What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Recommended Reading: How To Heal Colon Ulcers
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Also Check: Peptic Ulcer Food To Eat
What Is Inflammatory Arthritis
IBD-associated inflammatory arthritis is a disease caused by an overactive immune system , rather than physical wear and tear of the joints over time, as is the case with osteoarthritis. Inflammatory arthritis can affect people of all ages, and people living with IBD-associated inflammatory arthritis usually experience joint pain and stiffness after long periods of inactivity, such as in the morning.
A specialized doctor called a rheumatologist should be consulted for the treatment of IBD-associated inflammatory arthritis.
Also Check: What Foods Should I Avoid With A Stomach Ulcer
How Frequent Is Uc Pain
The frequency of the pain due to UC varies. Some people have frequent flares that include pain, while others can have few or no symptoms for years before experiencing discomfort for the first time.
People with frequent flares are much more likely to feel UC pain regularly. Individuals whose flares are more spaced out will have more sporadic pain.
You May Like: Wound Vac For Pressure Ulcers
Pain Management For Ibd Patients
If you are experiencing pain from your disease and have been able to identify the source of the pain, talk to your healthcare provider about what treatments or therapies might work best for you. Different approaches include traditional medications, psychosocial therapies, and complementary therapies.
Five Tips For Dealing With Ulcerative Colitis Pain
There are ways to combat the pain that comes along with ulcerative colitis flare-ups. However, it is always best to get treatment from a doctor as they are most likely to efficiently and safely resolve your symptoms.
Here are five strategies you can use to help relieve symptoms and avoid a flare-up in the first place.
You May Like: How To Lose Weight With Stomach Ulcers
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Knowing The Symptoms Of Ulcerative Colitis
Approximately 750,000 people in the US are living with ulcerative colitis. While relatively less common than other bowel diseases, you probably cant go very long without seeing an ad for medications that are designed to treat symptoms of UC. Perhaps you see these ads and realize that the symptoms they are talking about are ones you experience. Could you have ulcerative colitis? Fortunately, your gastroenterologist will be able to shed light on this issue.
Recommended Reading: Best Supplement For Gastric Ulcers In Horses
Now Adjust Your Energy Flow
Finally, dont be afraid to explore newor, in this casevery old things. Acupuncture, an ancient Chinese practice that uses very thin needles to pierce your skin on strategic parts of the body to adjust or rebalance energy flow , has been shown to both relax you and distract you from pain. And while more research is needed, some studies suggest this traditional Eastern medicinal approach can help ease the inflammation associated with ulcerative colitis. Its definitely worth trying, Dr. Padua maintains, adding that the risk is minimaland the rewards just might be significant.
- About UC: Crohns & Colitis Foundation. What Is Ulcerative Colitis? crohnscolitisfoundation.org/what-is-ulcerative-colitis
- UC and Probiotics: Science Direct. Probiotics for improving quality of life in ulcerative colitis: Exploring the patient perspective. sciencedirect.com/science/article/pii/S2213434418301075
- UC and Anemia: Crohns & Colitis Foundation. Anemia. crohnscolitisfoundation.org/science-and-professionals/emr-search-tool/emr-topics/anemia.html
- UC and Acupuncture:Gastroenterology: Research and Practice. Review of Clinical Studies of the Treatment of Ulcerative Colitis Using Acupuncture and Moxibustion. ncbi.nlm.nih.gov/pmc/articles/PMC5112307/
Warning Signs Of A Flare
Flares often are acute, meaning they come on suddenly. They can last from days to weeks. Between flare-ups, you may experience weeks, months, or years of remission.
Symptoms of a flare may be different depending on the severity and location of the inflammation in the colon and rectum. Nevertheless, common symptoms include:
- Abdominal pain or cramps
- Fever
Read Also: Difference Between Ulcerative Colitis And Crohn’s Disease Ppt
What Are The Causes Of Ulcerative Colitis
It was believed that our diet and too much stress results in UC, but now it is understood that they only aggravate the condition and not cause it. The exact cause is still not known. Doctors now think that when our immune system fights off infection, it also attacks the normal cells in the gastrointestinal tract causing UC. It has also been seen that genetics and family history all seem to play a role.
