Diet Management In Ulcerative Colitis
Its important to pay attention to what you eat if you have ulcerative colitis . Foods do not drive the condition, although they can induce flare-ups.
How can you avoid those triggers while still getting the nutrition you require? A nutrition plan can be beneficial in this situation. Here we discuss diet in Ulcerative Colitis, including what foods to eat and what foods to avoid.
Ulcerative Colitis Diet: Advice From A Dietitian
If you have ulcerative colitis, knowing what to eat can be tricky. Its important to customize your food choices based on your current tolerance and health goals. This post will help you understand the current scientific thinking on ulcerative colitis and diet and how to move forward with the approach that is right for you.
We have been working with clients with Crohns disease and ulcerative colitis in our practice for over seven years its an area I am passionate about because of the massive toll these diseases take on peoples quality of life. I also believe that nutrition can play a much larger role in the management of the diseases than is often discussed in the doctors office.
As a dietitian, I believe that the goal of nutrition is more than just ensuring you get all the vitamin D you need. I believe and have seen firsthand in my practice that creating a strong individualized approach to nutrition can help people find healing and learn how to thrive, no matter their diagnosis. Which is why it is frustrating that much of the scientific literature on ulcerative colitis is focused on either associating the risk of disease with certain foods, or acute strategies for securing remission in a flare.
Cooked And Peeled Vegetables
Many vegetables are high in fiber, but as with fruit, peeling them removes a layer of insoluble fiber.
Some vegetables do not need peeling, such as asparagus tips and mushrooms, but it can help to remove the skins of potatoes, carrots, and squash.
Cooking vegetables also makes them easier to digest, and it can reduce the fiber contents.
However, avoid roasting or frying vegetables in oil or butter, because fats can irritate the digestive system and worsen symptoms of Crohns. Try boiling or steaming them instead.
You May Like: How To Prevent Diabetic Ulcers
Back Up: What Is Ulcerative Colitis Exactly
Ulcerative colitis is a type of inflammatory bowel disease that causes ulcers and sores in the lower quarter to third of your digestive tract. Typically, these ulcers are found in your rectum or in the inner lining of your lower intestine . This can cause bloody diarrhea, the most common symptom of ulcerative colitis, but you might also experience things like abdominal cramping, constipation, and a general sense of fatigue. Weight loss and a loss of appetite can also crop up, per the U.S. National Library of Medicine.
Diana Whitehead, M.D., director of the Inflammatory Bowel Disease Center at the Greater Baltimore Medical Center, explains that though ulcerative colitis has a strong genetic component, symptoms are often set off by a triggering event that activates inflammation in the lower intestine. Basically, your immune system is not doing what it should do, which is to protect you, but its gone kind of into overdrive, Dr. Whitehead says. In other words, even though the exact causes of ulcerative colitis arent fully understood, experts consider it to be an autoimmune condition thats set off by this overreaction in the gut.
Scd And Low Fodmap Diet For Ulcerative Colitis
There is a lot of interest but limited clinical evidence for the use of the specific carbohydrate diet and low FODMAP diet for ulcerative colitis.
In one trial, a low FODMAP diet did appear to improve quality of life and symptoms of ulcerative colitis, without improving fecal calprotectin or C-reactive protein, two markers of inflammation. If you are experiencing a lot of IBS-like symptoms, it may be a temporary option to help get symptoms under control.
I have also used low FODMAP foods as a lower fermentation framework for increasing fruit and vegetable intake for those who are currently eating a low fiber diet. I worry about the adoption of a long-term low FODMAP diet in ulcerative colitis as I believe that it might be simply tamping down symptoms by further altering the gut microbiomewhich could be detrimental for long term gut health.
The specific carbohydrate diet is based on a decades-old book called Breaking the Vicious Cycle. To my mind, it is similar to a low FODMAP approach in that it alters the types of carbohydrates available for fermentation in the gut.
It is not uncommon for those who have UC to feel that an SCD diet is helping if that is the case, we will support our client on that chosen path however, I dont believe it is a solution for long term gut health and wont advocate for it in practice. It is a complex diet to follow and isnt supported by the evidence.
Don’t Miss: Bland Diet Recipes For Ulcers
Other Weight Loss Tips
Other strategies that may help someone lose weight include:
- Cutting down on alcohol: Drinking alcohol can cause a person to experience symptoms of UC and gain weight. People who drink alcohol may find that reducing their intake is an easy way to cut down the number of calories they consume.
- Reducing plate size: People can reduce their portion sizes by replacing their dinner plate with a side plate. A small plate gives the illusion of a full plate while decreasing the portion size.
- Taking steps to improve sleep hygiene: Getting enough sleep can help a person lose weight.
Foods Rich In Sulfur And Sulfites
Foods like beer, wine, shellfish, some dried fruits, white bread, and cured meats containsulfur, producing excess gas in the colon. Even without these foods, UC patients produce more hydrogen sulfide than usual, and they have difficulty breaking the gas down due to inflammation of the colonic wall. Hence, ingesting more foods with sulfur causes more damage to the colon.
