injury: Partial thickness skin loss with exposed dermis. Wound bed is viable, pink or red, moist, and may present as an intact or ruptured serum filled blister. Adipose and deeper tissues are not visible.
Bedsores can develop quickly
Standardized nursing pressure injury prevention tools
Preventing bedsores
What you can do
We are here to help
You May Like: Children’s Mouth Ulcers Treatment
The Closed Pressure Ulcer
The closed pressure ulcer is a difficult lesion to diagnose. It has the appearance of a small wound, but inside is an insidious Stage IV-type lesion. Closed pressure lesions are frequently overlooked, with the result that patients who develop these can die from an infection. Most often, these ulcers are not detected until postmortem examination.
Pressure Injury Risk Assessment
The Norton pressure ulcer risk assessment scale was being used at KUH however, most ED nurses found it too long and time-consuming to use properly and consistently. Therefore, the scale was abridged to include minimal criteria for assessment of risk of pressure ulcer development . Posters showing these criteria were displayed prominently at the entrance to the ED alongside a digital screen showing a 45-second instructional video designed to educate and remind paramedics that when handing over patients to the triage nurses, they must communicate clearly if patients met the inclusion criteria and should be identified as at-risk. The triage nurse would then record this information in the patientâs electronic medical record , which would trigger fields and alarms prompting the nurse to undertake an initial skin assessment, ensure a turning and positioning system was in place, and ensure that prophylactic dressings were available.
Box 1.
Read Also: How To Cure Tongue Ulcer
Attitudes Of Nurses To The Prevention Of Pressure Ulcer Among Patient In Hospitals
by The Document Co | Jul 23, 2019 | Article Service For Health Care |
This article consists of 23 pages and 7,000 words. Attitudes of nurses In order to get fill access to this article, please email us at Thedocumentco@hotmail.co.uk
Chapter 3.0. Critical Review of Literature
In order to perform a significant and critical review of the literature, four articles have been selected as mentioned in the preceding section. Before the presentation of discussion and review of the research, a thorough explanation of specific notions of each article has been summarised into tabular form. The critiquing framework used for the purpose is adopted from the works of Holland and Rees . The table is displayed in Appendix 4 of this dissertation.
3.1. Critical Review of the Recruited Articles
The most recent study conducted by Sving et al., was mixed method research. The study focused on explaining the practices of registered nurses in regard to the prevention of pressure ulcer within the wards of general hospitals located in Central Sweden.
Sving et al implemented a descriptive approach with the help of multi-method consideration. The participating registered nurses were from three different clinical settings in central Sweden including medical, geriatric and an orthopaedic ward.
Pressure Ulcers Vs Pressure Injury: What’s The Difference
A pressure injury is caused by high pressure, continuous pressure, or pressure combined with shear and or friction, which occurs in the skin or the localized damage of the underlying soft tissue under the skin. A pressure ulcer, also known as Bed Sore, is a type of pressure injury a lesion caused by unrelieved pressure that results in damage to underlying tissue.
Most common pressure ulcer areas are bony prominences including the following:
- The back of the head and ears
Also Check: How Can You Get Rid Of Ulcers
Study Design And Setting
Institutional based cross-sectional multi-center study using quantitative method was conducted from August 1322, 2018. Thera are 10 public hospitals functional in Wollega zones. The study setting includes five public hospitals including one teaching hospital , five Public Referral Hospitals: Nekemte, Gimbi, Nedjo, and Shambu Referral hospitals. Among ten hospitals, the investigators purposively selected five hospitals where large number of patients visit, referred and admitted. Wollegas main town is 330km to the west from the capital city of the country, Addis Ababa, Ethiopia. .
Swedish missionaries introduced the modern nursing to Ethiopia around 1866. Then, Russia and French were delivering the nursing service in limited areas of Ethiopia. After the Second World War , the Ethiopian Red Cross Society established the first nursing school in at Haile Selassie I hospital. Swedish Missionaries at the Princess Tsehai Memorial Hospital opened the second nursing school. These two nursing schools were only admitting females to train in nursing profession. Males were admitted to nursing programs in 1954 in Ethiopia in Nekemte nursing school found in the current study area, Wollega zones. Currently, in Ethiopia nursing profession could be educated after completed grade ten or twelve .
Data Processing And Analysis
The data collected were checked for completeness and entered into Epi data V.4.6.0.2. Analyses were done by SPSS V.25. Bivariate and multivariate logistic regression models were used to identify factors associated with PI prevention practice. In bivariate analysis, the association was tested with each independent variable and dependent variable separately. The variables with a p0.25 in bivariate analysis were taken into the multivariable model to control for all possible confounders. ORs with 95%CI were estimated to identify the factors associated with PI prevention practice using multivariable logistic regression analysis. The level of statistical significance was declared at a p< 0.05.
Also Check: Meal Replacement Shakes For Ulcerative Colitis
Study Setting And Design
A Hospital-based cross-sectional study design was conducted at WSUTRH, which has 268 beds and 246 staff nurses. The hospital provides services to 3.55million people annually for the neighbouring areas of Wolaita and Dawuro, Gamo Gofa and Kambata Tambaro. The study was carried out from 1 July 2019 to 30 July 2019.
Implementing A Prevention Plan
Preventing pressure ulcers can be nursing intensive. The challenge is more difficult when there is nursing staff turnover and shortages. Studies have suggested that pressure ulcer development can be directly affected by the number of registered nurses and time spent at the bedside., In contrast, however, one recent study suggested that there was no correlation between increasing the nurse-to-patient ratio and the overall incidence of pressure ulcers. Donaldson and colleagues noted that this particular study was limited by the fact that the researchers could not affirm compliance with ratios per shift and per unit at all times. Given that the cost of treatment has been estimated as 2.5 times that of prevention, implementing a pressure ulcer prevention program remains essential.
A key component of research studies that have reported reduction of pressure ulcers is how to sustain the momentum over time, especially when the facility champion leaves the institution. It is clear from the evidence that maintaining a culture of pressure ulcer prevention in a care setting is an important challenge, one that requires the support of administration and the attention of clinicians.
Don’t Miss: How To Cure Duodenal Ulcer
Prevention Emergency Project Pressure Ulcer Risk Assessment Criteria
-
⢠Patients with suspected hip fracture
-
⢠Patients aged over 75 years for whom the answer to any of the following questions is yes:
-
⢠Has the patient reduced their intake of nutrients and/or fluids, and do they have reduced mobility?
-
⢠If the patient has reduced mobility, is it difficult for them to change position without help?
-
⢠Does the patient have reduced general health ?
Stage : Pressure Ulcer Stages
Stage I pressure ulcer exhibits an observable, pressure-related alteration of intact skin. It looks like reactive hyperemia, but it is not blanchable. . Changes in sensation, temperature, or firmness may precede visual changes, but color changes do not include purple or maroon discoloration as these may indicate deep tissue pressure injury. Symptoms can be pain, burning, or itching. It is important to stop the pressure by changing the patient’s position or using foam pads, pillows, or mattresses.
Read Also: Ulcerative Colitis And Lower Back Pain
Sample Size And Sampling Procedure
The sample size was determined by using a single population proportion formula with the assumption of 54.4% Proportion , 95% confidence level and 5% margin of error. Since the source of the population was less than 10,000 , a correction formula was used. Using 10% nonresponse the final sample size obtained was 220. Then, the number of participants in each selected hospital to take a similar proportion of participants were determined using the proportionate population sampling.