What Are The Prescription Medications For Uc
Medication for UC is designed to suppress your immune systems abnormal inflammatory responsewhich is causing symptoms. When inflammation is suppressed, it offers relief from common symptoms .
There are 5 main categories of medications used to treat inflammatory bowel disease like UC.
Given either orally or rectally, these drugs work to decrease inflammation in the lining of the intestines and are usually used to treat mild to moderate UC symptoms. Sulfasalazine and mesalamine are examples of 5-ASA medications.
Metronidazole, ciprofloxacin, and other antibiotics may be used when infections occur, or to treat complications of ulcerative colitis.
These suppress the immune system to reduce inflammation by targeting a specific pathway. Certain biologics work by targeting specific inflammatory proteins that play a role in inflammation called cytokines. Others work by preventing certain white blood cells from getting into inflamed tissues.
Prednisone, prednisolone, and budesonide are included in this type of medication. They affect the bodys ability to initiate and maintain an inflammatory processkeeping the immune system in check. While effective for short-term flare-ups, theyre not recommended for long-term use.
These modify the bodys immune system activity to stop it from causing ongoing inflammation. These drugs , and methotrexate) are usually used to maintain remission or for people who have only responded to steroids.
Types Of Ulcerative Colitis:
Let the names help you, so you can understand where the ulcerative colitis is located:
Ulcerative proctitis : affects the rectum and is the most mild form of all types. It tends to have fewer complications due to being located just in the rectum.
Proctosigmoiditis: PROCT: COLON and SIGMOID: SIGMOID COLON and ITIS: inflammationinflammation of the rectum and sigmoid colon.
Pancolitis . It is a very severe form of ulcerative colitis.
Left-sided colitis: LEFT-SIDED: includes the descending colon, sigmoid colon, and rectum and ITIS: inflammation.inflammation of the descending, sigmoid, and rectum.
Nclex Review For Ulcerative Colitis
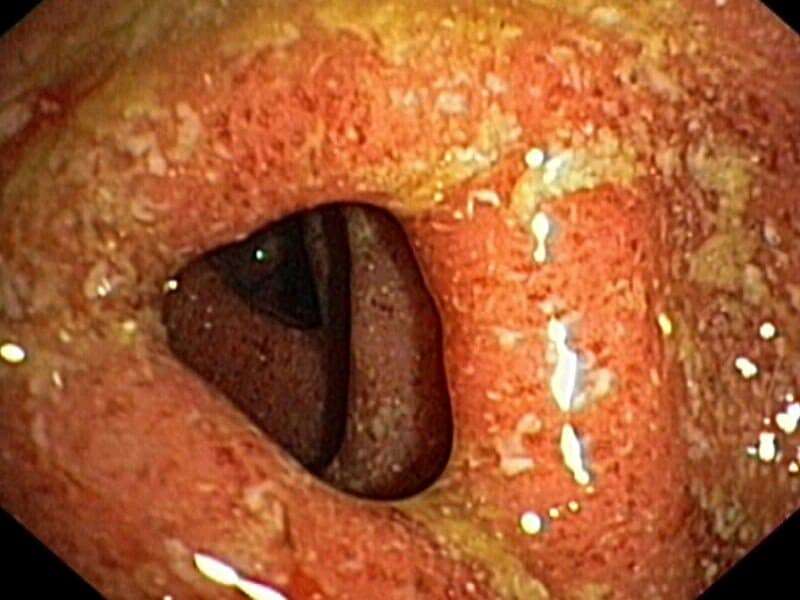
What is Ulcerative Colitis? It is one of the two types of inflammatory bowel diseases that causes inflammation and ulcers in the inner lining of the COLON and RECTUM .
Important take away: Remember it affects the COLON/RECTUM and INNER LINING only. It is different from Crohns Disease that can affect any part of the GI tract and the whole bowel wall.
Key Points:
- No cure managed with diet and medications
- Happens over time or suddenly
- Tends to start in the rectum and over time moves throughout the large intestine in a uniform fashion
- Patient will experience periods of flare-ups and remission
- Cause is unknown at this time but seems to be autoimmune that is triggered by the following:
- Environment
- Genetic factors make more susceptible
You May Like: Best Feed For Ulcer Prone Horses
True Stories: Living With Ulcerative Colitis
Ulcerative colitis affects about 900,000 people in the United States. In any single year, about 20 percent of these people have moderate disease activity and 1 to 2 percent have severe disease activity, according to the Crohns and Colitis Foundation of America.
