Increased Severity Of Back Pain After Uc Diagnosis
Anyway, over the years I used yoga to manage my pain. Sometimes I only experienced dull twinges. Other times I had to take a day to ice it so I could walk normally and bring down the pain level. But it never was as bad as it was in the beginning-until I moved back home.
I had forgotten how terrible the pain was. And after experiencing that awful two week period of constant bathroom visits and abdominal spasms, I thought nothing else could be as painful. After I got stuck in the backyard on my stomach because I couldnt get up, my parents shoved a phone in my hand and told me to call a doctor.
This time though I was armed with some new information. I had been doing some reading on ulcerative colitis and discovered that UC can affect other parts of the body, sometimes years before there are any signs of bowel disease.
Joints can be affected and in rare cases, there can be inflammation of the joints in the spine and pelvis. When I saw a doctor this time, I was still experiencing a lot of pain and he was able to better observe what I was going through.
Unfortunately, he could not prescribe me anything. All the stronger pain medications have anti-inflammatory drugs in them, which can cause bleeding in people with inflammatory bowel disease. I was referred to physical therapy, where I was told, once again, that it was SI joint dysfunction.
Symptoms Of Ulcerative Colitis
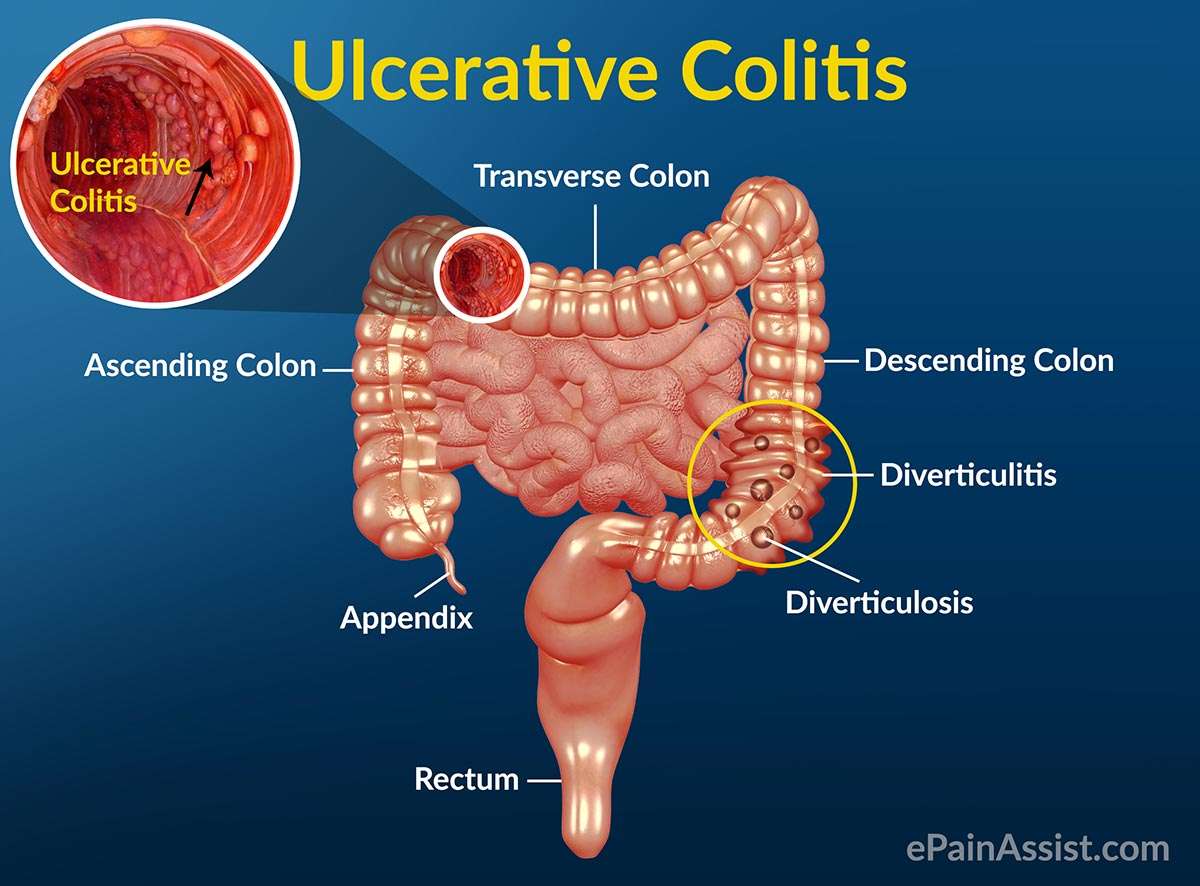
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- feeling tired
- dehydration
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Basics Of Inflammatory Bowel Disease
Arthritis means inflammation of joints. Inflammation is a body process that can result in pain, swelling, warmth, redness and stiffness. Sometimes inflammation can also affect the bowel. When it does that process is called inflammatory bowel disease . IBD is actually two separate diseases: Crohn’s disease and ulcerative colitis.
