Is Zinc Good For Ulcerative Colitis
There is a substance called zinc. Zinc helps the body fight off infections. The level of zinc in your system can be affected by a number of symptoms of both Crohns disease and ulcerative colitis. Irritable bowel syndrome . Irritability is a common symptom of IBS, which is characterized by abdominal pain, bloating, diarrhea, and constipation.
It can also be caused by a number of other conditions, such as diabetes, high blood pressure, heart disease, or high cholesterol levels. Symptoms can range from mild to severe, depending on the severity of the symptoms and the amount of time youve had the condition. In some cases, you may not have any symptoms at all.
However, if you do have symptoms, its important to see your doctor as soon as possible to rule out other possible causes of your symptoms. If you dont see improvement within a few weeks, see a gastroenterologist for a more thorough evaluation and treatment plan. Inflammatory boweldisease . Inflammation is the process by which the immunesystem attacks and destroys healthy tissue.
IBD is an autoimmunedisease in which your body attacks your own bodys own tissues and organs.
Mechanism Of Action Of Probiotics For Gut Health
Probiotics, as per pieces of evidence, are in charge of keeping your immune system in check. Your mucosal immune system in your gut will be activated. As a bonus, probiotics correct the mucosal immune systems function, halting further inflammation.
They can also repair the damaged intestinal lining caused by ulcers. They accomplish this by stimulating mucus production and preserving the integrity of the intestinal tight junction. Therefore, mucus production safeguards the intestinal wall by coating it in a protective layer. As a result, you may be able to avoid getting sick from potentially harmful bacteria in the food or drink you ingested.
Who Is At Risk Of Ulcerative Colitis
- Age: Ulcerative colitis may affect any age group, although there are peaks at ages 15 to 30 years, and again at ages 50 to 70 years.
- Race/ethnic background: Ulcerative colitis is more common among caucasians and in people of Ashkenazi Jewish descent.
- Family history: People with a first-degree relative with ulcerative colitis are at greater risk of developing the condition.
Read Also: How To Treat A Diabetic Ulcer
Read Also: Remicade Dosing Schedule For Ulcerative Colitis
Will Probiotics Cure My Ibd
No. Unfortunately there is currently no cure for IBD.
However, some people have found that some probiotics assist in alleviating some symptoms of their IBD. If you choose to take a probiotic it is recommended you do so alongside any other treatment you are undergoing and that you discuss taking it with your doctor before starting.
People who report success with probiotics have found a reduction in symptoms such as bloating, diarrhoea, fatigue, skin conditions and constipation. Probiotics are increasingly being recognised to help people who have irritable bowel syndrome. Many people with IBD suffer from IBS too.
The success rate varies from person to person and a probiotic that may produce results for one person may not do the same for another.
The Probiotic Enema To Deal With Uc
As disagreeable as it might sound, you may select to immediately apply probiotics to your colon through an enema. The benefit is that the great micro organism dont should undergo the cruel surroundings of your digestive system to achieve the colon. Round 60 p.c dont survive that abdomen acid waterslide. Extra analysis is required on the effectiveness of this therapy for UC, however one 2010 examine referred to as it a well-tolerated treatment alternative. A 2011 examine discovered that administering some strains with an enema together with oral medicine could also be helpful for youngsters with UC.
Read Also: How Do You Know You Have A Stomach Ulcer
Is There Harm In Taking A Probiotic
People who live with IBD might wonder what harm there could be in taking a probiotic. For one thing, it might be expensive. For another, it might not help.
While in some cases, probiotics might not have any adverse side effects, for some people it could lead to bloating, gas, or diarrhea. Sometimes these effects will go away over time and with continued use of the probiotic.
Another potential harm is the cost: in some cases probiotics can be quite expensive. If theyre not giving any benefit, that is a problem, especially for people who already have high medical costs.
Whats less well understood is if a probiotic might be used instead of receiving a treatment for IBD that has been proven to work in clinical trials. The harm would be in taking probiotics that might not have an effect and in forgoing other treatment.
Read Also: What Probiotic Is Good For Constipation
Relationship Between Ulcerative Colitis And Probiotics
November 2, 2022, Samsa Latif,
Gut health and probiotics are well-known partners. Helpful in treating various gastrointestinal issues, such as gastroenteritis, and boosting general immunity.
