Bedsores Caused By Neglect
Bedsores are also called pressure sores because they are usually caused by prolonged pressure on a specific area of the body. Other factors that can put nursing home residents at risk are malnutrition, , and excessive friction on the skin. These causes are almost always preventable and in some cases are signs of serious neglect or abuse.
Many stage 2 bedsores could have been prevented with better care, more movement, or more frequent skin checks. Sometimes nursing homes fail to notice stage 1 sores or improperly treat them, allowing them to develop into stage 2 sores.
Families trust nursing homes to properly care for their loved ones. A nursing home is responsible for keeping their residents safe, healthy, and happy. Caretakers in nursing homes should monitor the nutrition, hydration, and skin health of their residents.
You may need to take legal action if you believe your loved ones bedsores were caused by neglect or abuse at a nursing home. If your loved one is not receiving proper care at their nursing home, please contact us for a .
Navigate This Page
Identifying A Stage 2 Bedsore
Stage 2 bedsores can be identified as an intact blister or shallow open sore. These sores are often red or pink and surrounded by red and irritated skin. These sores may also be moist if pus or fluid is present.
Human skin is made up of layers. The topmost level is called the epidermis. A stage 2 sore has broken the epidermis to create an open wound. The second layer of skin, the dermis, is visible in stage 2. In some cases, the dermis is broken.
Stage 2 bedsores have broken the skin but have not broken past the dermis to fat. The deeper a sore goes, the more difficult it will be to treat and the longer it will take to heal. People who are at risk of developing bedsores should receive regular skin checks to identify bedsores before they progress past stage 2.
Signs of a stage 2 bedsore include:
- Intact or ruptured blister
- Pus or fluid
- Redness or discoloration
Identifying a stage 2 sore as soon as possible is imperative. Complications can occur when bedsores go unnoticed and untreated. In serious situations, bedsores can become life-threatening or lead to amputation. If a sore becomes infected, the infection can spread to the blood, heart, or bones.
Notify a doctor or other healthcare provider if you or a loved one has developed a stage 2 bedsore. A health professional can decide the best plan of action to treat the bedsore properly.
Who’s Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 older people are more likely to have mobility problems and skin that’s more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body