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
Recommended Reading: How Can Ulcers Be Treated
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
Ulcerative proctitis has very few complications but with increased irritation to the anal and rectal area, hemorrhoids may occur. Only rarely do other complications occur, such as abscesses and extra-intestinal manifestations. Individuals with ulcerative proctitis are not at any greater risk for developing colorectal cancer than those without the disease.
Recommended Reading: Best Anti Diarrhea Medicine For Ulcerative Colitis
How To Manage Ulcerative Colitis Pain
Learning effective pain management strategies is a crucial aspect of living well with ulcerative colitis , a form of inflammatory bowel disease . Flare-ups can happen, even if you carefully manage your condition. Swelling of the intestine may cause bloating and painful cramping. You may experience bleeding due to skin irritation from persistent diarrhea.
During a flare-up, it’s not unusual to feel unwell all over. Fatigue, nausea, fever, and anxiety are common symptoms with UC. Progression of the disease can produce joint pain, skin rashes, mouth sores, and even make your eyes hurt.
UC pain can significantly impact quality of life. One MyCrohnsAndColitisTeam member wrote, Pain in my gut . So tired of being in pain. Another member posted, Woke up with the worst back pain I could ever imagine. I was in tears.
Fortunately, it’s possible to manage the pain associated with UC using a combination of at-home remedies, medical interventions, lifestyle changes, and alternative treatments.
Tylenol And Heat Therapy
Doctors frequently prescribe nonsteroidal anti-inflammatory drugs such as ibuprofen or aspirin to help manage back pain. However, NSAIDs arent typically a viable solution for people with UC, as the medication can cause symptoms to flare.
Those with ulcerative colitis can generally take the pain reliever Tylenol which is not an NSAID for minor aches and pains without side effects. Applying moist heat to affected areas may also reduce pain.
Recommended Reading: What Causes Acute Ulcerative Colitis
How To Treat Ulcerative Colitis
The treatment of Ulcerative Colitis also depends upon the severity of the patient. The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis.
Following drugs may calm down the inflammation and make the patient feel better.
Vitamin And Mineral Supplements

People with IBD often have vitamin or mineral deficiencies because digestive dysfunction prevents the body from absorbing important nutrients. These include iron, folate, vitamin D, and vitamin B12. As part of treatment at NYU Langone’s Inflammatory Bowel Disease Center, nutritionists may recommend dietary changes. They may also advise supplementing your diet with vitamins and minerals to boost your digestive health.
Recommended Reading: What To Eat During An Ulcerative Colitis Flare
The Link Between Ulcerative Colitis And Joint Pain
UC is a type of inflammatory bowel disease . Arthritis is the most common non-GI complication of IBD. The reason for the link may lie in genes that make people with IBD more susceptible to arthritis.
Two types of conditions can affect the joints of people with UC. Arthritis is joint pain with inflammation . Arthralgia is pain in the joints without any inflammation.
Arthritis that occurs with UC is a bit different than regular arthritis. For one thing, it typically starts at a younger age.
In addition, arthritis in people with UC doesnt usually cause long-term joint damage. The joints swell up and become painful, but they return to normal once intestinal inflammation is under control.
A few types of arthritis can affect people with UC:
Can Ulcerative Colitis Lead To Cancer
If you have widespread ulcerative colitis, your risk of developing colon cancer is higher than people who do not have ulcerative colitis. This is particularly true if you have had colitis for many years.
Your doctor will probably advise you to have regular examination by colonoscopy. Biopsies will probably be taken at the colonoscopy for microscopic examination to detect any changes in bowel tissue that might lead to cancer. Your doctor will advise you on how often you should have these examinations depending on how long you have had ulcerative colitis.
Read Also: What Should You Eat When You Have Ulcerative Colitis
Signs Of Possible Colitis
General signs of colitis can include:
- Intense pain
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
Proctocolectomy With Ileoanal Anastomosis
Alternatively, you may be able to have a different kind of operation that eliminates the need to use a bag altogether. A pouch is constructed from the end of the ileum and then attached directly to the anus, allowing you to expel your waste normally. However, this type of operation, which may be carried out in one or 2 stages, can result in frequent bowel movements in the long term.
