What Is Dietary Fiber
Dietary fibers are non-digestible carbohydrates found in plants. Humans cant break down fiber so it travels throughout the gastrointestinal tract and exits more or less the same way it came in. Thats why we see corn in the toilet.
All fibers are not the same. There are different types with varying characteristics. Health organizations have tried to define them, but the definitions are imperfect and inconsistent.
More often than not, youll hear fiber described as insoluble or soluble.
Soluble fiber is more fully fermented in the large intestine and has a higher gel-forming capacity than insoluble fibers. Humans cant digest fiber, but microbes can. When a fiber is fermentable, that means bacteria can metabolize it in the colon. These are prebiotic fibers. When a fiber has a higher gel-forming capacity, that means its viscous. Soluble fiber is more fermentable and viscous than insoluble fiber, although certain insoluble fibers are fermentable.
I like to refer to insoluble fiber as roughage because of its coarse nature. Roughage has a mechanically irritating effect on the large intestine, triggering water and mucus secretion.
Think of an apple. The inside of the apple is the soluble fiber, whereas the apple skin is the roughage. This illustration applies to most fruits and vegetables. Their insides are soft and soluble whereas the skins and stalks are roughage.
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
Ulcerative Colitis Diet According To An Rd
Some periods of your life, you almost forget you have ulcerative colitis. You get a glimpse into what normal life is like, without the painful symptoms and constant concern of how soon youll reach bathroom. Taking in the time you have without those feverish symptoms and relentless inflammation. Although ulcerative colitis can feel like an uncontrollable cascade of compromising complaints, there are a few things you can do to keep your symptoms at bay one of the most highly recommended and suggested being your diet.
Recommended Reading: Support Surfaces For Pressure Ulcer Prevention
Treating Treats As Treats
Avoid sweet fruit juices, sodas, or other drinks made with sugar and rather drink water, decaf tea, and hydrating drinks like coconut water. Avoid sugarless or sugar-free products because many times they have sugar alcohols, which lead to uncomfortable gas symptoms. Limit or avoid alcohol which is both irritating and dehydrating.
Evidence From Intervention Studies
Dietary interventions to reduce relapse and disease activity in IBD patients have used different strategies/targets including promotion of favorable gut microbiota, decrease in intestinal permeability and intestinal epithelial injury, and reduction of inflammation. Dietary interventions tested for their efficacy against IBD include specific carbohydrate diet, low-FODMAP diet, gluten-free diet, antiinflammatory diet, immunoglobulin-G4-guided exclusion diet, high-fiber diet, low-residue diet, semivegetarian diet, Mediterranean diet, and paleolithic diet. Dietary supplements investigated for benefits in IBD patients are curcumin, glutamine, n-3 fatty acids, vitamin D, prebiotics, and probiotics. The effects of these dietary interventions and nutrition supplementations on pathogenesis and treatment of IBD have been reviewed in several recent articles.183,188â190
Recommended Reading: Food To Avoid For Ulcer Patient
What To Eat During A Flare
All of the diets above are intended to be temporary and followed during a flare-up. Working with a dietitian can help prevent deficiencies in certain micronutrients, which is common with IBD.
During a flare its helpful to eat four to six small meals per day rather than fewer larger meals. Its also very important to drink fluids because diarrhea can occur with a flare and cause dehydration.
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!
Tom
Also Check: Can Ulcerative Colitis Cause Cancer
Dairy Intake As Risk Factor For Ibd
The European Investigation into Cancer and Nutrition study found that individuals that consumed milk had significantly reduced odds of developing CD , suggesting a protective effect with dairy product consumption . Individual dairy products consisted of milk, yogurt, and cheese with varying fat content . This is supported by a case-control study in children that demonstrated that consumption of dairy products was not associated with CD . Overall, the consumption of dairy products is not a risk factor for IBD.
Supplement Your Diet If Its Not Right
Work with your physician or dietitian to get enough vitamins and minerals through food, first. If you are not able to get enough through the food youre eating, consider taking a high-quality supplement. Beware of clever marketing scams and educate yourself on what to look for when choosing a supplement.