Don’t Miss: What Does Asacol Do For Ulcerative Colitis
Lifestyle Diet In Inflammatory Bowel Disease
Inflammatory bowel disease , which consists of Crohns disease and ulcerative colitis, can be a frustrating diagnosis to deal with. In general, there is no clear evidence that one trigger alone causes problems. Therefore, there is no particular food, diet or lifestyle that causes, prevents or cures IBD.
Some patients are more fortunate and can control their IBD through medication. Other patients experience flare-ups, meaning the lining of the intestine is inflamed and the absorption of nutrients in the body is disturbed. Identifying the cause of this disturbance takes time, patience and some homework.
Keeping a food diary is a great way to manage flare-ups. Start with a low-fiber or liquid diet until the situation is resolved, and realize certain foods may make symptoms worse.
In general, IBD patients should follow a healthy diet keeping these tips in mind:
- Eat smaller, more frequent meals.
- Enjoy food in a relaxed atmosphere.
- Avoid identified trigger foods.
- Limit foods such as seeds, nuts, beans, fruit and bran.
- Drink plenty of good fluids such as water, low-sugar sports drinks and diluted fruit juice.
- Stay away from caffeine and energy drinks.
- Use the choosemyplate.gov website as a guideline.
Besides eating a recommended diet, there may still be some supplements suggested for patients with IBD. Talk to your health care provider about assistance from calcium, vitamin D, folic acid, vitamin B12, iron, zinc and probiotics .
Topics in this Post
Diet Recommendations For Crohn’s Disease Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
Also Check: How Do You Get Rid Of Stomach Ulcers
It Can Be Challenging To Differentiate Between Crohns And Uc
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
You May Like: What Over The Counter Medicine For Ulcers
Tips For Managing Ulcerative Colitis Symptoms
- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods boil, steam, grill, poach, broil or saute
Recommended Reading: What To Drink With Stomach Ulcer
Recommended Reading: Corneal Ulcer Dog Home Remedy
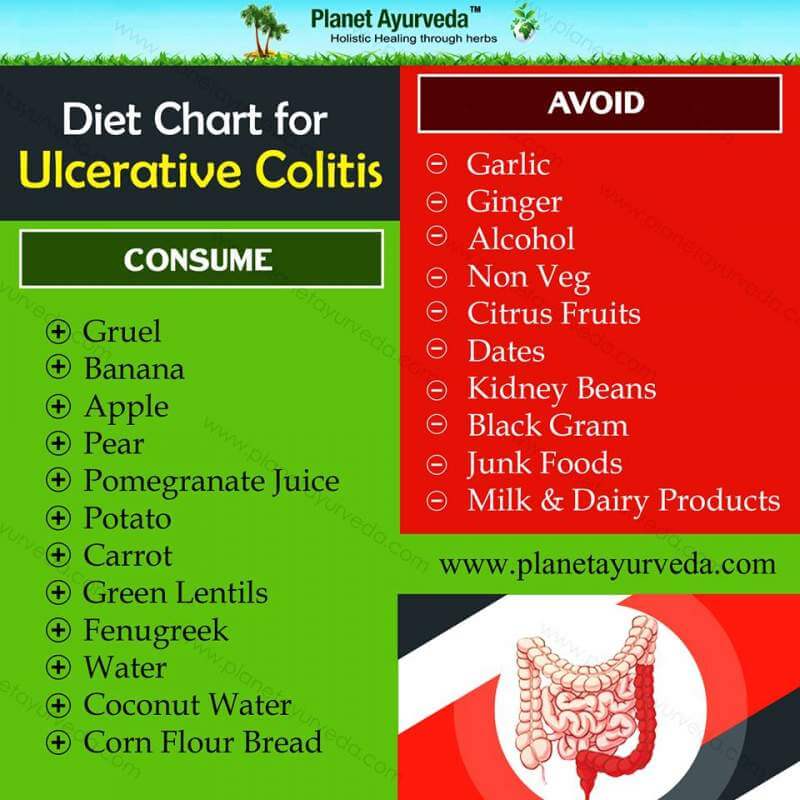
Foods To Avoid With Ulcerative Colitis
- Added sugars and hyper-processed foods
Our North American love affair with low fibre, high sugar and high fat hyper-processed food is associated with our risk of ulcerative colitis. It is this type of eating that is thought to drive gut dysbiosis or the overgrowth of more pro-inflammatory gut bacteria that can harm gut barrier integrity leading to leaky gut and inflammation. In laboratory studies, this type of diet can decrease the number or acetate and butyrate producing bacteria and increase the risk of colitis.
Another issue with hyper-processed foods is that they contain emulsifiers like xanthan gum and carrageenan which may alter gut barrier integrity. While their true impact on gut health is still hotly debated, in one double-blinded trial, people with ulcerative colitis on a carrageenan free diet had lower relapse rates than those given two capsules of carrageenan. For me, this would not be the first place I look when adjusting someones diet instead, it would be a refinement only after taking more global steps towards a more whole foods, plant-based approach.
