How Long Does It Take To Recover From The Surgery For Ulcerative Colitis
The hospital stay after the surgery is usually 3 to 7 days. During this period, the surgeon will monitor the surgical wound and watch for complications, if any. The patient will be advised to follow a specific diet and will be advised how to take care of the surgical wound or the stoma and the stool bag, if any.
The recovery period for the surgical procedures will generally be 4 to 6 weeks. During this period, the patient will have regular follow-ups with the doctor.
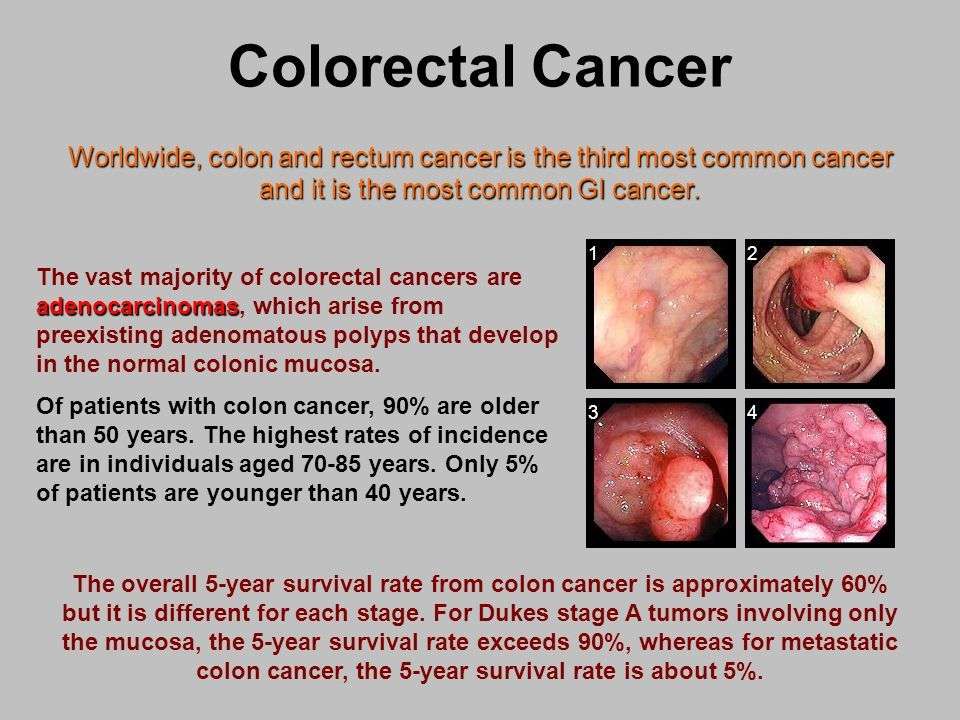
Colon Cancer And Ulcerative Colitis
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you don’t get treatment for UC. That’s because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if you’ve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesn’t go away.
- You’re a man.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member who’s had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think it’s because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Recommended Reading: How Do You Check For A Stomach Ulcer
Not Everyone Will Understand The Intensity Of Your Disease
Although ulcerative colitis can affect many aspects of your physical health, its often considered an invisible illness. Depending on the severity of symptoms on a given day, people with the condition can often still move around without any obvious signs that theyre in pain or discomfort. It puts a lot of pressure on your shoulders when you are chronically ill and it’s not visible, because you have to explain yourself time and time again, Skomski says. And since people between the ages of 15 and 30 are one of the more at-risk age groups for developing ulcerative colitis, people with the condition are sometimes perceived as too young to be sick.
People may also have a hard time wrapping their head around the pretty major lifestyle adjustments you might have to make with ulcerative colitis. My lifestyle’s not like a typical 20-something, Sam says. I think a lot of my friends see this as the intense period of their life: staying up all night, going to concerts that go until the middle of the night, going to bars, things like that. And I just can’t.
Medications For Ulcerative Colitis
The goal of medication is to control inflammation and heal the intestinal lining known as mucosal healing.
