Olive Oil Coconut Oil Omega
Fat is an important component of a balanced diet. A good quality olive oil is best for sautéing over low heat and making cold dressings or sauces.
Coconut oil is worth trying, especially if you have a difficult time digesting fat. As a medium-chain triglyceride, its more easily and more completely digested without the help of bile salts than other plant oils. For that reason, it can be a good oil for people with malnutrition and malaborption problems.
Coconut is solid at room temperature, so it is versatile and can be used like butter for both sautéing over high heat and for baking.
Omega-3 fats are important because we cannot make them in our body. They are found in nuts, avocadoes, freshly ground flaxseed, and fish. Wild salmon and sardines are preferable to other fish as a source of omega-3s because of their low heavy metal content.
Artificial trans fats should be avoided altogether because it increases the risk of developing heart disease. Trans fat is used to make crackers, cookies, and other processed food because it extends the shelf life.
Can Food Cure Crohns Or Colitis
You may come across diets that claim to cure Crohns or Colitis, but there isnt any evidence to prove that these work. A healthy, balanced diet will give you nutrients that are important to help you stay well.Some people find that making small changes to their diet, for example avoiding spicy food, helps them cope with their symptoms. If cutting out a food makes no difference to your symptoms, make sure you start eating it again to avoid missing out on important nutrients.There are times when your IBD team or dietitian may advise you to change your diet, for example, after surgery or if you have a narrowing in your small intestine, called a stricture. Some people, such as children or people with Crohns, may benefit from a liquid diet, called exclusive enteral nutrition.Always speak to your GP or a dietitian before making any big changes to your diet.
Ive tried just about all the different diets for Ulcerative Colitis and just gone round in a complete circle, not finding any success, only causing problems and stress! I now realise the most important thing is to eat a balanced diet and enjoy my food!
Trevor
Eating In Periods Of Remission
If youre in remission and your symptoms are light or even gone, give yourself the best chance at maintain that state by continuing to eat a nutritious and diverse diet. Consider the food you eat as the most powerful of medicines!
With all ulcerative colitis diets, we need to be sure work new foods in very slowly. Stay hydrated. Talk to your nutritionist, dietitian or healthcare professional before making any drastic changes to your diet, and of course, remember to keep up with your food journal.
These are examples of foods that may help you stay healthy, hydrated and in remission:
Read Also: Triderma Diabetic Ulcer Defense Healing Cream
Tips For Preparing Nutritious Foods For Uc
Its one thing to know which foods are nutritious for you, but another to safely consume them. As one MyCrohnsAndColitisTeam member put it, The hard part is getting your nutritional requirements in with limited choices. Practicing meal planning and preparation techniques can be helpful to ensure adequate nutrition.
Members often share creative ways theyve found to incorporate nutritious foods into their diet safely. I made some pureed green sauce with greens, anchovies, garlic, and EVOO to add to roasted veggies and soups, said one. I have a Nutri Ninja. It purees my fruits and veggies, so I eat lots of smoothies with almond milk and Activia yogurt added, shared another.
It may also be helpful to purchase meal replacements, such as protein shakes, to keep your weight up. One member had a tip for weight gain: I increase the recipes that use lots of natural fats olive oil, coconut oil, coconut cream, avocado and I might increase my red meat. All of those make me feel super healthy.
Who Gets Ulcerative Colitis And Why

UC like all other health conditions is caused by various underlying factors including unresolved infections, toxins, nutritional deficiencies and emotional patterns.
Ulcerative colitis is an inflammatory bowel disease that occurs mostly in developed nations, and is more common in urban centers where the Western diet pattern dominates. It is estimated that approximately 1 million people in the U.S. alone suffering from the disease and its many gastrointestinal symptoms.
As a chronic illness, UC can be active at times and inactive at other times. If the symptoms are mild, they do not make the body burn out. The unpredictable nature of ulcerative colitis makes diagnosis very challenging.
The disease may start at any age, but individuals with the disease usually develop it between 15 and 25.
It seems that there is a genetic component to ulcerative colitis because individuals of eastern European Jewish lineage have a great risk of ulcerative colitis. While the cause is still unknown, research has hinted at a connection to irregular reactions to bacteria in the colon. Evidence does not indicate that ones diet is the cause of ulcerative colitis.