You May Like: How To Heal Mouth Ulcers Fast
Why Someone May Need A Low
As stated above, the intent behind a low-residue diet is to give the bowels and colon time to rest or become less inflamed. So, by and large, the ideal candidate for someone who may need a low-residue diet is someone who is having digestive issues. While many think low-residue diets are only for individuals that have just received bowel surgery, individuals that need colonoscopies, and individuals with IBD, low-residue diets can also be a treatment option for individuals with GERD symptoms. The foods to avoid with GERD are consistent with the foods encouraged and discouraged with a low-residue diet.
Special diets are recommended as initial efforts for mitigating digestive issues prior to using traditional medical approaches. So those who can benefit from low-residue diets vary tremendously from patients going through chemo to individuals that simply eat too much fiber in their diet.
Low Residue Foods And Ingredients
Part 2 of this series will be a list of foods that will help you write your grocery lists and may even be worth sharing with immediate family and friends, so when they ask how they can help, they will know which foods, in particular, to avoid serving you or including in your dish. The internet is a great tool and resource for finding substitutes, my friends. Use it to your advantage!
It’s also gathering crops & gardening season, so this is a great time to have a refresher on what types of foods we might be consuming more in the summer months after we harvest or take a stroll down to the Farmer’s Markets in our areas.
So let’s break it down:
Read Also: How Do They Check For Ulcers
A Satisfying Nicoise Salad
If you hear salad and think, I wish, this Lettuce-Less Nicoise Salad from New York City-based Colleen Webb, MS, RDN has got you covered. Eliminating the lettuce from this traditional Nicoise salad allows people with inflammatory bowel disease to enjoy a salad without the roughage, says Webb. Roughage refers to high-fiber foods that are generally less tolerable with Crohns or colitis.
Lettuce-Less Nicoise Salad
- 2 hard-boiled organic eggs, roughly chopped
- 1 5-6 oz can tuna in water, drained
- 1 avocado, halved and roughly chopped
- 12 Kalamata olives, halved
- 3 Tbsp extra virgin olive oil
- Sea salt to taste
- Black pepper to taste, optional
- 3-4 Tbsp fresh dill, chopped OR 3-4 tsp dried dill
Directions:
Can You Eat Gravy On A Low
Related Articles
Your doctor may place you on a low-residue, low-fiber diet if youve recently had an intestinal surgery like a colostomy, or if you suffer from a digestive disorder such as ulcerative colitis, diverticulitis or Crohns disease. The purpose of the diet is to slow down bowel activity, decrease your stool bulk and lower the possibility of blockage in your intestinal tract. While youre on a low-residue diet, youll need to avoid high-fiber foods like whole grains, seeds, nuts, beans and raw fruits and vegetables in favor of easily digestible foods such as white-flour products and well-cooked fruits, vegetables and meat.
Read Also: Ulcerative Colitis And Lung Disease
Eating To Cope With The Pain Of Strictures
That being said, along with medications, a low fiber & low residue diets have a better likelihood of getting you back on your feet quicker after experiencing the pain and struggles of what strictures can cause to your digestive system. Low fiber diets may actually complicate things and stimulate more bowel movements, according to GI Associates.
With all of this being said, does this make you rethink your choices in the foods you’re consuming and most importantly, how they might be prepared?
Being on a low fiber and low residue diet doesn’t mean completely cutting out all roughage and foods that may cause you issues. You may have to take it easy on your GI tract during flares and especially after procedures and surgeries. More to come on which particular foods can be found in Part 2 of Low Residue Diets: Let’s Dig In!
Challenges In Creating Evidence
Although there are diet intervention trials that show promise in maintaining remission, their efficacy remains in question. The short duration of the interventions , the lack of a proper control group in some instances, and the small sample sizes make it very challenging for clinicians to draw firm conclusions from existing data. There is an overall lack of objective clinical and endoscopic disease markers. For example, many studies are completed retrospectively and they rely on patient questionnaires regarding disease symptoms, such as pain and stool frequency. Well-designed clinical trials in IBD are urgently required to define the precise role of each of these diets in the prevention or management of IBD. Up until now, the role of diet in IBD is highly undermined by lay and anecdotal reports without sufficient scientific proof.
