Description Of The Intervention
This review includes RCTs of any dressings or topical agents applied directly onto or into wounds and left in situ, as opposed to products used to irrigate, wash or cleanse wounds and those that are only in contact with wounds for a short period.
Dressings
The classification of dressings usually depends on the key material used in their construction, and whether additional substances are added to the dressing. Several attributes of an ideal wound dressing have been described , including the ability of the dressing to:
- absorb and contain exudate without leakage or strikethrough, in order to maintain a wound that is moist but not macerated
- achieve freedom from particulate contaminants or toxic chemicals left in the wound
- provide thermal insulation, in order to maintain the optimum temperature for healing
- allow permeability to water, but not bacteria
- optimise the pH of the wound
- minimise wound infection and avoid excessive slough
- avoid wound trauma on dressing removal
- accommodate the need for frequent dressing changes
- provide pain relief and
- be comfortable.
There are numerous and diverse dressings available for treating pressure ulcers and their properties are described below.
Absorbent dressings are applied directly to the wound and may be used as secondary absorbent layers in the management of heavily exuding wounds. Examples include Primapore , Mepore and absorbent cotton gauze .
Topical agents
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
What Are The Symptoms Of Stage 2 Pressure Ulcers
Stage 2 pressure ulcers are open, shallow, broken wounds with a red base. Intact or incompletely ruptured blisters may also be present with clear fluid or pus seeping from the affected area, and the skin to it adjacent may be discolored. It may involve both the dermis and epidermis of the skin.
Stage 2 bedsores are common in ankles and heels, back of the head, hip, shoulder blades, and tailbone. However, it can develop in any part of the body under constant pressure. Still, areas near bones are at a higher risk.
There is more significant pain in stage 2 bedsores than in stage 1 bedsores. The pain decreases as the sore worsens but becomes harder to treat, leading to fatal complications.
Also Check: Best Smoothies For Ulcerative Colitis
Also Check: Do Ulcers Cause Weight Loss
Treatments Your Physician May Prescribe
In addition to self-care, your doctor might prescribe special pads or mattresses. Special dressings may be used, and whirlpool baths or surgery may be recommended to remove dead tissue. Infection requires antibiotic treatment. Sometimes deep wounds may require surgery to restore the tissue. Experimental work is now being done using honey preparations, high-pressure oxygen, and application of chemicals that stimulate cell growth .
Recommended Reading: Can You Drink Ensure With Ulcerative Colitis
What Is A Stage 4 Bedsore
Stage 4 bedsores are the most severe form of , also called pressure sores, pressure ulcers, or decubitus ulcers. A stage 4 bedsore is characterized by a deep wound that reaches the muscles, ligaments, or even bone. They often cause residents to suffer extreme pain, infection, invasive surgeries, or even death.
A stage 4 bedsore may be an unfortunate sign of . Residents of nursing homes may develop these sores if the staff fails to treat earlier-stage sores.
Thankfully, financial compensation may be available if your loved one develops a stage 4 bedsore while living in a nursing home. Get a free case review to see if you can pursue compensation to help pay for medical treatment.
Victims of stage 4 bedsores can take legal action.
to learn if you can access financial aid and hold abusive nursing homes accountable.
Read Also: What To Take If You Have A Stomach Ulcer
Keep The Area Clean And Dry
Moisture exacerbates skin breakdown, so it is important to keep a pressure ulcer clean and dry. If a pressure sore develops on the buttocks or near your genital area, try to prevent urine or sweat from sitting on or near the pressure sore.
Stage 1 pressure ulcers may be cleaned with warm water and soap. Do not use hydrogen peroxide or other products that may further damage the skin. You only want to use products that are gentle, protective, and wont cause further harm. If your pressure ulcer is advanced, your healthcare provider will likely give you an antibacterial cream or an oral antibiotic to help treat/prevent potential infection. Follow their instructions carefully on how to care for your pressure ulcer.
With stage 2 and stage 3 pressure injuries, you can use an antibacterial spray to clean the wound every few hours. Once it is clean, you can dry the area with non-adhesive gauze and cover with a fresh dressing. Some pressure ulcers may need to be left uncovered if they are in an area prone to excessive sweating or possible urine contamination. Follow your doctors advice for the specifics to your wound.