To diagnose ulcerative colitis a colonoscopy is usually ordered, during which an endoscope is passed through the anus and into the colon. While ulcerative colitis can be diagnosed by X-rays of a barium-filled colon, colonoscopy should be used because they are more sensitive and allow for biopsies to be taken of the lining of the colon.
Also Check: What Not To Eat If You Have An Ulcer
What Advice Is There For When I Have No Active Disease
When you are in remission then it is essential to make sure you are well nourished and regain any lost weight you may have experienced during a flare. Good nutritional status also helps to prevent vitamin and mineral deficiency and infection, and maintain disease remission.
- Base meals on higher fibre starchy foods like potatoes, bread, rice or pasta.
- Have some dairy or dairy alternatives .
- Eat some beans, pulses, fish, eggs, meat and other protein.
- Choose unsaturated oils and spreads, and eat them in small amounts.
- Drink plenty of fluids .
Can You Eat White Bread With Ulcerative Colitis
Low-residue diet
Temporarily eating a low-residue or low-fibre diet can sometimes help improve symptoms of ulcerative colitis during a flare-up. These diets are designed to reduce the amount and frequency of the stools you pass. Examples of foods that can be eaten as part of a low-residue diet include: white bread.
Recommended Reading: Nutritionist Specializing In Ulcerative Colitis
Don’t Miss: Is Ulcerative Colitis An Inflammatory Bowel Disease
The Nutritional Impact Of Uc
Changes in diet and nutrition are one part of a multifaceted approach for treating ulcerative colitis and other IBD conditions. Your doctor also will likely prescribe medication. In more severe cases, surgery may be needed, to repair or remove damaged portions of the colon.
Malnutrition, dehydration, and weight loss are major health risks of UC. When the colon becomes inflamed and ulcerated, its less able to absorb fluids and nutrients needed to help sustain your body.
Diarrhea, a symptom of UC, also increases loss of fluids and nutrients, such as sodium, potassium, magnesium, phosphorus, and zinc.
In severe cases, people with UC may need IV fluids to replace these lost nutrients and fluids.
Other UC symptoms, such as abdominal pain and nausea, can further rob you of nutrition as they reduce your appetite, so you consume fewer calories and nutrients.
Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs they typically develop over time. Most people experience mild to moderate symptoms, but the course of ulcerative colitis may vary and some people have long periods of remission. The symptoms depend on the location of the disease-causing inflammation. If you have ulcerative colitis, you may have the following signs and symptoms:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- An increased risk of blood clots in veins and arteries
You May Like: Ulcerative Colitis Weakness And Fatigue
Nutritions Role In Treating Uc
Your health care provider can help you make up for these nutritional deficits by identifying foods to help control your UC symptoms and provide you a well-balanced, nutritious diet.
Certain foods or beverages may irritate your digestive tract and trigger flare ups of UC symptoms. Your health care provider will help you identify these foods, so you can avoid them and identify substitute foods that provide the same nutrients, without flare ups.