Medications used to treat ulcerative colitis include:
- Aminosalicylates, such as sulfasalazine and mesalamine , which reduce inflammation
- Antibiotics to treat bacterial infections
- Antidiarrheals to control diarrhea
- Biologic agents that can rapidly induce remission in patients with severe ulcerative colitis, defined as more than six bloody stool episodes daily
- Corticosteroids
- Immunomodulators that suppress the bodys immune response, such as azathioprine and 6-mercaptopurine
After beginning medication therapy, follow-up blood and stool tests for markers of disease activity, such as fecal calprotectin can help monitor the response to various therapies.
You May Like: Artificial Sweeteners And Ulcerative Colitis
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
What Are Complications Of Ulcerative Colitis
Your risk for UC complications is higher the more severe the disease. If symptoms are neglected, life-threatening complications can occur, including:
- Anemia: Anemia occurs when the body has fewer red blood cells than normal, which can happen if stools are frequently bloody. Long-term anemia with a severe dip in hemoglobin can cause stress to the heart leading to heart failure.
- Bone problems: Problems with vitamin D and calcium absorption due to gut swelling can cause bones to become brittle. This increases the risks of joint problems and even fractures.
- Perforation: Untreated intestinal swelling in severe cases of ulcerative colitis may cause a tear or a hole in the wall of the large intestine. This can be life-threatening.
- Shock: Passing a lot of blood from the rectum can cause low blood pressure and even shock.
- Toxic megacolon: Extreme intestinal swelling can prevent regular intestinal movements, leading to paralysis of the intestine. This condition is potentially fatal.
Because this is a long-term disease with potential complications, its important to maintain regular follow-ups with your doctor.
Also Check: Mouth Ulcer On Tongue Causes
Complications Of Ulcerative Colitis
Although people with ulcerative colitis commonly have minor liver dysfunction, only about 1 to 3% have symptoms of liver disease, which vary from mild to severe. Severe liver disease can include inflammation of the liver , inflammation of the bile ducts , which narrow and eventually close, and replacement of functional liver tissue with scar tissue . Inflammation of the bile ducts may appear many years before any intestinal symptoms of ulcerative colitis. The inflammation greatly increases the risk of cancer of the bile ducts and also seems to be associated with a sharp increase in the risk of colon cancer.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Recommended Reading: Is Sweet Potato Good For Ulcerative Colitis
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
What Are The Different Classifications Of Ulcerative Colitis
Doctors often grade UC based on symptoms and blood work results, classifying the disease as mild, moderate or severe.
Table: Classification of ulcerative colitis
| Signs/Tests | ||
|---|---|---|
|
|
|
|
||
| Blood tests |
|
|
| 72% of patients have mild disease | 27% of patients have moderate disease | 1% of patients have severe disease at presentation |
Don’t Miss: Will Ulcers Cause Blood In Stool
How Do I Ensure A Long Life Expectancy Living With Ibd
If you suffer from Crohn’s disease or colitis, then you need to be proactive with your health and nutrition to ensure your life expectancy is not affected. Here are the top 4 things that recommend ensuring you have a long-life expectancy.
- Regular Doctor Visits
- Regular Cancer Screenings and Colonoscopies
- Proper Supplement and Medication Intake
What Are The Signs And Symptoms Of Colon Cancer Vs Ulcerative Colitis
Colon Cancer Symptoms and Signs
Some individuals with colon cancer have no symptoms, and if they do have symptoms they often are minimalized and overlooked until the cancer becomes more severe. Cancer screening tests for colon cancer thus are important in individuals 50 years of age and older. Colon and rectum cancer can have many different symptoms and signs. If you have any of these symptoms, seek immediate medical help. You may notice bleeding from your rectum or blood mixed with your stool. It usually, but not always, can be detected through a fecal occult blood test, in which samples of stool are submitted to a lab for detection of blood.
People commonly attribute all rectal bleeding to hemorrhoids, thus preventing early diagnosis owing to lack of concern over “bleeding hemorrhoids.” New onset of bright red blood in the stool always deserves an evaluation. Blood in the stool may be less evident, and is sometimes invisible, or causes a black or tarry stool.
Rectal bleeding due to colon cancer may not be noticeable or chronic, and may only show up as an iron deficiency anemia, not colon cancer. Colon cancer may be associated with fatigue and pale skin due to the anemia. Changes in bowel movement frequency also is a symptom of colon cancer.