- medical conditions that affect blood supply, make skin more fragile or cause movement problems such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis and Parkinson’s disease
Also Check: Ulcerative Colitis Abdominal Pain Relief
Symptoms Of Stage 2 Pressure Ulcers
Stage 2 pressure ulcers are shallow with a reddish base. Adipose and deeper tissues are not visible, granulation tissue, slough and eschar are not present. Intact or partially ruptured blisters that are a result of pressure can also be considered stage 2 pressure ulcers. Note that causes of erosion, ulceration, or blistering that aren’t a result of pressure are not included in the definition of a stage 2 ulcer.
The Four Stages Of Pressure Injuries
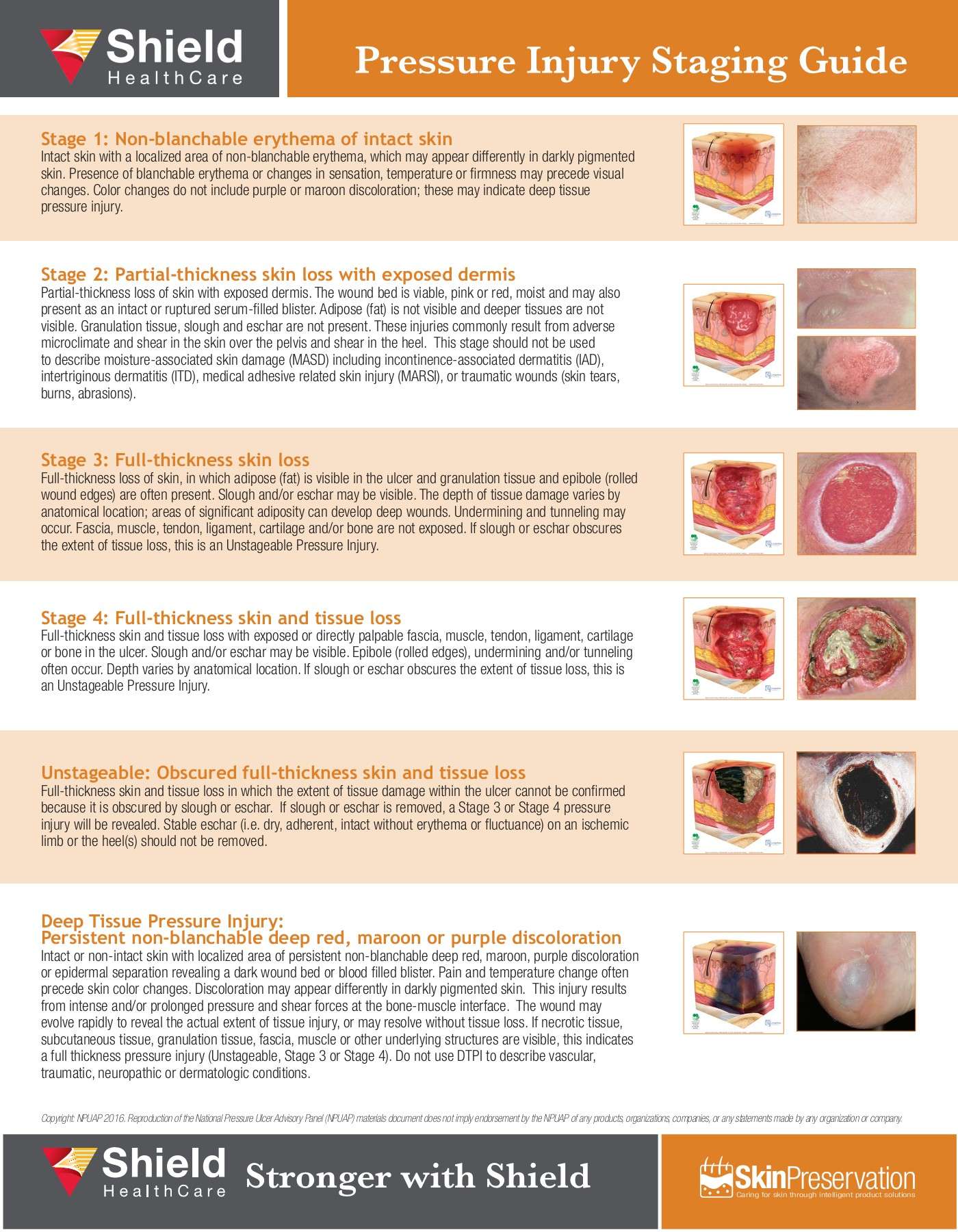
We know pressure injuries are dangerous for our patients and costly for our medical system, so the question becomes, how can we recognize them in order to guard against them? Pressure injuries are broken into four stages, where the stage indicates the extent of tissue damage. Following are the key indicators for each stage.
Recommended Reading: Ulcerative Colitis And Lung Disease
What Are The Characteristics Of Each Stage Of Pressure Ulcer
By Nursing Home Law Center
Of course, no one ever enters a medical facility expecting to get sicker. Unfortunately, thousands of people who enter nursing homes and hospitals every year for medical treatment or rehabilitative care wind up developing a complication that is more painful and enduring than they ever could have imagined the development of a pressure ulcer.
Pressure ulcers are wounds that frequently develop on bony areas of the body where there is little tissue to distribute the pressure from the surface that they are sitting or laying on over extended periods. For this reason, the most common areas of the body where pressure ulcers develop are: hips, elbows, heels and the area of the lower back known as the coccyx.
The medical community has embraced a staging system to grade pressure ulcers as they progress. The four stage scaling system uses identifiable characteristics present in various types of wounds to help professionals in the treatment of the pressure ulcers as well.
The National Pressure Ulcer Advisory Panel has devised the most widely accepted pressure ulcer staging scale. Below are the guidelines as proposed by NPUAP:
Given the severity of pressure ulcer progression and ensuing complications, it is imperative that staff at medical facilities identify and begin a course of treatment as soon as there is evidence of a pressure ulcer in order to avoid the dibilitiating complications that typically accompany this condition.