- Meat, particularly red meat
If you arent a huge fan of red meat, ditch it entirely. If you truly love red meat, try to limit yourself to one 3-4 ounce portion every week or two, no more.
- Dairy
Dairy could be impacting symptoms for a few reasons:
- Omega 6-rich cooking oils like soy, corn and safflower oils
Choosing The Right Diet For Ulcerative Colitis
Because each body is different, there isnt a one-size-fits-all diet for UC. Work closely with a registered dietitian to design a diet that works for you, Diekman advises. Its also good to keep track of what you eat in a food journal. This makes it easier to pinpoint which ingredients trigger your symptoms.
Additional reporting by Kaitlin Sullivan
Don’t Miss: Is Ulcerative Colitis Considered An Autoimmune Disease
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
You May Like: Foods That Cure Ulcerative Colitis
How Can I Track Foods That Cause Flare
The Crohns and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohns and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Don’t Miss: What Is A Decubitus Ulcer Why Does It Occur
Ulcerative Colitis Treatment Medications
Treatments for ulcerative colitis includes both medications and surgery however, there is no medication that can cure ulcerative colitis. Medicationsthat treat ulcerative colitis are
- anti-inflammatory agents, for example, 5-ASA compounds like sulfasalazine , and olsalazine , and topical and systemic corticosteroids), and
- immunomodulators, for example, 6-mercaptopurine , azathioprine , methotrexate , cyclosporine .
Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohns disease.
Can You Eat Pizza With Ulcerative Colitis
There are many tasty foods that provide good nutrition and may not irritate your digestive tract. If you can tolerate dairy products, ice cream or milk shakes made with ice cream or yogurt are a good choice. Pizza or a cheeseburger may be a good choice.
Also Check: Interprofessional Care For Ulcerative Colitis
What Side Effects Of Ibd Can Cause Malnutrition
There are several reasons why people with IBD may be at risk for malnutrition. The following list includes some side effects that contribute to malnutrition.
- Inadequate food/fluid intake may by caused by nausea, abdominal pain, loss of appetite or altered taste sensation
- Increased losses â intestinal inflammation during acute flares results in increased protein losses, losses from fistula fluids, diarrhea and bleeding
- Increased nutritional needs â inflammation or infection increases metabolic requirements
- Malabsorption with Crohns disease may be caused by severe intestinal inflammation, resection of small intestine and medications, such as prednisone and sulfasalazine
What Is Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that affects that affects the colon, or large intestine. Typically, the inflammation starts in the rectum and then extends continuously throughout the colon. It is commonly diagnosed in your thirties, and takes a flare and remission pattern where sometimes you feel okay and other times you dont.
You May Like: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
Fructose & High Fructose Corn Syrup
Ascientific study that examined the effect of fructose among people with ulcerative colitis concluded that high amounts of fructose causes can be inflammatory in UC. Fructose can be found in several foods, including corn syrup, honey, fruit juice, and molasses. Fructose also depletes the layer of mucus lining the colonic wall, exposing it to bacteria that eat up the colonic lining. That results in inflammation.
Nutritious Foods To Combat Ulcerative Colitis Complications
People with ulcerative colitis commonly experience anemia and unintended weight loss. Anemia is a low red blood cell count caused by chronic blood loss. It can cause fatigue unless treated. For this reason, the nutrients folate, magnesium, calcium, and iron are of special importance for individuals with UC.
Furthermore, steroid medications such as prednisone may contribute to risk of osteoporosis, which puts emphasis on dietary intake of calcium, vitamin D, magnesium, and vitamin K. Here are the vital body functions that depend on each of these nutrients, along with food sources rich in each.
Calcium
Calcium is important for healthy bones, teeth, and the heart. The best food sources include dairy products, such as yogurt, milk, cottage cheese, and more. Nondairy sources of calcium include sardines , fortified soy milk and almond milk, tofu, kale, broccoli, and chia seeds.
Folate
Folate is crucial for cell division and DNA synthesis. It is found in avocados, black-eyed peas, spinach, Brussels sprouts, asparagus, and fortified breakfast cereals.
Iron
Iron is an important mineral that helps transport oxygen in red blood cells from the lungs to body tissues. It is found in fortified breakfast cereals, tofu, spinach, lentils, chickpeas, and cashews.
Magnesium
Magnesium is an important electrolyte that may be lost through sweating or diarrhea. Foods such as halibut, nuts, nut butters, spinach, potatoes with skin, black-eyed peas, and spinach are rich in magnesium.
Vitamin D
Don’t Miss: Horse Stomach Ulcers Natural Remedies
What Foods Should You Eat With Ulcerative Colitis
If you have Ulcerative Colitis, very minor changes to what you eat can make a BIG difference in your symptoms. Consider keeping food logs or adjusting foods that trigger your symptoms. You may also want to work with your doctor or dietitian to work through an elimination diet. Generally, you should try to:
In terms of specific food recommendations, go with these:
| Food Type |
|---|