To determine if probiotics are helpful in the treatment or prevention of ulcerative colitis, it is necessary first to understand the condition.
Read Also: What To Eat With Gastric Ulcer
Can Probiotics Treat Other Gi Issues
Studies show that probiotics help with symptoms of inflammatory bowel disease. But more research to form a standard treatment goes on.
Research into whether probiotics may help people with Crohnâs disease is less clear. The studies have been small, and we need more research into what types of probiotics might work. Because of this, doctors aren’t likely to recommend probiotics to people with Crohnâs disease.
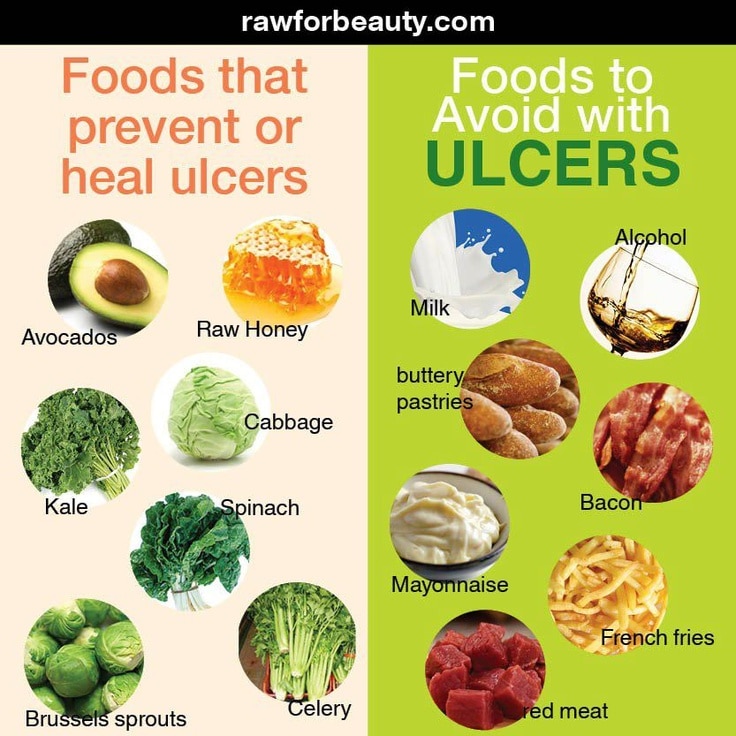
Youre Not Avoiding Trigger Foods
Theres no food or food group that causes or cures ulcerative colitis, Yun explains. But many people with UC say that certain foods either bring on symptoms or make them worse.
During a flare-up, your doctor may recommend adjustments to your diet. This can mean avoiding foods that trigger symptoms, such as bloating, diarrhea, and cramping. For example, dairy products can be particularly irritating for people who have both UC and lactose intolerance.
Aside from dairy, common trigger foods include beans, whole grains, nuts, seeds, some raw fruits and vegetables, high-fat foods, sugary foods, and sugar alcohols . If youre trying an elimination diet to determine which foods you need to avoid, keep a food diary, and always work with a healthcare practitioner to ensure youre getting all the nutrients you need.
Read Also: How To Heal Colon Ulcers
What Is The Best Diet For Managing Microscopic Colitis
There is no microscopic colitis diet per se, but diet can play a role in managing your symptoms by reducing the foods that trigger them and promoting anti-inflammatory foods. Your trigger foods will be specific to you, however, and identifying them can take some trial and error. Your doctor may suggest:
Eliminating common triggers
Some of the most common trigger foods for microscopic colitis include:
- Artificial sweeteners.
Low fat and low fiber
To manage flare-ups, some healthcare providers recommend a gastrointestinal soft diet, which is made up of low fat and low fiber foods. Reducing fat and fiber in your diet gives your digestive system less work to do. There may still be particular foods in the diet that trigger you, though.
Elimination diet
One way to isolate trigger foods is to try an elimination diet, such as the low-FODMAP diet. This short-term diet eliminates certain classes of foods and then reintroduces them in a systematic way, to find out which ones you are sensitive to. A registered dietician guides you through the process.
Anti-inflammatory diet
Certain foods, such as polyunsaturated fats, have been shown to reduce inflammation. The Mediterranean diet is a good example of a diet that promotes anti-inflammatory foods. Turmeric is another well-known anti-inflammatory agent that you can use in food.