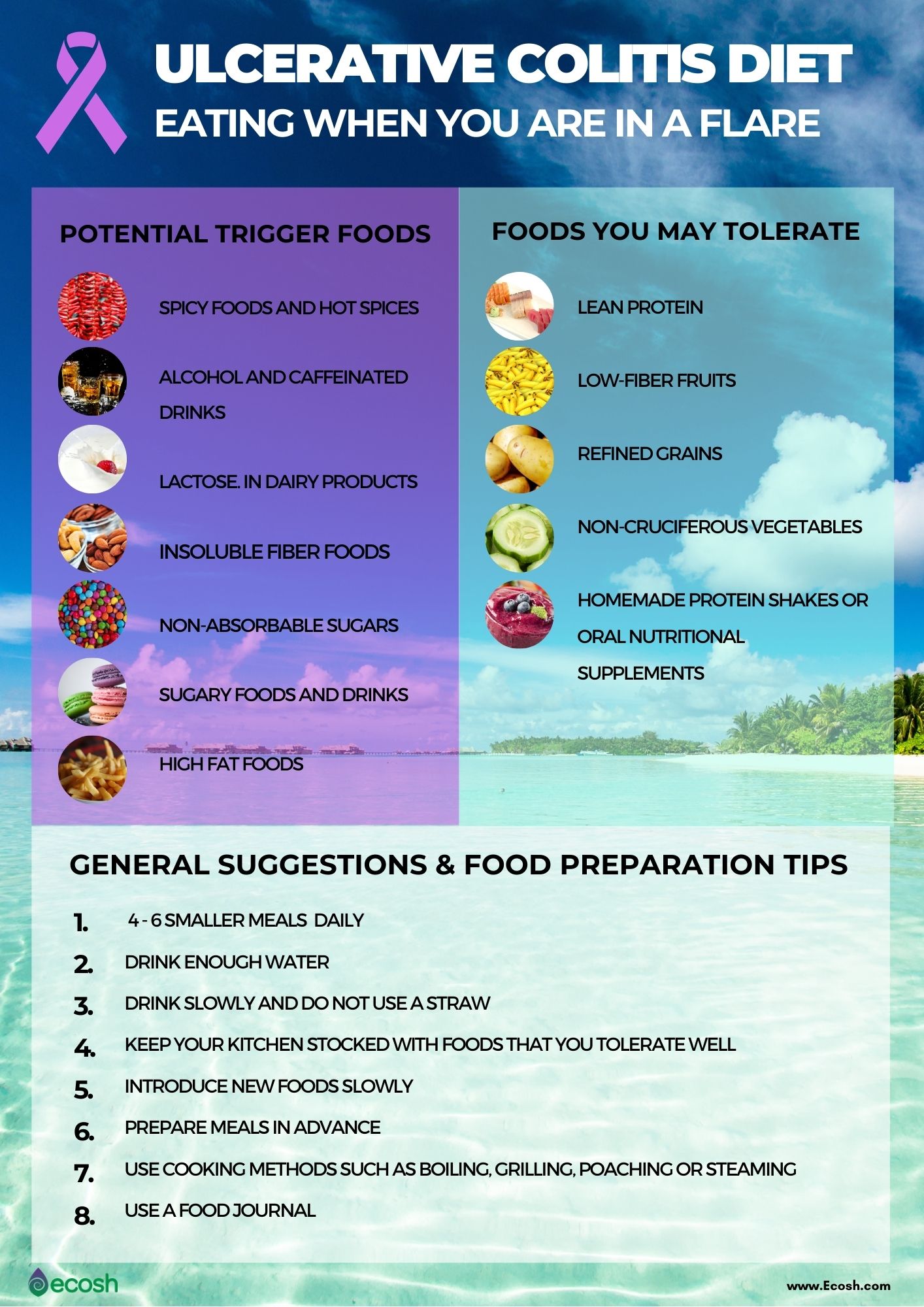
Foods more likely to trigger UC symptoms include:
-
Plant foods that contain insoluble fiber, such as fruits with skin or seeds raw green vegetables, especially cruciferous vegetables, such as broccoli or cauliflower whole nuts or whole grains and anything with a peel
-
Lactose, a sugar in dairy products, such as milk, cream, and soft cheeses
-
Sugary foods such as pastries and juices
-
Non-absorbable sugars: sugar alcohols found in sugar-free gum, candy, ice cream, and certain types of fruits/juices such as pear, peach, and prune
-
High-fat foods, including fried or greasy foods, butter, coconut, margarine, and cream
-
Alcohol
Recommended foods for UC include:
-
Refined grains, such as sourdough, potato, or gluten-free bread, white pasta, white rice, and oatmeal
Your health care provider may also recommend:
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Read Also: How To Prevent Decubitus Ulcers
Foods That May Help Avoid Flares
Some healthful foods may have anti-inflammatory effects that can help control the underlying inflammation of Crohns disease and ulcerative colitis. Many of these foods are unprocessed. They also tend to have lots of color. Some of the substances that give fruits and vegetables their color have anti-inflammatory and other healthful effects.
Eating this way helps support anti-inflammatory pathways in our bodies, which may be very helpful when managing an inflammatory disease like IBD. In addition, if you are not flaring, eating healthful foods will also help you avoid any deficiencies in vitamins, minerals, and other nutrients.