Also Check: Colon Cancer Symptoms Vs Ulcerative Colitis
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Can You Die From Ulcerative Colitis
Ulcerative colitis usually isnt fatal, according to the Mayo Clinic. But it can cause severe and even life-threatening complications.
This means that ulcerative colitis is considered a serious illness, and you should treat its management and treatment with a similar seriousness.
Getting the right treatments for ulcerative colitis can cause a dramatic reduction in symptoms and possibly lead to lasting remission.
Additional reporting by Jordan M. Davidson
Don’t Miss: Bland Diet Recipes For Ulcers
Right Or Middle Abdomen Pain
A pain that feels like cramps in the middle of the abdomen or the lower right quadrant is typical of the types of Crohn’s disease known as ileocolitis and ileitis.
Ileocolitis is the most common form of Crohn’s disease and is defined by inflammation located in the last section of the small intestine and in the large intestine .
Ileitis is a type of Crohn’s disease that affects only the ileum and is the second most common form. People with ileitis may also find that their pain or discomfort appears within a few hours of eating a meal.
Colitis And Sacroiliac Pain
What is the relationship between colitis and sacroiliac pain? Doctors have been busy studying the increasing evidence showing a definite link between certain types of sacroiliac joint pain and various lower bowel issues, like irritable bowel syndrome and ulcerative colitis.
There can be many possible reasons for sacroiliac joint pain and most people with SIJ symptoms will not develop colitis. However, scientists have seen enough proof that some sacroiliac symptomology can be an early manifestation of colitis and other autoimmune disorders of the lower bowel.
This short discussion takes a look at what we know about the link between colitis and sacroiliac joint pain. We will explore several scenarios commonly seen by doctors who treat both disorders.
Also Check: How To Check A Horse For Ulcers
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, persons with ulcerative proctitis generally do not have nutrient deficiencies however, other factors may influence an individuals nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, then modifications to the diet will be necessary to compensate for this.
Better overall nutrition provides the body with the means to heal itself. It is important to follow Canadas FoodGuide, but some foods may irritate the rectum and increase symptoms, even though they do not affect the disease course. The customized recommendations of a registered dietitian can address your sensitive digestive tract.
What Is The Makeup Of The Lower Back
To understand numerous reasons for lower back pain, it is important to appreciate the typical style of the cells of this area of the body. Vital frameworks of the lower back that can be related to signs in this region consist of the bony lumbar spinal column , discs between the vertebrae, tendons around the spine and also discs, spinal cord and also nerves, muscles of the lower back, interior body organs of the hips and abdominal area, as well as the skin covering the lumbar location. Ulcerative Colitis And Lower Back Pain
The bony lumbar back is developed to make sure that vertebrae stacked together can offer a movable assistance structure while also protecting the spine from injury. The spinal cord is composed of nervous cells that prolongs down the spinal column from the mind. Ulcerative Colitis And Lower Back Pain
Each vertebra has a spinous process, a bony importance behind the spine, which guards the cords nervous cells from influence injury. Spine also have a strong bony body before the spinal cord to give a platform appropriate for weight bearing of all tissues above the buttocks. The back vertebrae stack right away atop the sacrum bone that is located in between the buttocks.On each side, the sacrum satisfies the iliac bone of the hips to create the sacroiliac joints of the butts.