Failure To Have A Gastroenterology Specialist On Your Side
Your primary care physician can only do so much for you. In order to adequately manage and treat your Crohns or ulcerative colitis, you will need to see a specialist for regularevaluation. In fact, you should have a whole team of doctors working for you, from surgeons to radiologists to nutritionists however, your gastroenterologist should be your main point of contact when it comes to your condition.
We treat patients with Crohns and ulcerative colitis as well as a variety of other gastrointestinal diseases, including colon cancer, hepatitis, biliary diseases, esophageal disorders, and peptic ulcer disease. Our specialists can offer you more tips on how to best manage your condition, and work with you one-on- one to develop a workable treatment plan.
Please note, the information provided throughout this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and video, on or available through this website is for general information purposes only. If you are experiencing related symptoms, please visit your doctor or call 9-1-1 in an emergency.
GET OUR FREE NEWSLETTER
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
You May Like: Can You Have Constipation With Ulcerative Colitis
Speak To Your Physician Probiotics For Ulcerative Colitis
? Probiotics are microorganisms that we take into our our bodies to help our well being. Sometimes, theyre strains of micro organism that may assist enhance our digestion, or so-called good bacteria. Probiotic merchandise are meant to produce wholesome, gut-friendly micro organism to populate the intestinal wall. Probiotics are present in sure meals. In addition they are available dietary supplements, which can be found in a wide range of types, together with tablets and capsules. Whereas many individuals take probiotics to help their basic digestive well being, theyve additionally been used to deal with sure intestinal issues equivalent to gastroenteritis and a situation known as pouchitis. However can these good micro organism even be used to deal with ulcerative colitis ?
My Experience With Vsl#3
Ive been using VSL#3® with much personal success. Any time I take a stool test, the bacteria in the genus Lactobacillus and Bifidobacterium are often at acceptable levels which I know is thanks to VSL#3®. Its so important that these levels are acceptable because they are considered keystone bacteria for a healthy microbiome . I add VSL#3® to my morning iced coffee . Its pretty simple, I just put it in a shaker, along with collagen and some other supplements to keep my symptoms at bay. VSL#3® is a must-have, especially when Im in remission, because it keeps me regular and helps keep my symptoms toan absolute minimum.
It is important to consult with your healthcare provider to determine the appropriate dosage and length of therapy for your condition. It may take up to 1 month for the colonization of the gut to become optimally stable. VSL#3® Capsules and VSL#3® Unflavored 450B Packets are available for purchase without a prescription on www.vsl3.com. VSL#3 is stocked or available to order at all retail chains and independent pharmacies. VSL#3® is kept refrigerated behind the pharmacy counter so ask the pharmacist.
Don’t Miss: Method For Cleaning Leg Ulcers
How Will I Feel Taking Probiotics
Again, this really varies from person to person. Some people who take probiotics – whether they have IBD or not – report feeling bloated and gassy or have a short bout of diarrhoea at the beginning. This may be a reaction to the changes in bacteria in your gut. To help prevent this some probiotic companies recommend you start by taking a small dosage and build up to taking the full dose to allow your body to adjust. If you are concerned, or these symptoms persist, you should stop taking the probiotic and speak to your doctor.
Caution should be taken around taking probiotics when you are on immunosuppressant medications or are acutely unwell – always speak to your doctor before starting a probiotic to check it is safe for you to do so.