Related Information
Pressure Ulcer Prevalence Varied By Age Sex And Length Of Time Since Admission To The Nursing Home But Not By Race
Residents aged 64 years and under were more likely than older residents to have pressure ulcers . Pressure ulcers were more common in males than in females . Residents in nursing homes for 1 year or less were more likely to have pressure ulcers than those with a longer length of stay . There was no significant difference between white and nonwhite populations with respect to having pressure ulcers.
You May Like: Dog Skin Ulcer Home Treatment
What Causes Pressure Injuries
There are many contributing factors for pressure injuries. At the most basic level, they result from three primary factors:
- Sustained pressure. When skin and underlying tissue experience prolonged contact against a surface, the pressure may lead to insufficient oxygenation and damaged cells. This happens most often to areas that lack sufficient padding from muscle or fat, like heels, hips, shoulder blades, elbows, and the tailbone.
- Friction. Friction occurs when skin is dragged across a surface. For instance, when a patient changes position or a care provider moves them. Friction is exacerbated when skin is moist.
- Shear. Shear occurs when two surfaces move in opposite directions for example, when a hospital bed is elevated, a patient may slide down, pulling bones and skin in different directions.
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Recommended Reading: What Medicine Is Best For Stomach Ulcers
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Unstageable Pressure Injury: Obscured Full
Unstageable pressure injuries occur when the extent of tissue damage within the ulcer cannot be ascertained because it is obscured by eschar for example. However, if the eschar is removed, a stage 3 or stage 4 pressure injury will present. In these instances, the NPUAP advises that âstable eschar on the heel or ischemic limb should not be softened or removed.â
Recommended Reading: What Is The Best Treatment For Ulcerative Proctitis
Failure Of Reactive Hyperaemia Cycle
It is a known fact that tissue distortion causes ischaemia that in turn stimulates protective movements to relieve pressure and circulatory activity to restore normal blood flow in the affected areas. These protective movements are often reflexes as the person is unaware of making them. However, if these prompt actions prove insufficient to relieve ischaemia, the central nervous system is stimulated by constant signals of discomfort and pain to make sure that the pressure is relieved before any permanent damage occurs. Once the pressure is relieved, and the circulation restored, local capillaries begin to dilate and increased blood flow takes place, referred to as reactive hyperaemia. As a result, a bright pink transitory patch appears on the skin, often called blanching erythema because it blanches on pressure unlike the dull red non-blanching erythema that indicates tissue damage . Reactive hyperaemia ensures a rapid restoration of oxygen and carbon dioxide balance it also flushes out waste products. Erythema subsides as soon as tissues are restored to their resting state.
Various grading of pressure ulcer . A very severe trochanteric pressure ulcer where destruction is so severe that the femoral head dislocated and came out
Treatment Of Stage 2 Pressure Ulcers

The goal of care for stage 2 pressure ulcers is to cover, protect, and clean the area. As always, on the area is key to wound healing. With quick attention, a stage 2 pressure ulcer can heal very rapidly. Emphasis should be placed on proper nutrition and hydration to support wound healing. Generally, pressure ulcers that develop beyond stage 2 are considered to be a result of lack of aggressive intervention.
The following precautions can help minimize the risk of developing pressure ulcers injuries in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individuals level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
- Use positioning devices to prevent prolonged pressure bony prominences.
- Keep the head of the bed as low as possible to reduce risk of shearing.
- Keep sheets dry and wrinkle free.
Recommended Reading: Does Turmeric Help Ulcerative Colitis
Treating Stage 2 Bedsores
Treatments for stage 2 bedsores are usually similar to the treatments for . The most important steps for treating bedsores are to identify the cause of the sore and to eliminate that cause.
For example, bedsores are usually caused by pressure on a specific area of skin. This occurs with a lack of movement, often due to age or a health condition. A sore that has progressed to stage 2 can be aided by reducing or eliminating the pressure on that area.