Although the decision to have surgery will have to be carefully considered by you and your doctors, it does mean your condition should no longer be a problem.
Recommended Reading: Ulcer In My Stomach Symptoms
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Faqs About Ulcerative Colitis
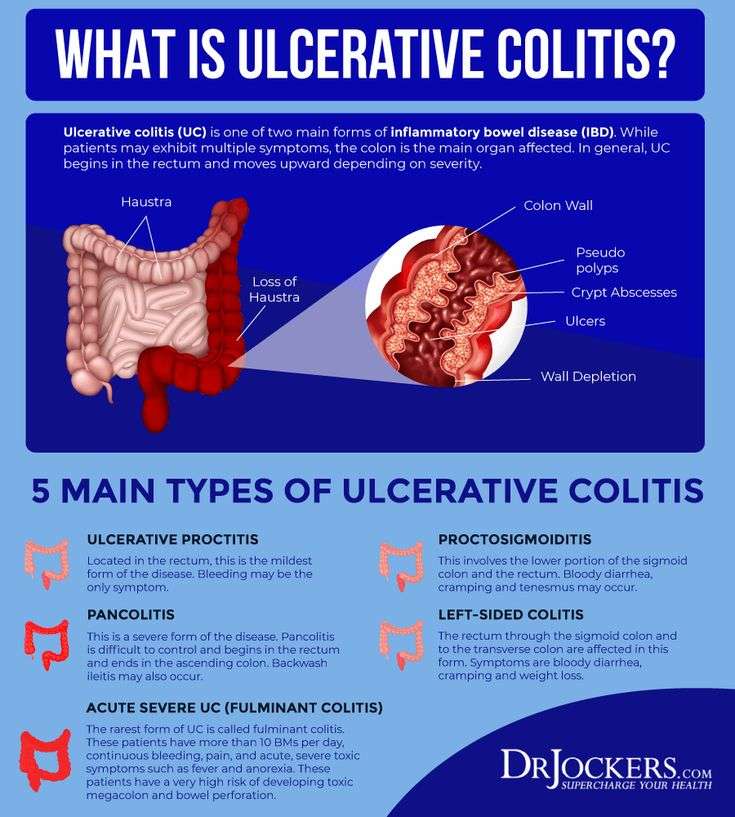
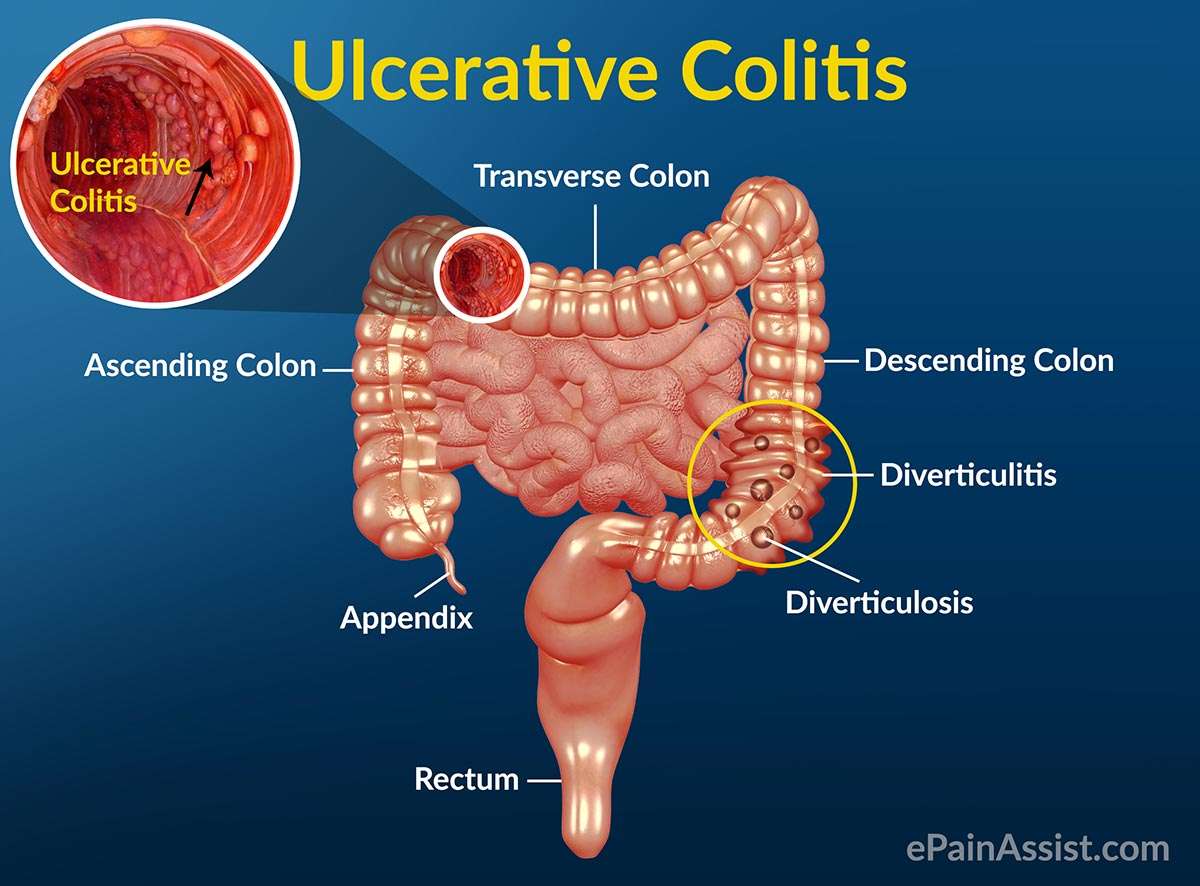
What is ulcerative colitis?
Ulcerative colitis is an inflammatory bowel disease of unknown cause in which the gastrointestinal tract is unable to distinguish foreign from self-antigens. It is characterized by chronic inflammation of the colonic mucosa and submucosa, atrophy and possibly dysplasia limited to the colon. The extent of disease varies and may involve only the rectum , the left side of the colon to the splenic flexure or the entire colon .
What causes ulcerative colitis?
Hereditary factors seem to play a role in the etiology of ulcerative colitis. The most significant risk factor for the development of ulcerative colitis is a family history. Environmental factors are also involved, as evidenced by higher rates of this disease in urban locales.
What are the symptoms of ulcerative colitis?
The most common symptom of ulcerative colitis is diarrhea that is often bloody. Other symptoms include abdominal and/or rectal pain, fever and weight loss. Some patients complain of constipation and rectal spasm. Arthritis symptoms may occur in as many as 26 percent of patients with ulcerative colitis, dermatological changes in fewer patients and ocular manifestations in about 5 percent.