Its an unpredictable disease. Symptoms tend to come and go, and sometimes they progress over time. Some patients go for years without symptoms, while others experience frequent flare-ups. Symptoms vary depending on the extent of the inflammation, as well. Because of this, its important for people with UC to keep track of how it affects them on an ongoing basis.
Here are the stories of four peoples experiences with UC.
years ago.
How do you manage your symptoms?
My first treatment was with suppositories, which I found extremely uncomfortable, hard to put in, and hard to hold. For the next year and a half or so I was treated with rounds of prednisone and mesalamine . This was awful. I had terrible ups and downs with prednisone, and every time I started to feel better I would feel sick again. I finally switched doctors to Dr. Picha Moolsintong in St. Louis, who actually listened to me and treated my case and not just my disease. I am still on azathioprine and escitalopram , which have been working very well.
What other treatments have worked for you?
What advice would you give to other people with UC?
How long ago were you diagnosed?
How difficult has it been to live with UC?
What helped you?
Inflammatory Bowel Disease Nursing Care Plans
Inflammatory bowel disease is an idiopathic disease caused by a dysregulated immune response to host intestinal microflora. It results from a complex interplay between genetic and environmental factors. Similarities involve chronic inflammation of the alimentary tract and periods of remission interspersed with episodes of acute inflammation. There is a genetic predisposition for IBD, and patients with this condition are more prone to the development of malignancy.
The two major types of inflammatory bowel disease are ulcerative colitis and Crohn disease .
Ulcerative colitis : A chronic condition of unknown cause usually starting in the rectum and distal portions of the colon and possibly spreading upward to involve the sigmoid and descending colon or the entire colon. It is usually intermittent , but some individuals have continuous symptoms. Cure is effected only by total removal of colon and rectum/rectal mucosa.
Regional enteritis : May be found in portions of the alimentary tract from the mouth to the anus but is most commonly found in the small intestine . It is a slowly progressive chronic disease of unknown cause with intermittent acute episodes and no known cure. UC and regional enteritis share common symptoms but differ in the segment and layer of intestine involved and the degree of severity and complications. Therefore, separate databases are provided.
Read Also: Stage 2 Pressure Ulcer Treatment Cream
What Other Conditions Are Related To Ulcerative Colitis
Ulcerative colitis is a type of inflammatory bowel disease , but its not the same as irritable bowel syndrome .
Although the disorders share some of the same symptoms, such as abdominal pain and diarrhea, inflammation and ulcers do not occur with IBS.
Another disease often mentioned alongside ulcerative colitis is Crohns disease. Ulcerative colitis and Crohns are different types of IBDs that affect the digestive tract in different ways.
There are some common symptoms between the two conditions, but the overall pattern of symptoms tends to be different for each.
While diarrhea and rectal bleeding are more common in ulcerative colitis, Crohns disease more often causes severe abdominal pain, nausea, weight loss, and vomiting.
Ulcerative colitis is limited to the lining of the large intestine , whereas Crohns disease can affect the entire digestive tract from your mouth to your anus and isnt limited to the inner part of the intestines.
Learn More About the Differences Between UC and Crohns
Dont Miss: How Can Ulcers Be Treated
What Do Ibd Nurse Specialists Do
Within the multidisciplinary team operates a small team of IBD Nurse Specialists. They have extensive training and experience in gastroenterology and are especially interested in treating and supporting patients with IBD.
IBD Nurse Specialists can conduct both face-to-face and telephone clinics, provide advice on how to manage the condition and refer patients to other relevant specialists within the team.
You May Like: Is Oatmeal Good For Ulcerative Colitis
Cohen R D Yu A P Wu E Q Xie J Mulani P M And Chao J
Systematic review: the costs of ulcerative colitis in Western countries
2010 – Alimentary Pharmacology & Therapeutics
In-text:
Your Bibliography: COHEN, R., YU, A., WU, E., XIE, J., MULANI, P. and CHAO, J., 2010. Systematic review: the costs of ulcerative colitis in Western countries. Alimentary Pharmacology & Therapeutics, 31, pp.693-707.