The Icd Code L89 Is Used To Code Pressure Ulcer
Pressure ulcers, also known as pressure sores, bedsores and decubitus ulcers, are localized injuries to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. The most common sites are the skin overlying the sacrum, coccyx, heels or the hips, but other sites such as the elbows, knees, ankles or the back of the cranium can be affected.
| Specialty: |
You May Like: Ulcerative Colitis Biologics Side Effects
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Recommended Reading: Difference Between Ulcerative Colitis And Crohns Disease Ppt
Posthoc Sensitivity Analysis Dressings Only
For the individual network, we also investigated, posthoc, our original assumption that topical agents could be used in place of dressings, by examining only the network of studies involving two or more dressings . There were no threearm trials remaining and the 30 studies compared 12 interventions in a total of 1627 participants experiencing 641 events, with 16 direct contrasts and 66 mixed treatment contrasts. The NMA rankings were similarly imprecise .
For the group network, 17 studies compared five interventions in a total of 798 participants experiencing 304 events, with five direct contrasts and 10 mixed treatment contrasts. This network was still sparse in terms of total participants, but, on average, there were more events per contrast. The posthoc sensitivity analysis had less overlap of rankograms than the full group network, and the mean rank was closer to a whole number one SUCRA value was 0 and another was 0.9. The mean ranks were: proteasemodulating 1.4 advanced 1.9 basic 3.1 antimicrobial 3.7: advancedantimicrobial 4.9. For the comparisons with basic dressing, effect estimates were similar to those in Table 4 but CIs were still wide.
You May Like: Natural Ways To Cure Stomach Ulcers
Pressure Ulcer And Non
Pressure ulcer and non-pressure chronic ulcer diagnostic codes are located in ICD-10-CM chapter 12, Disease of the skin and subcutaneous tissue. The concept of laterality is pertinant, and should be included in the clinical documentation for skin ulcers.ICD-10-CM codes for Pressure ulcers, located in Category L89, are combination codes that identify the site, stage, and the laterality of the ulcer. Possible stages are 1-4 and unstageable.
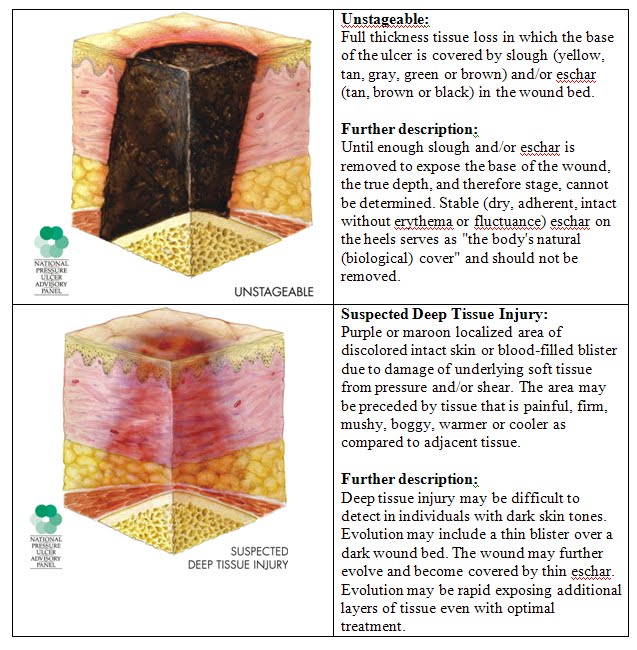