How is ulcerative colitis diagnosed?
Who is affected by ulcerative colitis?
Is there a relationship between smoking cigarettes and developing UC?
What is the treatment for ulcerative colitis?
Will I eventually need to have surgery for ulcerative colitis?
What is pouchitis?
Don’t Miss: Mouth Ulcer On Tongue Causes
Avoid Foods That May Exacerbate Uc Symptoms
Because a healthy diet is a cornerstone for overall health, its no surprise that it tops Sniders list of natural remedies for ulcerative colitis. Diet is a foundational treatment for patients with ulcerative colitis, he says, adding that there’s often a dietary component to the disease.
According to a review published in October 2014 in Clinical Gastroenterology and Hepatology, people who reported a diet high in fats were more likely to have a relapse of UC. Other studies highlighted in the paper suggested avoiding greasy foods, dairy products, caffeine, and raw fruits and vegetables if you have ulcerative colitis. But the review notes that theres no one-size-fits-all diet for UC, so youll have to figure out what works best for you through trial and error.
It helps to keep a food diary to discover which foods are best for you. Snider says it can’t hurt to limit certain foods, and then if your symptoms improve according to your symptom diary, to continue doing so. He also notes that it’s worthwhile to avoid sugar because its effect on the pancreas hinders the output of anti-inflammatory enzymes.