How The Gut Microbiome Works
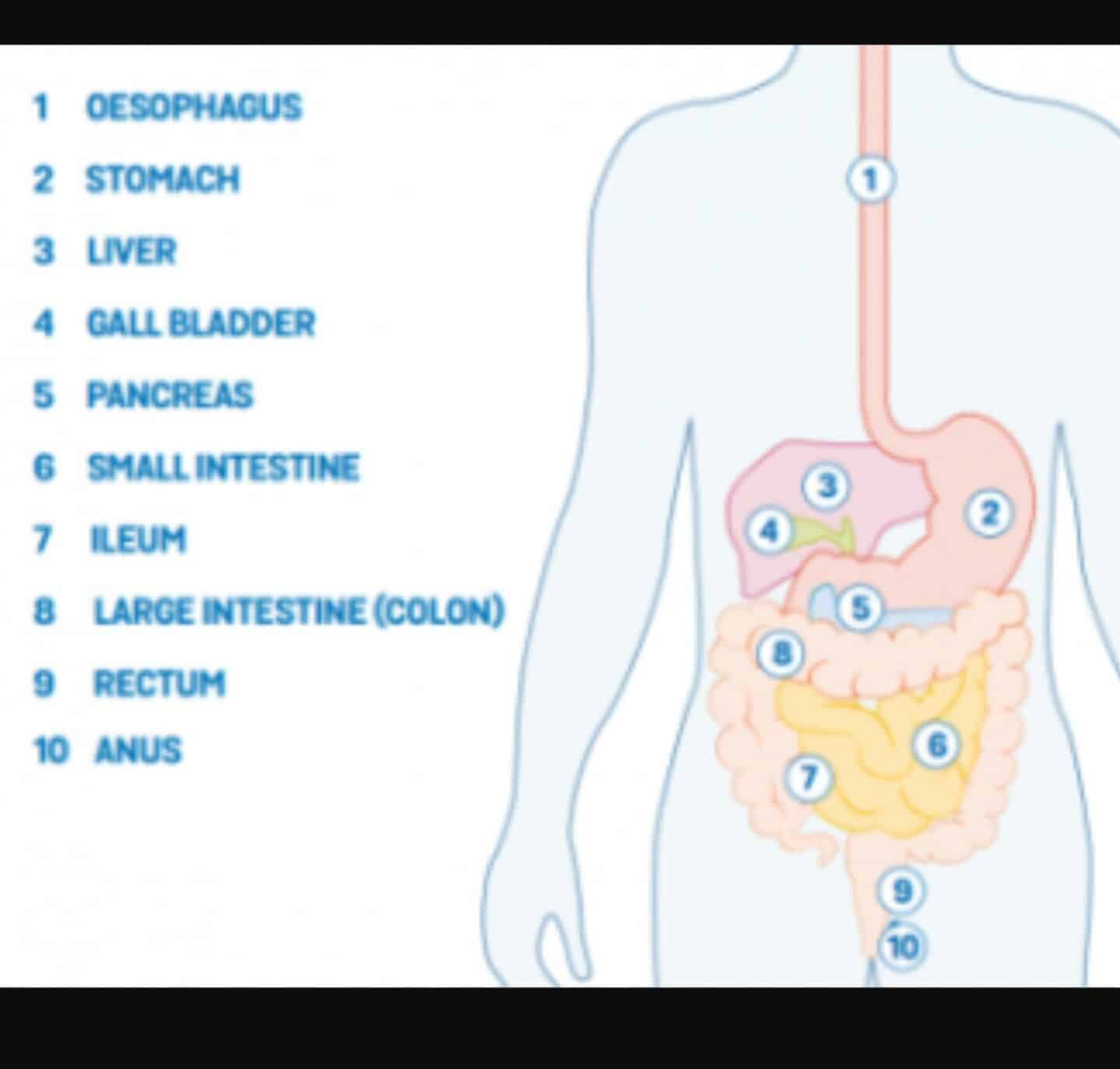
If all systems are operating normally, your large intestine serves as a home to a diverse mix of bacteria that produce and modify molecules that have beneficial physiological functions. This “good” gut bacteria protects the intestine from harmful bacteria that could invade it. It does this by releasing a specialized, anti-inflammatory and immune-beneficial substance called butyrate, a fatty acid. This, in turn, protects the innermost lining of the intestine , which is key to a healthy gut.
The intestinal barrier is made up of a tightly knit network of cells that maintain the guts integrity. A healthy gut relies on the interactions between the gut microbiome and this barrier. If something upsets the balance between the good and bad bacteria in the microbiome or if theres a dysfunction in the intestinal barrier, harmful bacteria can invade the barrier itself, resulting in the intestines immune cells being activated and, ultimately, chronic intestinal inflammation, like you find in people with UC. The interaction between the host, intestinal microbiota, and anti-inflammatory metabolites these bacteria produce, may be a key factor in ulcerative colitis, says Paul-Peter Tak, M.D., Ph.D., a professor of medicine at Amsterdam University Medical Centre in the Netherlands.