Do A Little Research Before Leaving Home
When someone has UC, the last thing you want to do is wing it. To help ease your loved ones concerns about going out whether its a short trip to the grocery store or an outing to a park scout out the locations of bathrooms at your destination. Make sure they have a clear path to the bathroom, says Hanauer.
If youre going to a restaurant, you can also scan the menu ahead of time to make sure there will be dishes that are good choices for someone with UC.
Read Also: How To Repair An Ulcer
Deterrence And Patient Education
American College of Gastroenterology has made guidelines on preventive care in patients with ulcerative colitis. These recommendations include:
- Screening for skin malignancies irrespective of the use of biological agents
- Assessing bone mineral density
- Be vaccinated against herpes zoster
- Vaccinated against pneumococcus, H. influenzae, and the flu virus
- Should not travel to areas of yellow fever without first consulting with an infectious disease expert
- Be screened for depression and anxiety
- Women with ulcerative colitis should get annual cervical cancer screening
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Also Check: How To Stop An Ulcerative Colitis Flare
Read Also: Pepto Bismol And Ulcerative Colitis
Ibd Research And Clinical Trials
The University of Michigan Inflammatory Bowel Disease Center is nationally recognized for clinical and laboratory research. The majority of our referrals are patients who have already tried the treatment options available for IBD and are looking for the very newest therapies they cant get anywhere else. We have multiple open clinical trials investigating new therapies and diagnostics for Crohns disease and ulcerative colitis for those who qualify. Learn more at IBD Clinical Trials and Research.
Should I Stop Taking My Medicine
The short answer is, âNo.â If you stop taking your medicine because youâre worried about your immune system, your symptoms may flare. Some medicines take months to leave your system anyway. So stopping them now wouldnât change your risk of COVID-19 now. And you definitely donât want to have to go to a hospital now because of a flare.
It may be a good idea to avoid steroids if you can. But you shouldnât stop taking them suddenly. As a general rule, donât change any of your medications without first talking to your doctor.
Dont Miss: Is Ulcerative Colitis Considered An Autoimmune Disease
Also Check: Remicade Vs Entyvio For Ulcerative Colitis
More Than 200 Genes Identified
While no single underlying cause for IBD has been identified, genetics certainly play a role.
Jeffrey C. Barrett, Ph.D. who is a senior group leader from the Wellcome Trust Sanger Institute in Cambridge in the United Kingdom explains in an article published in the Journal of Autoimmunity that identical twins had nearly 10 times the rate of Crohns disease and nearly four times the rate of ulcerative colitis as non-identical twins.
This support the importance of genetics in IBD risk, he says. But it is not straightforward.
More than variations in the DNA code have now been linked to IBD, and this number is continuing to rise as molecular biology technology is becoming ever more sophisticated.
What are all these genetic data telling us about IBD?
Certain biological processes or pathways keep on cropping up. These include genes involved in the innate immune response including some genes responsible for keeping the lining of our gut intact as well as those involved in the activation and regulation of the adaptive immune response.
Perhaps these findings come as no surprise the classic hallmark of IBD is a dysregulated immune response. However, without detailed knowledge of how these pathways are disrupted, treatments will mostly focus on symptoms, rather than the underlying causes of the condition.
Yet genetics can only explain a proportion of the risk associated with developing IBD.
article in The Lancet thathighlights how IBD rates have evolved across the globe.
Feuerstein J D And Cheifetz A S
Ulcerative Colitis: Epidemiology, Diagnosis, and Management
2014 – Mayo Foundation for Medical Education and Research
In-text:
Your Bibliography: Feuerstein,, J. and Cheifetz,, A., 2014. Ulcerative Colitis: Epidemiology, Diagnosis, and Management. Mayo Foundation for Medical Education and Research, 89, pp.1553-1563.
Read Also: How To Stop Ulcers From Hurting
Living With The Unpredictability Of Ibd
May 19, 2021 | Mount Sinai Hospital, Sinai Health
Sabine Goldberg, 37 is a very busy mom. She is raising her energetic toddler, excelling at work and managing the unpredictability of living with IBD.