Treatments for stage 2 bedsores include:
- Removing all pressure from the area
- Keeping the area clean and dry
- Maintaining a nutritious diet high in protein, vitamins and minerals
- Staying properly hydrated
- Finding and eliminating the cause
- Inspecting the area as often as possible, at least twice a day
Nursing home attendants should help patients with bedsores to move to new positions regularly. They can also relieve the pressure by propping up parts of a patients body with pillows or switching the patients bedding or mattresses. Some bedding products are made to specifically to relieve pressure.
Cleaning a stage 2 bedsore is another important step to treatment. Stage 2 bedsores should be cleaned with saltwater or another doctor-approved cleaner and then kept dry. The cleaning process will help remove loose, damaged, and dead tissue, this is called debridement. In some cases, a doctor will recommend surgical debridement.
Nursing Home Abuse & Neglect Resources
Common Cases:
Client Reviews
Nursing Home Law Center, LLC is not a law firm. It is an organization that concentrates solely on helping provide nursing home patients and their families the legal help they need. NHLC LLC has a network of recognized attorneys located across the country who have experience representing clients in all types of nursing home injury cases. References to “NHLC attorneys” or “our attorneys” are references to attorneys within NHLC’s network, and not employees, agents, or partners of NHLC. Please consult the disclaimer page for further information concerning NHLC. All information on this site shall be considered ‘attorney advertising’ and not construed as legal advice. Prior case results should not be relied on when retaining a lawyer.
Don’t Miss: Diet Plan For Ulcerative Colitis Flare Up
Stage 1 Pressure Injury: Non
In stage 1 pressure injuries the skin is still intact with a localized area of redness that does not turn white when pressure is applied . Stage 1 does not include purple or maroon discoloration these may indicate deep tissue pressure injury. For visual reference, see illustrations of pressure injuries from the NPUAP here.
The Available Reconstructive Options Are
Split thickness skin grafting
When the ulcer is superficial and vital tissues such as bone, vessels, nerves or tendons are not exposed, and the ulcer is not copiously discharging, skin grafting is the first option for surgical treatment. The slimy layer over the surface of ulcer is sharply debrided to get a healthy vascular bed for skin grafting.
Local flaps
Variety of local flaps can be used to reconstruct the defect created by excision of pressure ulcers. Local transposition, rotation, limberg flap are the available options .3]. Biceps femoris V-Y advancement for ischial pressure sore and perforator based V-Y advancement is another good options if the anatomy permits .
Sacral pressure sore , debridement and cover by local perforator based V-Y advancement flaps , 1-month post-operative , recurrence on the flap after 11 years due to loss of family support and subsequent improper care. Another patient with the same flap after 16-year of follow-up with a proper weight shifting and care showing stable coverage
Regional flaps
Medial planter flap for heel sore: A long-standing deep trophic ulcer of heel . The islanded medial planter flap was transposed to the defect and the resultant donor site was covered by split thickness skin graft . The 1-week and 3-month post-operative pictures showing stable coverage. Patient allowed full weight bearing from 6th week along with silicone footpad protection
Microvascular free flaps
Also Check: How To Prevent Skin Ulcers
Prevention: Mattresses And Cushions
Protection is the best way to prevent ulcers. Patients who are at risk of developing pressure ulcers should have the skin carefully inspected for any damage or redness twice daily. The skin should be kept clean and dry. Any pressure causing damage to skin or tissue should be immediately eliminated. This can be done with the help of special mattresses, cushions and by many protective devices that can relieve the external pressure on vulnerable areas of body limbs. These specially designed protective devices can be very helpful in patients who thought to be at risk of developing pressure ulcers, or who have pre-existing Grade 1 or 2 pressure ulcers. Classified by their static or dynamic nature, many advanced low tech and high tech support surfaces and overlays are available for patients bound to lie on bed for long periods of time. Static surfaces do not require electrical power, while dynamic surfaces require electrical power for shifting and redistributing the pressure within the surface. Other integrated electronic beds like air fluidised beds and electronic moving air mattresses require high technology and heavy machinery to let air and ceramic sphere particles support the object on a stream mechanically are often costly, noisy and not easily available. Due to lack of substantial evidences and researches, it is difficult to firmly conclude about relative effects of support surfaces.