You May Like: How To Tell Stomach Ulcer
Inflammatory Spinal Disorders Common In Ibd Patients
NEW YORK Ankylosing spondylitis , axial spondyloarthritis and inflammatory back pain are common in inflammatory bowel disease patients two decades after IBD diagnosis, according to findings from the IBSEN study1.
You Might Also Like
Doctors should know IBD patients are at risk of inflammatory back problems, and refer them to a rheumatologist when appropriate, Dr. Alvilde Ossum of Oslo University Hospital in Norway, the studys first author, told Reuters Health in a telephone interview. It can actually damage the back more if you dont get help, she added.
While inflammatory back disorders are known to occur frequently in IBD patients, their prevalence is unclear, Dr. Ossum and her team note in the Journal of Crohns and Colitis, online September 13. To investigate, they looked at 470 patients participating in the Inflammatory Bowel South-Eastern Norway study, including 315 with ulcerative colitis and 156 with Crohns disease.
Twenty years after enrollment, 4.5% of study participants had AS, 7.7% had axial SpA, and 11.5% had inflammatory back pain, according to Assessment of Spondyloarthritis International Society criteria. AS prevalence in the general population is 0.26% in northern Norway and 0.25% in Europe, the researchers note, so the prevalence in IBD patients was 13 to 18 times higher.
Simple Tasks
ACR Convergence
Duration And Evolution Of Pain In Ibd
Pain was a longstanding problem for the majority of the patients with 52% of patients experiencing pain > 5 years. Fifteen patients reported pain since < 1 month, 57 patients suffered from pain since 1 month½ year, 59 patients since ½ year 1 year, 79 patients since 12 years and 215 since 25 years . When comparing CD and UC 388 of the 556 UC patients reported pain in general. Of these the majority reported to suffer from pain more than 5 years. The 679 CD patients on the other hand also reported about pain in 71% of these a majority also suffered from pain > 5 years. When comparing the duration of pain statistically more UC patients only suffered from pain in the last 12 years compared to CD . For the other durations of pain there was no statistical difference .
Also Check: How To Prevent Pressure Ulcers In Wheelchairs
Research And New Developments
Previous research has shown that ankylosing spondylitis has a strong genetic component and were currently funding several research projects to further understand this. Previously, we part funded research that identified a specific gene, called IL23R, thats linked to the condition. Were now funding a follow-on project to investigate how changes in this gene lead to the development of ankylosing spondylitis.
Were also supporting a study thats investigating a gene called RUNX3. Researchers are investigating whether this molecule can be targeted with drugs. Results from this research may lead to the development of new and more effective drug treatments.
Were funding a project investigating the protein HLA-B27. This protein is found in over 90% of people with ankylosing spondylitis. Its thought that HLA-B27 proteins tend to fold incorrectly inside cells, which may lead to the immune system releasing chemicals that cause inflammation. This research aims to generate HLA-B27 specific treatments that overcome the problems associated with current treatment options.
Tylenol And Heat Therapy

Doctors frequently prescribe nonsteroidal anti-inflammatory drugs such as ibuprofen or aspirin to help manage back pain. However, NSAIDs arent typically a viable solution for people with UC, as the medication can cause symptoms to flare.
Those with ulcerative colitis can generally take the pain reliever Tylenol which is not an NSAID for minor aches and pains without side effects. Applying moist heat to affected areas may also reduce pain.
You May Like: How Effective Is Humira For Ulcerative Colitis
What Are The Complications Of Ulcerative Colitis
Colon Cancer
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Skin
Other Complications
What Causes Back Pain In Ulcerative Colitis
- Fatigue
- Weight loss
A person having backaches may not realize its related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
You May Like: Foam Dressing For Pressure Ulcer
Ulcerative Colitis Treatment In Tampa Bay
If you believe that you may be suffering from ulcerative colitis , reach out to the colorectal specialists at the Colorectal Clinic of Tampa Bay. There are many ulcerative colitis treatment options that may suit your lifestyle. Our professional team can help you get your condition under control you may even see remission!