If the tumor in the colon becomes large enough, it may completely or partially block your colon. Symptoms of bowel obstruction include:
Ulcerative Colitis Symptoms and Signs
Common symptoms of ulcerative colitis include:
Also Check: Topical Treatment For Decubitus Ulcer
How Does Ulcerative Colitis Progress
Ulcerative colitis is a chronic, relapsing condition. Chronic means that it is persistent and ongoing. Relapsing means that there are times when symptoms flare up and times when there are few or no symptoms . The severity of symptoms and how frequently they occur vary from person to person. The first flare-up of symptoms is often the worst.
It starts in the rectum in most cases. This causes a proctitis, which means inflammation of the rectum. In some cases it only affects the rectum and the colon is not affected. In others, the disease spreads up to affect some, or all, of the colon. Between flare-ups the inflamed areas of colon and rectum heal and symptoms go away. The severity of a flare-up can be classed as mild, moderate or severe:
- Mild – you have fewer than four stools daily and only have small amounts of blood in your stools. You do not feel generally unwell .
- Moderate – you have four to six stools a day, have some blood in your stools but do not feel generally unwell in yourself .
- Severe – you have more than six stools a day and have blood in your stools. You also feel generally unwell with more marked systemic disturbance with things such as high temperature , a fast pulse rate, anaemia, etc.
How Long Does An Ulcerative Colitis Flare
Ulcerative colitis is a chronic disease that causes inflammation and ulcers in the inner lining of the large intestine and rectum. If you have UC, you may experience repeated cycles of flare-ups and remissions .
A flare-up can last a few days or a few weeks and then be followed by a remission that lasts for months or even years. How long a flare-up lasts depends on factors such as:
While there is no cure for UC, several treatment options and lifestyle modifications can help reduce symptoms or prevent flare-ups.
Read Also: Vitamin E And Ulcerative Colitis
How Ibd Is Managed
IBD can be managed through multiple approaches, most likely including medication and lifestyle changes such as diet, exercise and stress management.
Ampersand Healths My IBD Care app is a great tool for those looking to self-manage their condition. The app offers tracking tools , expert-led courses, and a library of resources that are readily available for users to explore. For those who have a hospital signed up to the app, their clinical team is able to monitor tracking and activity on the app so that they can provide their patients with better care.
Does Ibd Effect Life Expectancy
This is a very complex question, and we will refer to scientific studies to help us answer it for you. Unfortunately, it is almost impossible to calculate life expectancy, but there have been studies on Crohn’s disease and ulcerative colitis whose goal was to find any noticeable patterns in life expectancy.
According to the National Library of Medicine, life expectancy for people with IBD increased from 1996 to 2011, but the study concludes that people who suffer from IBD do have a lower life expectancy than people without IBD.
Improved management of IBD symptoms and pain associated with these symptoms will continue to improve health-adjusted life expectancy for people with IBD.
Healthline suggests that IBD should not drastically affect life expectancy if you are taking care of your body, visiting the doctor regularly, and following proper dietary guidelines such as the Low FODMAP diet.
The Crohn’s and Colitis foundation says that life expectancy can be shortened due to the increased risk of colon cancer. They suggest that patients that suffer from Crohn’s disease and ulcerative colitis should have regular colon screenings as they are at higher risk of developing colon cancer than the general population.
WebMD says that people who suffer from Crohn’s disease and ulcerative colitis should have a similar life expectancy to someone without IBD if they are taking preventative measures and ensuring that no complications arise.
Also Check: What To Take For Mouth Ulcers
Can I Live A Normal Life With Ulcerative Colitis
Even during times of remission, it is important to continue taking medications and seeing your doctor regularly. Studies show that people with UC usually have the same life expectancy as people without UC. It is important to remember that most people who have ulcerative colitis lead full, happy, and productive lives.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
You May Like: Pressure Ulcer Care At Home
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Ulcerative Colitis: Prognosis And Life Expectancy
Ulcerative colitis is a chronic that can be mild, moderate or severe. Its impossible to predict how the disease will affect an individual because lifestyle, access to medical care, and overall health status all affect the progression of this common condition. With appropriate treatment, most people with ulcerative colitis will experience symptom-free periods of remission and periodic symptom flares.
There is no cure for ulcerative colitis, but many people with ulcerative colitis live satisfying lives.
Don’t Miss: Succeed For Horses With Ulcers