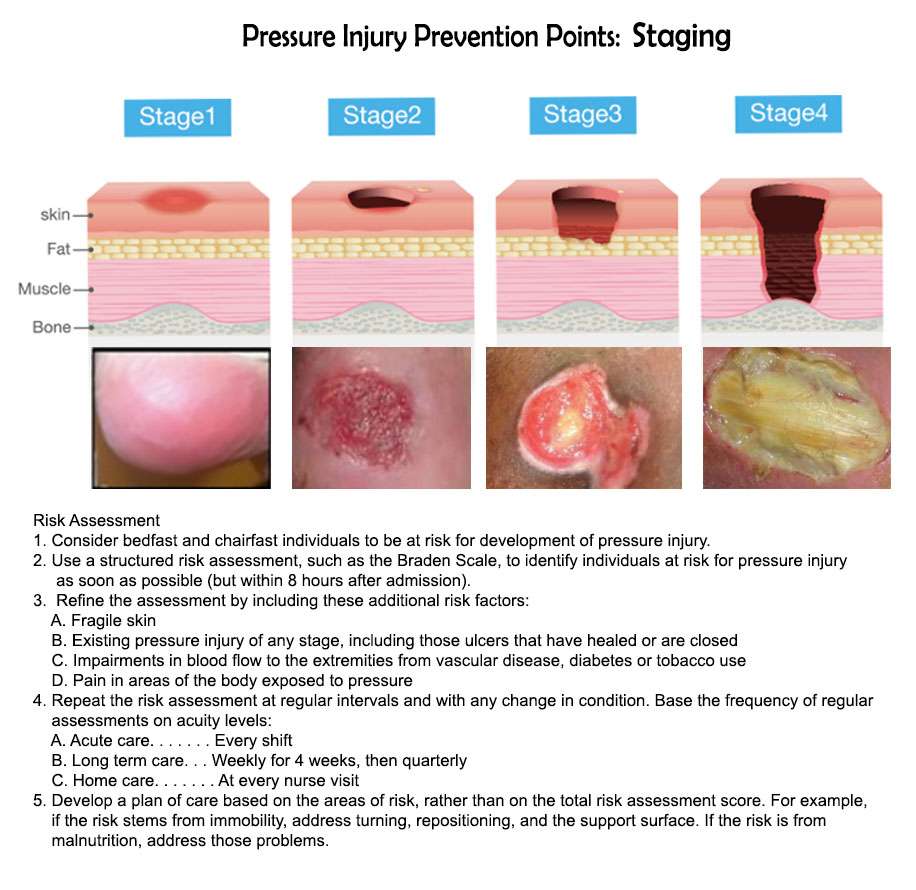
Stage 1: Skin changes limited to persistent focal edemaStage 2: An abrasion, blister, and partial thickness skin loss involving the dermis and epidermisStage 3: Full thickness skin loss involving damage and necrosis of subcutaneous tissueStage 4: Necrosis of soft tissues through the underlying muscle, tendon, or bone
Unstageable: Based on clinical documentation the stage cannot be determined clinically or for ulcers documented as deep tissue injury without evidence of trauma.An instructional note in ICD-10 states to code also any associated gangrene .Non-pressure chronic ulcers are similar to pressure ulcers in that they require documentation of the site, severity, and laterality. Category L97 and L98 are for Non-pressure ulcers, and have an instructional note to code first any associated underlying condition, such as:
Associated gangreneAtherosclerosis of the lower extremitiesChronic venous hypertensionThe severity of the ulcers is described as:Limited to breakdown of skinWith fat layer exposedWith necrosis of muscleWith necrosis of bone
What Is A Pressure Ulcer
A pressure ulcer happens when an area of skin, generally over a prominent bony structure, experiences excessive friction and breakdown. These commonly occur in settings where one is confined to a bed or a chair and is spending a lot of time in the same position. A pressure ulcer develops when there is significant damage not only to the upper layers of skin but in the deep bodily tissues beneath.
You are at high-risk for developing bedsores if you:
- Use a wheelchair
- Stay in bed for prolonged periods
- Are an older adult
- Have trouble moving on your own
- Have weak skin and/or impaired healing
- Are incontinent
- Have nutritional deficiencies
- Are mentally impaired
Pressure sores can happen anywhere on your body but are common at the bottom of the spine, on the buttocks, over the hip bones, on the soles of the feet, ankles, over the elbow joint, on the back of the head, and on the shoulders.
Recommended Reading: Normal Colon Vs Ulcerative Colitis
How Does A Pressure Ulcer Heal
With careful and consistent care, a bedsore can heal fully. The larger the pressure sore and the more advanced it is, the more time it will take to treat it. Again, a pressure ulcer takes days/weeks to develop and will take equally as long to fully heal.