What Causes Uc Cramping
Common causes of UC cramping, according to Ha, are flare-ups, lack of sufficient control of the condition , eating foods that are high in saturated fat or sugar, and adverse reactions to medication.
Cramping due to gas and bloating can also be caused by irritable bowel syndrome , a separate condition from ulcerative colitis that can cause symptoms even when your disease is in remission. IBS can be linked to certain gas-causing foods, including dairy if youre lactose intolerant.
Read Also: How To Treat Skin Ulcer On Leg
Diagnosing Colitis And Chronic Ulcerative Colitis
Your gastroenterologist may suspect colitis based on your medical history and a review of your symptoms. He or she will have you undergo a colonoscopy procedure using a colonoscope to view the colon and rectum, and may take a tissue sample to help determine the cause. Other tests and procedures include:
- BLOOD TESTSBlood tests are taken to determine both red and white blood cell counts. A low red blood cell count can indicate anemia, from bleeding within the colon and rectum. Elevated white blood cells, which fight infection, indicate inflammation within the colon and rectum.
- STOOL SAMPLEA stool sample may be taken to rule out a parasitic infection that can cause colitis.
- CT SCANIn addition to a colonoscopy, a CT scan can determine what areas of the rectum and colon are inflamed.
Classification of chronic ulcerative colitis
Gastroenterologists categorize chronic ulcerative colitis based on the location and extent of inflammation within the colon and rectum. For most patients, the affected area remains the same during the course of the disease.
Finding A Gi Doctor That Listened
Shortly after this I finally had my first appointment with my new GI specialist and it was wonderful because she listened to me. I brought my food journal along with me and described my symptoms in detail, along with my back issues.
She thought it sounded like I was almost reaching remission but that I needed a little push to help me along. Because all my symptoms were restricted to the lower colon, she prescribed me Colocort, a retention steroid enema.
She also thought it was suspicious that I had been having such bad back issues and referred me to a rheumatologist. The Colocort did its job and by the time I saw the rheumatologist, I was feeling great. But then my rheumatologist bluntly laid out the gist of the situation.
Recommended Reading: Best Way To Treat Mouth Ulcers
How Common Is Cramping Among Those Who Have Uc
Inflammatory bowel disease, which includes both UC and Crohns, affects about 1.6 million Americans of all ages, according to the Crohns and Colitis Foundation. More than half of those with UC experience abdominal pain.
The frequency and persistence of cramping can help determine the severity of UC, according to Faten N. Aberra, MD, MSCE, co-director of the Inflammatory Bowel Disease Center at the Joint Penn-CHOP Center and an associate professor of medicine at the Hospital of the University of Pennsylvania, in Philadelphia. Pain that comes and goes with bowel movements may indicate a moderate level of UC. Constant cramping and frequent, bloody stools, on the other hand, may indicate a more serious condition, says Dr. Aberra, such as a dilated colon.
What Makes It Worse
 ALQURUMRESORT.COM” alt=”Ulcerative colitis lower back pain > ALQURUMRESORT.COM”>
ALQURUMRESORT.COM” alt=”Ulcerative colitis lower back pain > ALQURUMRESORT.COM”> The reasons why aren’t totally clear. Doctors don’t know why it affects only a small section in one person, but spreads through the entire colon in another. But certain triggers sometimes play a role. These include:
Food. It’s different for everyone, but certain foods can irritate your symptoms. For example:
- Caffeine can make severe diarrhea worse
- Dairy may lead to more diarrhea, gas, and pain
- Fizzy drinks can be a problem if you have gas
- Greasy and fried foods often lead to gas and diarrhea
- High-fiber foods, such as fresh fruits and veggies, whole grains, corn, nuts, and seeds, can be hard on you
- Spicy foods can be tough to handle
Stress. It can trigger flare-ups and make your symptoms much harder to deal with. It’s especially challenging because just having ulcerative colitis can bring on more of it.
Skipping meds. Even when you’re in remission, it’s very important to take your meds. In the best case, they prevent flare-ups. And even if not, they can help keep things under control.
Follow these 5 tips to help control your ulcerative colitis flare-ups.
Don’t Miss: How Do I Know If I Have A Peptic Ulcer