High quality diet intervention studies for the treatment of IBD need to include the following: quantification of baseline intake of the habitual diet monitoring of diet adherence through food recalls large prospective, control trials over a longer-term use of a control diet to determine the specificity of observed effects to the intervention use of a variety of endpoints to monitor response to diet interventions and consider the use of IBD animal models to discover the mechanisms of pathogenesis.
Read Also: What Foods Should I Avoid With A Stomach Ulcer
Can Food Cure Crohn’s Or Colitis
You may come across diets that claim to cure Crohns or Colitis, but there isnt any evidence to prove that these work. A healthy, balanced diet will give you nutrients that are important to help you stay well.Some people find that making small changes to their diet, for example avoiding spicy food, helps them cope with their symptoms. If cutting out a food makes no difference to your symptoms, make sure you start eating it again to avoid missing out on important nutrients.There are times when your IBD team or dietitian may advise you to change your diet, for example, after surgery or if you have a narrowing in your small intestine, called a stricture. Some people, such as children or people with Crohns, may benefit from a liquid diet, called exclusive enteral nutrition.Always speak to your GP or a dietitian before making any big changes to your diet.
Ive tried just about all the different diets for Ulcerative Colitis and just gone round in a complete circle, not finding any success, only causing problems and stress! I now realise the most important thing is to eat a balanced diet and enjoy my food!
Trevor
Gravy Options And Preparation
You can have canned or homemade gravy on a low-residue diet. If you purchase pre-made gravy, choose a low- or no-sodium brand to help keep your sodium under the 2,300-milligram daily intake advised by the Food and Nutrition Board. You can prepare cream gravy with milk or cream, but remember to count the dairy used in this gravy as part of the 2-cup milk limit recommended on the low-residue diet. Avoid adding spicy seasonings like chili powder, cayenne pepper or hot sauce to your gravy, cautions Medline Plus, and do not cook or prepare gravy made with spicy sausage.
Read Also: What Are The Symptoms Of An Ulcer In Your Stomach
What To Know About The Low
Individuals that struggle with inflammatory bowel disease , Crohns disease, gastroesophageal reflux disease , ulcerative colitis, or other digestive conditions may be able to reduce or diminish symptoms by simply changing their diet. What you put into your body, and how you nourish your body matters in healthcare outcomes especially for the individuals struggling with one or more of the conditions listed above. Changing your eating habits or eliminating certain foods from your diet entirely may help reduce the effects or symptoms of gastrointestinal disorders
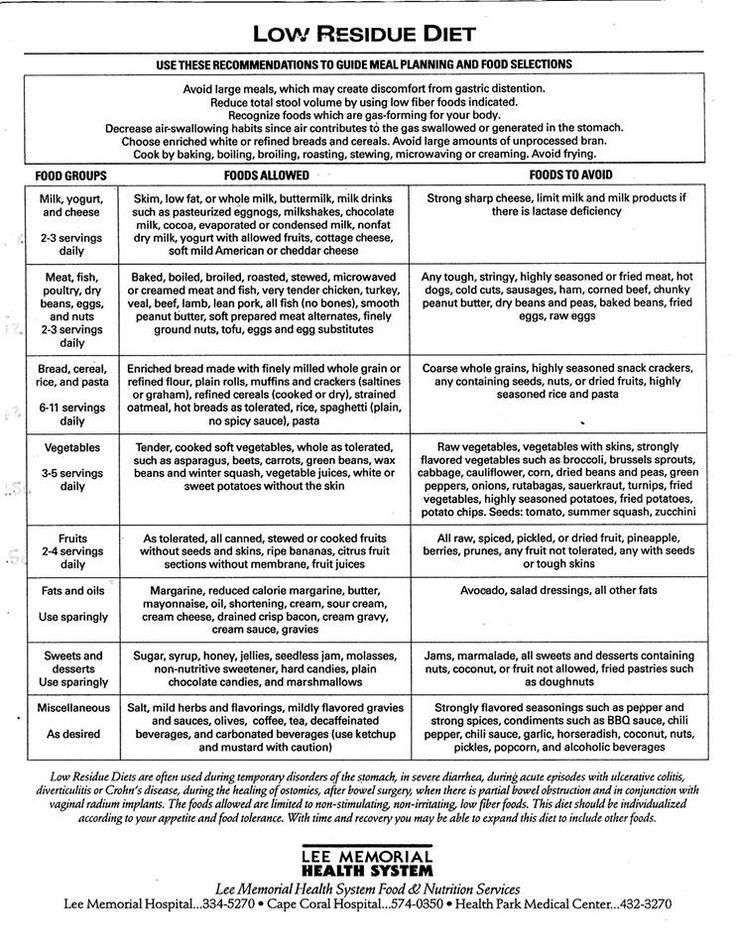
Low Fiber/low Residue Diet
A low fiber/low residue diet is designed to reduce the frequency, volume, and bulk of stools while it prolongs intestinal transit time. In certain medical conditions and/or before and after abdominal/intestinal surgeries or cancer treatments it is important to restrict fiber intake and avoid foods that increase bowel activity. This diet may also be used to treat diarrhea and to reduce the possibility of intestinal blockage when the intestines are narrowed for any reason. A low residue diet typically contains less than 10 grams of fiber per day. Extended use of this diet may not provide required amounts of vitamin C, calcium, and folic acid because of the lack of fruits and vegetables. Supplements may therefore be recommended. It is also important to stay well hydrated, especially during active disease. Many low fiber/low residue products are available in the health food or organic sections of most grocery stores.
