Dietary Fat Intake As A Risk Factor For Ibd
There have been conflicting data on the association between dietary fat intake and the development of IBD, as many of the studies are retrospective and use small sample sizes. However, a very large, long-term, prospective study completed over 26 years did not observe a significant association with increased risk of developing CD or UC with total dietary fat intake, saturated fatty acids and monounsaturated fatty acids , which has been well supported by other research studies . A growing body of scientific evidence indicates that the Mediterranean diet pattern has been associated with significant improvements in health status and decreases in inflammatory markers in humans . The protective effect is hypothesized to be derived from the balance in fats, which includes incorporating MUFA, SFA and fish intake . While a few studies do show that MUFAs are beneficial during colitis, studies on the effects of SFA and PUFAs on gut health are controversial.
The Nurses Health Study cohorts reported high, long-term intake of trans-unsaturated fatty acids was associated with a trend towards an increased incidence of UC but not CD . An increased relative risk of developing IBD has also been associated with frequent intake of fast foods . The relative risk associated with the consumption of fast foods at least two times a week was estimated at 3.4 for CD and 3.9 for UC . Frequent fast food intake, defined as more than once a week, was significantly associated with a risk of UC and CD .
Would You Like More Information On How To Start A Low Fodmap Diet For Ulcerative Colitis
Tap the blue button below to download our Eat This, Not That list as well as additional resources for IBS and colitis
SEND ME THE LIST
About Kimberly Yawitz
Kim Yawitz is a registered dietitian and nutritionist in St. Louis, Missouri.
She currently works with sports nutrition and weight management clients for a private practice. Prior to that Kim worked as an inpatient clinical dietitian, developing nutrition care plans for patients with health concerns ranging from autoimmune disease to critical illness.
Learn more about her on the About page.
Joe Leech, Dietitian
Recent Posts
What Should I Eat If I Have Ulcerative Colitis
If you have ulcerative colitis, you should eat a healthy, well-balanced diet. Talk with your doctor about a healthy eating plan.
Ulcerative colitis symptoms may cause some people to lose their appetite and eat less, and they may not get enough nutrients. In children, a lack of nutrients may play a role in problems with growth and development.
Researchers have not found that specific foods cause ulcerative colitis symptoms, although healthier diets appear to be associated with less risk of developing IBD. Researchers have not found that specific foods worsen ulcerative colitis. Talk with your doctor about any foods that seem to be related to your symptoms. Your doctor may suggest keeping a food diary to help identify foods that seem to make your symptoms worse.
Depending on your symptoms and the medicines you take, your doctor may recommend changes to your diet. Your doctor may also recommend dietary supplements.
Also Check: What Are The Symptoms Of An Ulcer In A Child
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
More Information About Ulcerative Colitis

According to George Washington University, colitis is a chronic digestive disease characterized by inflammation of the inner lining of the colon. Infection, loss of blood supply in the colon, Inflammatory Bowel Disease and invasion of the colon wall with collagen or lymphocytic white blood cells are all possible causes of an inflamed colon.
The following diseases fall into the colitis/IBD category they all can be treated with a combination of medication and improvements to your eating habits:
Read Also: Carbohydrate Diet For Ulcerative Colitis
What Are The Best Vegetables For Ulcerative Colitis
While every gut is different, many people with ulcerative colitis find that they can tolerate a wide range of vegetables when their symptoms are in remission , says Arielle Leben, RD, a member of the Inflammatory Bowel Disease Center Clinical Care Team at NYU Langone Health in New York. These may include:
- Peeled, shredded carrots
What makes these vegetables a particularly good bet? Many are high in soluble fiber, which pulls water into the GI tract to turn the fiber into a thick, gel-like substance during digestion. This type of fiber may be beneficial to patients in a flare experiencing diarrhea, because it slows digestion and can improve the consistency of bowel movements, Leben says.
At the same time, theyre lower in insoluble fiber, which can be irritating to the gut, particularly during a flare. When experiencing active symptoms, a diet low in insoluble fiber can be part of the management process to reduce irritation in the GI tract, Warren explains. Avoiding insoluble fiber might help prevent or reduce bloating, diarrhea, or abdominal pain.
Not all of these vegetables may be right for everyone, and you might find that you can tolerate certain vegetables when youre symptom free but not during a flare. Ulcerative colitis diets arent one size fits all, varying from person to person, Warren says.
Gut Microbiota And Ibd
Any alteration of the bowel eubiosis or in the composition of the microbiota is defined as dysbiosis. IBD is associated with alterations in the composition of the intestinal microbiota, characterised by decreased diversity, reduced proportions of Firmicutes, and increased proportions of Proteobacteria and Actinobacteria . Some of the bacterial species with pro-inflammatory effect are enriched in patients with IBD , while anti-inflammatory species are largely reduced in IBD . For example, patients with active IBD have been shown to have a lower abundance of Clostridium coccoides, Clostridium leptum, Faecalibacterium prausnitzii and Bifidobacterium . Prospective studies investigating the role of microbiome changes on the disease course have been scarce. A Dutch study based on 10 CD and nine UC patients reported patient-specific shifts in the microbial composition, but could not demonstrate general changes in the microbial composition or diversity . A Spanish study followed up 18 UC patients over the course of one year in those who remained in remission Faecalibacterium prausnitzii increased steadily, while in those who relapsed it did not .