Inflammatory Bowel Disease is a group of disorders, including Crohns disease and ulcerative colitis that involve chronic inflammation of the gastrointestinal tract.
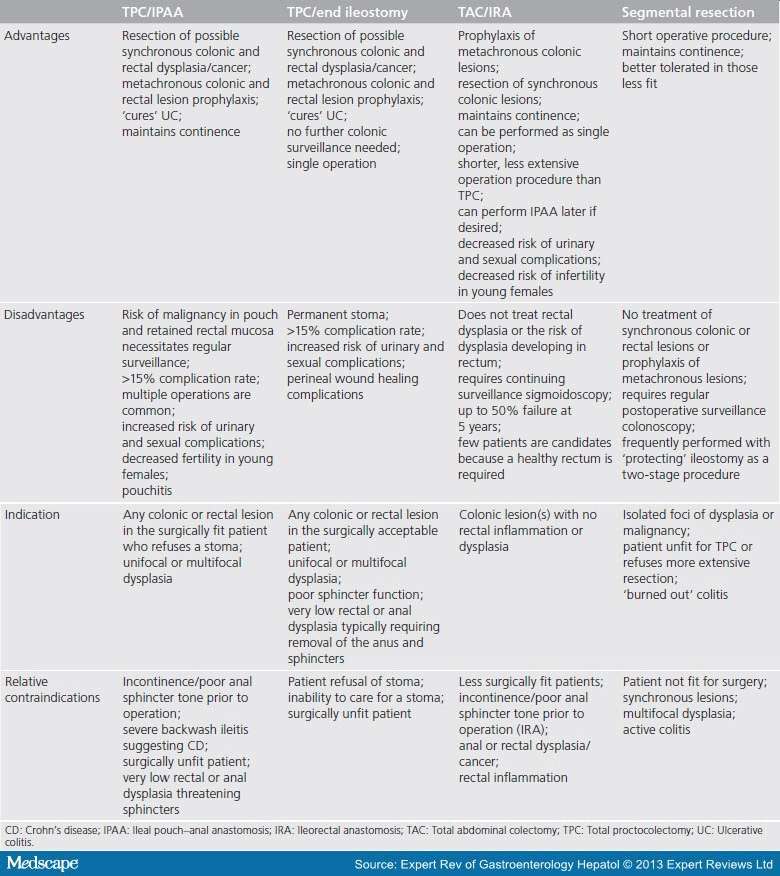
At age 16, an athlete playing basketball and soccer at the provincial level, Sabine was diagnosed with ulcerative colitis. Supported by a team of gastroenterologists at the Centre for Inflammatory Bowel Disease at Mount Sinai Hospital, she tried many medications that resulted in limited relief eventually undergoing surgery.
The programs interprofessional approach provided her with highly specialized surgery, and team-based care to include clinical nutrition, social work and psychosocial support. When she and her husband started thinking about family planning, she participated in a Pregnancy & IBD research initiative. Led by Dr. Vivian Huang, gastroenterologist at the Centre, the clinic collaborates with colleagues in the Womens and Infants Health program to optimize pre-conception care and manage IBD throughout pregnancy.
Expect That Uc May Change And Be Ready
The symptoms of UC can vary widely from person to person and can change over time in one individual. Some people have mild symptoms or long periods of remission, when their symptoms dont restrict their day-to-day activities, according to the Crohns and Colitis Foundation. During these times, you may not need to provide much support as a caregiver.
Other times, or in people with more severe disease, the symptoms can become distressing. Your loved one may experience:
- Frequent diarrhea
- Fatigue
- Weight loss
These symptoms can flare up seemingly out of nowhere and disappear just as quickly. When they occur frequently, your loved one may feel embarrassed, guilty, and even depressed. You can help by being prepared to extend more emotional support.
Read Also: What To Avoid Eating With Ulcerative Colitis
Work With Your Doctor To Understand Uc Severity
It’s important for you and your doctor to understand how severe your symptoms are. Beyond that, tests and procedures may be done to evaluate your disease activity and get an even better understanding of whats really happening inside your bodyand the inflammation thats occurringgetting you to the treatment plan thats right for you.