There are many treatments for bedsores, most of which you can do yourself at home. Here is how to properly care for a pressure ulcer in the early stages. If you think your pressure sore has progressed to a stage 3 or 4, it is important to work with a medical professional to ensure proper healing and prevention of infection. It is important to recognize that in its late stages, a pressure ulcer is an open wound that is susceptible to infection, especially in those who may be immune-compromised.
When Sacral Ulcers Require Surgery
If you catch sacral ulcers early, then improving a persons diet and keeping them active while cleaning the wounds can reverse the damage. Once a person starts to show symptoms of Stage Three development, most medical professionals recommend surgery as the most effective curative.
To remove the dead skin that results from untreated sacral pressure, medical professionals will use the methods most appropriate for the patients situation. These methods can include:
- Biological treatment
Also Check: Can You Donate Blood If You Have Ulcerative Colitis
Read Also: Is Ulcerative Colitis Considered A Disability
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should move or be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
Criteria For Considering Studies For This Review
Types of studies
We included published and unpublished randomised controlled trials , irrespective of language of report. We did not identify any crossover trials, but we would have included them only if they reported outcome data at the end of the first treatment period and prior to crossover. We excluded studies using quasirandom methods of allocation . We highlighted trials in which three or more interventions were randomised.
Types of participants
We included studies that recruited people with a diagnosis of pressure ulcer, Stage 2 and above , managed in any care setting. We excluded studies that only recruited people with Stage 1 ulcers as these are not open wounds requiring dressings.
We accepted study authors’ definitions of what they classed as Stage 2 or above, unless it was clear that they included wounds with unbroken skin. Where authors used grading scales other than NPUAP, we attempted to map to the NPUAP scale.
Types of interventions
Interventions of direct interest
The interventions in this section were all those that can be directly applied as dressings or topical agents to open pressure ulcers. We presented results for these interventions and included them in summary tables. In the context of a network of competing treatments, there are no ‘comparators’.
Some of the interventions we considered were as follows:
Supplementary intervention set
Terminology
Types of outcome measures
Primary outcomes
- the proportion of wounds healed
- time to complete healing .
Recommended Reading: What To Eat If You Have Gastric Ulcer
Stages Of Decubitus Ulcers
The National Pressure Ulcer Advisory Panel has developed a series of four stages of a decubitus ulcer to aid in diagnosis and treatment.Stage I: The skin is discolored but not broken. Light-complexioned people may have red marks. Dark complexioned people may have a discoloration that is blue or purple. In some people, the discoloration is white.Stage II: Skin breaks open and the ulcer is shallow with a reddish or pinkish wound bed. There may be tissue death around the wound, or a fluid-filled blister.Stage III: Ulcer on the skin is deeper, affecting the fat layer and looking like a crater. Pus may be in the wound.Stage IV: Ulcer moves to deeper layers of muscle or bone. A dark material called eschar may be inside the ulcer.Unstageable: An ulcer that is yellow or green. It might have a brown scab covering it, or be soft and look pus filled. A dry and stable ulcer surface is the bodys natural protection and should be allowed to continue healing. However, if extensive tissue damage is evident, the covering might need to be removed for treatment.
Pressure Ulcer Of Unspecified Part Of Back Unstageable
- 2016201720182019202020212022Billable/Specific Code
- L89.100 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM L89.100 became effective on October 1, 2021.
- This is the American ICD-10-CM version of L89.100 â other international versions of ICD-10 L89.100 may differ.
- Applicable To annotations, or
You May Like: Can Ulcerative Colitis Cause Bad Breath
Recommended Reading: Ulcerative Colitis And Stomach Pain
The Efficacy Of Duoderm
A study by Michel Hermans treating small partial-thickness burns found that HydroColloid Dressings provide an optimum wound environment for more rapid re-epithelialization than either allografts or SSD. The cosmetic and functional results were also excellent.1 A meta-analysis of pressure ulcers performed by Matthew Bradley comparing a hydrocolloid dressing with a traditional treatment suggested that treatment with the hydrocolloid resulted in a statistically significant improvement in the rate of healing compared to wet-to-dry dressings.2
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in Appendix 2.
Also Check: Can You Drink Beer With Ulcerative Colitis