Don’t Miss: Natural Ways To Heal Esophageal Ulcers
How Can I Track Foods That Cause Flare
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Vegetables To Avoid With Ulcerative Colitis
When it comes to veggies that can potentially trigger your symptoms or make them worse, cruciferous vegetables, such as broccoli, cauliflower, Brussels sprouts, and cabbage, are often at the top of the list. Theyre common triggers for gas and bloating, regardless of whether they are raw or cooked, Leben says. Depending on how they affect you, you may find that you need to steer clear during flares or cut them out of your diet completely.
Be careful with large amounts of tough, uncooked greens, too, such as kale salads. While leafy greens that have been cooked until soft may be tolerable for some, the rough texture of the raw greens can be irritating, Warren notes. But again, this will all depend on the patient, she says.
Salads dont have to be entirely off limits, Warren and Leben say. If you find that raw vegetables work for you when youre not experiencing symptoms, go ahead and enjoy them in quantities you can tolerate.
Recommended Reading: What Is Bad For Ulcers
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Eating When You Are In A Flare
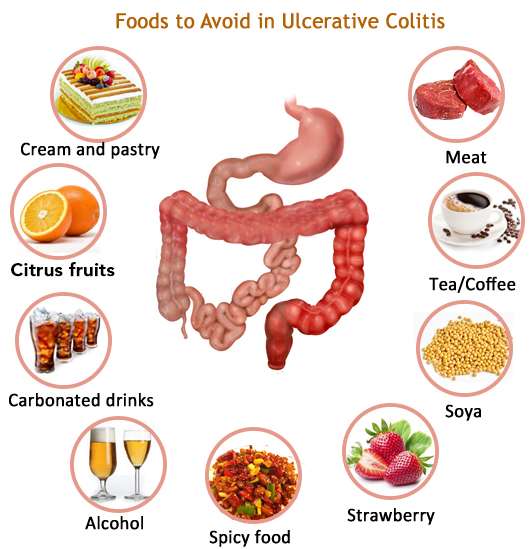
There are certain foods you may want to avoid when you are in an IBD flare, and others that may help you get the right amount of nutrients, vitamins, and minerals without making your symptoms worse.
Your healthcare team may put you on an elimination diet, in which you avoid certain foods in order to identify which trigger symptoms. This process will help you identify common foods to avoid during a flare. Elimination diets should only be done under the supervision of your healthcare team and a dietitian so they can make sure you are still receiving the necessary nutrients.
Some foods may trigger cramping, bloating, and/or diarrhea. Many trigger foods should also be avoided if you have been diagnosed with a stricture, a narrowing of the intestine caused by inflammation or scar tissue, or have had a recent surgery. Certain foods can be easier to digest and can provide you with the necessary nutrients your body needs.
You May Like: Foods Okay To Eat With An Ulcer
Diet Recommendations For Crohn’s Disease Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
Overview Of Uc And Causes
UC is a chronic condition of the gastrointestinal tract . It is a form of inflammatory bowel disease , causing inflammation, irritation, and sores, referred to as ulcers, in the innermost lining of the large intestine and rectum.
While the cause of UC is unknown, experts believe that changes in the gut microbiota and abnormal immune responses in the gut may UC. Genes also play a role since having first degree-relatives is the highest risk factor for IBD.
Environmental factors can IBD risk at an individual level, such as diet. They may also be factors that modify the risk to entire populations, such as air pollution or UV light exposure.
While diet does not directly cause UC, certain foods can trigger or worsen UC symptoms.
For more research-backed information about the microbiome and how it affects your health, please visit our dedicated hub.
Recommended Reading: Interprofessional Care For Ulcerative Colitis
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Donât Miss: Sample Meal Plan For Ulcerative Colitis
Get Regular Exercise To Reduce Uc Inflammation
Snider says exercise is useful in managing many of the complications associated with ulcerative colitis, including decreased bone density, a weakened immune system, emotional health problems, stress, and weight gain.
âTry to engage in a moderate-intensity exercise like swimming or biking, three or four days per week,â he says. A review published in August 2016 in Pharmacological Reports noted that moderate exercise releases protective myokines such as irisin from working skeletal muscles, which promotes healing and helps with inflammatory bowel disease inflammation.
Snider also strongly recommends yoga as a natural treatment for ulcerative colitis, as it promotes relaxation and targets the digestive system, flooding the area with oxygen and nutrition for healing. Find what type and frequency of exercise works for you and take it slow: Too much exercise can cause mild systemic inflammation.
Research indicates that stress plays a role in inflammatory bowel diseases such as ulcerative colitis. Researchers analyzed data on 2,007 adults in a Swiss IBD study and found a relationship between depression and anxiety and disease symptoms. The results were published in June 2016 in Clinical Gastroenterology and Hepatology.
Counteract stress with relaxation techniques such as meditation, deep breathing, and progressive muscle relaxation to help your body relax.
Donât Miss: Do Ulcers Cause Acid Reflux
Don’t Miss: Things To Eat When You Have An Ulcer
What To Eat In Remission
When in remission, a person will not have symptoms. While there is not always a way to avoid them from returning, a person may prolong the state of remission.
A person will benefit the best from a diverse and nutrient-rich food source. Foods to consider include:
- high fiber foods, unless the personâs doctor says otherwise
- healthy fats such as nuts, seed butter, and olive oil
It Can Be Challenging To Differentiate Between Crohn’s And Ulcerative Colitis
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
|
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
Don’t Miss: Acute Exacerbation Ulcerative Colitis Symptoms
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient.
Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high-calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAP stands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have an intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Dietary choices do not cause ulcerative colitis, but certain foods can trigger and worsen symptoms. Learning to identify trigger foods can help reduce the frequency and severity of ulcerative colitis symptoms.
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Don’t Miss: Blood Clots In Stool With Ulcerative Colitis