Ulcerative Colitis Vs Crohns Disease
Crohns Disease is another inflammatory bowel disease that shares similarities to ulcerative colitis, with a few key differences. The first is that Crohns disease can technically occur along the entire length of the GI tract, as opposed to ulcerative colitis occurring exclusively in the colon. Crohns disease also presents in discontinuous patches as opposed to the continuous diseased areas in ulcerative colitis. Imbalances in gut bacteria tend to be more pronounced in Crohns disease than ulcerative colitis. Finally, the inflammation in ulcerative colitis typically does not go as deeply into the gut tissue layers as in Crohns disease, but both diseases show evidence of gut barrier dysfunction, or leaky gut.
Don’t Miss: Nutritionist Specializing In Ulcerative Colitis
How A Professional Can Help
Living with ulcerative colitis can be frustrating, and its better if you dont have to go at it alone. Working with a gastroenterologist and a registered dietitian can help. Medications can ease symptoms, and diet changes can help to control flares. Its especially important to include a registered dietitian if youre trying an elimination diet since they will work with you to prevent any nutritional deficiencies.
Since everyone with UC has different triggers, figuring out what works best for youand the trial and error that goes along with itwill be much easier with the help of health professionals.
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Recommended Reading: How To Treat An Ulcer After Gastric Bypass
Dietary Changes To Help Reduce Ulcerative Colitis Symptoms
Since ulcerative colitis , a condition that causes inflammation in the colon and rectum, is never medically cured, certain lifestyle behaviors can help you manage symptoms and better cope with your condition. In addition to managing stress, paying attention to what you eat can have a big impact on your quality of life.
There is no single diet that works best for managing UC. In fact, no studies have shown that any specific diet improves symptoms or that any specific foods cause UC flare-ups. The best approach is to avoid or reduce the foods that aggravate your symptoms.
You should eat a well-balanced, healthy diet rich in fresh fruits and vegetables, such as a Mediterranean style diet. Avoid preservatives and emulsifiers, such as carrageenan, carboxymethylcellulose, and polysorbate-80.
Having a nutritionist design a specialized diet plan for you may be helpful. The nutritionist will first want to identify foods that may trigger flare-ups or make your symptoms worse.
There is no strong evidence that following any particular specialized diet dietsuch as low-carb, vegetarian, or paleohas any effect on keeping UC in remission.
- disaccharides, such as lactose
- monosaccharides, such as fructose
- oligosaccharides, such as fructans and galactans
- polyols, such as sorbitol and mannitol .
Speak with your doctor about whether adding more probiotics to your diet might help you.
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Recommended Reading: How Do You Get Rid Of Leg Ulcers
Do Patients Living With Ulcerative Colitis Adhere To Healthy Eating Guidelines A Cross
Published online by Cambridge University Press: 24 September 2014
- Michelle Walton
- Affiliation:Department of Sport, Health and Nutrition, Leeds Trinity University, Brownberrie Lane, Horsforth, Leeds LS18 5HD, UK
- Ieva Alaunyte*
- School of Health Sciences, Liverpool Hope University, Hope Park, Liverpool L16 9JD, UK
- *
How To Calculate The Pucai Score
The PUCAI score ranges from 0 to 85 and is defined as:
- Remission : less than 10
- Mild: 10-34
- Predict the course of the disease over time
- Know when to recommend other treatments in severe cases
Experts recommend that doctors check a childâs PUCAI score during every visit and reevaluate treatment if their score is above 10.
You May Like: What Foods Are Good To Eat With Ulcerative Colitis
What Causes Ulcerative Colitis
The cause of ulcerative colitis is unknown but it is believed to be caused by a combination of several factors including an overactive immune system, genetics, and the environment.
- Overactive immune system: It is believed that in ulcerative colitis, the immune system is triggered to mistakenly attack the inner lining of the large intestine, causing inflammation and symptoms of ulcerative colitis.
- Genetics: Ulcerative colitiscan run in families. The genetic link is not entirely clear but studies show that up to 20% of people with ulcerative colitis have a close family member with the disease.
- Environment: Certain environmental factors including taking certain medications , and eating a high fat diet may slightly increase the risk of developing ulcerative colitis.
Physical or emotional stress, and certain foods do not cause ulcerative colitis, however, they may trigger symptoms in a person who has ulcerative colitis.