The Future What Needs To Be Done
In the future, developments in disease phenotyping and genotyping may help inform earlier intervention. A plethora of new and emerging therapeutic agents and interventions affected through differing mechanisms of action should also help improve future management of IBD. Improving patientphysician communication and supporting patients in their understanding of the evidence base are also important for ensuring patient commitment and involvement in the long-term management of their condition. There is also a desire to create more IBD centres of excellence and to develop IBD networks to ensure a consistent level of care across different settings working alone is no longer acceptable. Finally, improved communication may hold the key to empowering and allowing patients to actively participate in disease management.
Also Check: Ulcerative Colitis And Lactose Intolerance
Cholapranee A Hazlewood G Kaplan G Peyrin
Systematic review with meta-analysis: comparative efficacy of biologics for induction and maintenance of mucosal healing in Crohn’s Disease and Ulcerative Colitis controlled trials
2017 – AP & T
In-text:
Your Bibliography: Cholapranee, A., Hazlewood, G., Kaplan, G., Peyrin-Birovlet, L. and Ananthakrishnan, A., 2017. Systematic review with meta-analysis: comparative efficacy of biologics for induction and maintenance of mucosal healing in Crohn’s Disease and Ulcerative Colitis controlled trials. AP & T, 45, pp.1291-1302.
How Are Ulcerative Colitis And Crohn’s Disease Similar
- Both diseases often develop in teenagers and young adults although the disease can occur at any age
- Ulcerative colitis and Crohn’s disease affect men and women equally
- The symptoms of ulcerative colitis and Crohn’s disease are very similar
-
The causes of both UC and Crohn’s disease are not known and both diseases have similar types of contributing factors such as environmental, genetic and an inappropriate response by the body’s immune system
You May Like: Can You Take Imodium If You Have Ulcerative Colitis
Enhancing Healthcare Team Outcomes
Ulcerative colitis is a systemic disorder with no cure. The disorder has numerous extraintestinal involvement in addition to the colon. Thus, it is best managed by an interprofessional team. All patients with the disorder need lifelong monitoring. Because of the risk of colorectal cancer, surveillance colonoscopy should occur every 1-2 years. Further, since patients are often treated with biological agents, they need to undergo screening for melanoma and nonmelanoma skin cancer.
The pharmacists should assist the team by educating the patient on the importance of medication compliance to avoid relapse. The nurse should encourage regular vaccinations, hand washing, and cancer screening. A dietary consult should be obtained to educate the patient on foods to eat and what not to eat, especially if they have a stoma. In addition, a stoma nurse should be involved in the teaching of stoma care.
An infectious disease nurse should monitor the patient in the outpatient setting to ensure that they are not immunocompromised. Social workers should be involved to ensure that the patient has ample support and finances so that the treatments are not missed. Patients with risk factors for osteoporosis need screening for bone mineral density periodically. Patients should be encouraged to undergo annual vaccination against influenza and pneumococcus. Finally, many patients with ulcerative colitis develop depression and anxiety and should be referred to a mental health counselor.
Outcomes
Inflammatory Bowel Disease Conditions Require Long
Both Crohns disease and ulcerative colitis are conditions that fall under the umbrella term of Inflammatory Bowel Disease and both require management, and sometimes treatment, for a lifetime. However, with proper care from a facility that specializes in these diseases, you can expect to have a good quality of life. The University of Michigan Inflammatory Bowel Disease program is dedicated to the comprehensive medical and surgical treatment of adult patients with Crohns disease and ulcerative colitis. Our dedicated inflammatory bowel disease specialists exclusively treat IBD.
What you should know about Crohns and ulcerative colitis:
- Inflammatory Bowel Disease is an umbrella term that Crohns disease and ulcerative colitis fall under.
- Crohn’s disease and colitis are easily confused because both have similar symptoms and treatments, but also distinct differences. With a series of tests, your doctor can usually tell ulcerative colitis from Crohns disease however, in some cases the two diseases cant be distinguished from each other.
- The diseases affect men and women about equally.
- While the diseases can occur at any age, they often start between the ages of 15 and 25 and last a lifetime.
- Crohns disease is more common in people with a family history of the disease.
- Ulcerative colitis affects about 600,000 people in the U.S, while Crohns disease affects about 700,000 people.
Also Check: What Not To Eat With Bleeding Ulcers