Recommended Reading: L Glutamine Ulcerative Colitis Dosage
What Is A Low Residue Diet
A low residue diet is followed to put as few demands on the digestive tract as possible. Its similar to a low fiber diet, but it also excludes some foods that can stimulate bowel contractions.
Residue refers to material left in your digestive tract after the initial stages of digestion are finished. These materials often contain a lot of fiber because the body cant fully digest fiber.
A low residue diet restricts foods that contain indigestible material. This causes the body to produce smaller amounts of stool less frequently.
A low residue diet is typically recommended for people with inflammatory bowel disease flares, for bowel surgery and colonoscopy prep, and for patients with infectious colitis or acute diverticulitis.
Dietary Fat Intake As A Risk Factor For Ibd
There have been conflicting data on the association between dietary fat intake and the development of IBD, as many of the studies are retrospective and use small sample sizes. However, a very large, long-term, prospective study completed over 26 years did not observe a significant association with increased risk of developing CD or UC with total dietary fat intake, saturated fatty acids and monounsaturated fatty acids , which has been well supported by other research studies . A growing body of scientific evidence indicates that the Mediterranean diet pattern has been associated with significant improvements in health status and decreases in inflammatory markers in humans . The protective effect is hypothesized to be derived from the balance in fats, which includes incorporating MUFA, SFA and fish intake . While a few studies do show that MUFAs are beneficial during colitis, studies on the effects of SFA and PUFAs on gut health are controversial.
The Nurses Health Study cohorts reported high, long-term intake of trans-unsaturated fatty acids was associated with a trend towards an increased incidence of UC but not CD . An increased relative risk of developing IBD has also been associated with frequent intake of fast foods . The relative risk associated with the consumption of fast foods at least two times a week was estimated at 3.4 for CD and 3.9 for UC . Frequent fast food intake, defined as more than once a week, was significantly associated with a risk of UC and CD .
Don’t Miss: Side Effects Of Ulcerative Colitis
What Should I Eat
Its not always easy knowing what foods best fuel your body, especially when you have Crohn’s disease or ulcerative colitis. Your diet and nutrition are a major part of life with inflammatory bowel disease , yet there is no single diet that works for everyone.
Nutrition affects not just your IBD symptoms, but also your overall health and well-being. Without proper nutrients, thesymptoms of your Crohns disease or ulcerative colitis can cause serious complications, including nutrient deficiencies, weight loss, and malnutrition.
We have several tips for a healthy diet thats well-balanced and nutrient rich. These tips are for educational purposes only. You should work with your doctor or a dietitian specializing in IBD to help you develop a personalized meal plan.
Watch our with Emily Haller, registered dietitian at Michigan Medicine! Tune in to hear Emily review diet facts, debunk myths, speak about restrictions, and highlight ongoing research.