Read Also: Interventions To Prevent Pressure Ulcers
Ulcerative Colitis: This Is Why Youre Here Right
- Why did you get Ulcerative Colitis? The short answer is that scientists still dont know. Genetics are a major risk factor, but some people without a family history develop the condition
- Ulcerative Colitis is caused by an autoimmune response from your body
- Your symptoms may include:
- GI: loose and urgent bowel movements, bloody stool, abdominal pain and cramps, persistent diarrhea
- Non-GI: appetite loss, weight loss, nausea, low energy, anemia
- There are flares and periods of remission throughout disease course UC is different from other types of colitis because tiny ulcers form, causing long term inflammation
How To Take Probiotic Supplements
We cant stress enough that its a good idea to visit a doctor and/or a registered dietitian before taking something new to treat ulcerative colitis.
They may have some advice about which probiotic to take and what dosage might be right for you.
Probiotic dosage for ulcerative colitis is not an exact science. The dosages found to be effective in various studies usually range from 2 billion to 25 billion colony-forming units . The more bacteria, the merrier.
Check the expiration date and make sure to store them properly, refrigerating them if recommended on the packaging. These are living organisms that require a little TLC, and they die out over time if not used.
Don’t Miss: Foods That Heal Stomach Ulcers
What Are Probiotics And Why Would You Need Them
Among the estimated 100 trillion microbes living in your gut, there are some really helpful bacteria. They break down stuff like fiber into nutrients that your body then uses for energy and as a weapon against everything from cardiovascular disease to cancer.
Bottom line
The pro in probiotics refers to good bacteria that you can ingest as food or in tablet form, among other methods. If the good bacteria survive the journey through your digestive system into your gut, they will settle in and colonize it, eventually driving out the bad guys.
How Is It Diagnosed
To diagnose ulcerative colitis, a doctor will ask about your symptoms, do a physical exam, and do a number of tests. These tests may include colonoscopy, blood tests, and stool sample testing. Testing can help rule out other problems that can cause similar symptoms, such as Crohn’s disease and irritable bowel syndrome.
Also Check: Over The Counter Ulcerative Colitis
What Foods Should I Eat If I Have Ulcerative Colitis
Many people with ulcerative colitis can eat a normal diet, but during flare-ups your diet may need to be altered to help reduce your symptoms.
Eating during a flare up
When you are experiencing a flare-up, eating a temporary diet of low-residue or low-fibre foods may reduce the amount and frequency of the stools you pass and allow your colon to heal.
Foods to eat during a flare-up include:
- Low-fiber fruits: bananas, cantaloupe, honeydew melon. Cooked, pureed, canned or peeled fruits. Avoid skins and seeds.
- Lean protein sources: fish, lean cuts of pork, white meat such as chicken, soy, eggs, firm tofu and smooth nut butters
- Refined grains: sourdough, potato or gluten-free bread, white pasta, white rice and oatmeal
- Seedless, skinless vegetables: fully cooked, peeled vegetables such as asparagus tips, cucumbers, potatoes and squash
- Oral nutritional supplements or homemade protein shakes
Eating when in remission
When symptoms have lessened or subsided, many people with ulcerative colitis can resume a more normal, well-balanced diet and reintroduce foods slowly.
Slowly reintroduce:
You May Like: Home Remedies For Stomach Ulcers During Pregnancy
What About Prebiotics For Ulcerative Colitis Probiotics Uc
? Among the many estimated 100 trillion microbes dwelling in your intestine, there are some actually useful micro organism. They break down stuff like fiber into vitamins that your physique then makes use of for vitality and as a weapon in opposition to the whole lot from heart problems to most cancers.
Backside line The pro in probiotics refers to good micro organism that you would be able to ingest as meals or in pill type, amongst different strategies. If the great micro organism survive the journey by way of your digestive system into your intestine, theyll settle in and colonize it, finally driving out the dangerous guys.
Do they assist? The decision on probiotics and ulcerative colitis A number of research have concluded that sure strains of micro organism may also help forestall a relapse of ulcerative colitis signs. The correct mixture of strains, akin to these present in VSL#3, may even assist individuals go into remission throughout a flare-up. Extra analysis is required although, as a result of the phrase probiotics refers to numerous species of micro organism. Evaluating every of them and their myriad combos requires an excessive amount of testing to determine how greatest to deploy them for every distinctive case of IBD.
Also Check: How Are Stomach Ulcers Caused