Is Ulcerative Colitis Characterized By Symptoms
The intensity of the disease determines the symptoms. Some symptoms include diarrhea, frequent stools, and blood in the stool as well as an urge to defecate along with rectal pain and incontinence from time to time.
Severe cases can include weight loss, swelling of the legs, weariness, dyspnea, and fever as well as failure to grow in height. Stools that include blood are the most common symptom, however, diarrhea is not required.
What are the Consequences of Ignoring the Problem?
Without treatment, the person will continue to lose blood and become anemic as a result of the condition.
Diarrheaand diarrhea-related problems may occur. Uncontrolled diseases can lead to obstructions of the colon and even cancer. It can affect other organs.
There is a possibility that a person will get joint discomfort, liver illness, bone disease, skin disease, ulcers in the mouth, and even an elevated risk for developing blood clots in the body.
How Does Blood In The Stools Appear
According to the Canadian Institute of Intestinal Research, most people with UC experience varying levels of hematochezia, which refers to blood in the stools. The blood will usually be clearly visible in the stool â which has a semi-solid consistency â or on the surface. The blood color can range from bright red to maroon, with or without blood clots. This symptom often accompanies lower abdominal pain and the urgent need to defecate.
Blood from the rectum and large intestine is usually bright red. If blood is a darker color, it may be coming from higher up the gastrointestinal tract.
People with UC may have slow, steady bleeding when they do not have a bowel movement. They may also experience bloody diarrhea and constipation.
Some individuals with severe UC may notice blood in their stools more than 10 times a day.
People with UC will also usually have mucus in the stools but may not be able to see it. The mucus helps protect the inner lining of the intestines, as well as helping with bowel movements.
According to the Crohnâs and Colitis Foundation, people need immediate medical attention if they experience rectal bleeding with blood clots in stools.
Rectal Bleeding And Inflammatory Bowel Disease
One of the many symptoms of inflammatory bowel disease is bleeding. Blood might appear in or on the stool or some people may pass no stool at all at times, and just pass blood.
Bleeding from the rectum and large intestine from IBD is typically red or bright red, while blood coming from higher up in the digestive tract could appear as darker or black stools. In most cases this bleeding is slow and steady.
However, you should get emergency attention if:
- Bleeding is severe
- You’re vomiting blood
- You faint or feel like you’re going to
Blood in or on the stool can be frightening but it doesn’t always mean that there’s an emergency. It’s sometimes part of an IBD flare-up and it should be discussed with a physician as soon as possible, especially if it hasn’t happened in a while.
Bleeding means that there is some inflammation somewhere, and a change in treatment might be needed. Many treatments are available for IBD that can help stop the inflammation and the bleeding.
Don’t Miss: How Can You Tell If You Have An Ulcer
Bleeding In Crohn’s Disease
Crohn’s disease causes blood in the stool less commonly than does ulcerative colitis, but this will vary between patients based on where the Crohn’s is causing the inflammation.
Crohn’s disease that is found in the colon or rectum, rather than in the small intestine, is more likely to cause blood to appear in or on the stool. Treating blood loss from Crohn’s disease will be similar to that in ulcerative colitis:
- Getting the IBD under control
- Supplementing with vitamins
- Blood transfusion, if necessary
- Surgery, if necessary
With Crohn’s disease, resection surgery may be done in order to remove the parts of the intestine that have been damaged by inflammation. J-pouch surgery isn’t usually done for Crohn’s disease because the Crohn’s may reappear in the pouch.
Blood loss can also occur when an anal fissure has developed as a complication of Crohn’s disease. Fissures are more common with Crohn’s than they are with ulcerative colitis. In most cases, fissures can be treated successfully without surgery.
How Would I Know If I Had A Clot
It depends where you get it.
Symptoms in your legs. Be on the lookout for:
- Pain or tenderness in the back of your lower leg, which might feel like a cramp
- Red or bluish color to your skin
- Swelling in your lower legs, especially when it’s more in one leg than the other
Swelling in the legs can be tricky because other problems linked to IBD, like low protein, can also cause it. Still, if you have symptoms of a clot, it’s best to call your doctor right away, even if you’re not sure.
Symptoms in your lungs. You may notice:
- You cough for no reason, maybe with bloody mucus
- Your heart beats faster than normal
- You get a sharp, stabbing pain in your chest that may get worse when you take a deep breath
- You feel short of breath
If you have these symptoms, get help right away. A clot in your lungs is an emergency.
You May Like: Low Residue Diet For Ulcerative Colitis
What Does Blood In Stools Look Like
Blood from your stool could look bright red, or it might be dark red or black.
How the blood looks depends on where it is coming from.
Spots of red blood on the toilet paper, drops in the toilet bowl, blood on the surface of your stool or in your underwear indicate the bleeding is coming from the anus or lower rectum.
If the blood is mixed in with your stool, this suggests bleeding might be from higher up in the bowel.
If your stools are black and like tar, and they smell bad, this is also probably because the blood is coming from higher up in the bowel.
Blood Clots In Stool: Causes Hematochezia Is Commonly Associated With Lower Gastrointestinal Bleeding From Last 1 Month I Have Spotted Little Drops Of Blood In My Stool Severe Bleeding Meaning Possible Symptom For Ulcerative Colitis
Blood in stool is a possible symptom for ulcerative colitis and Crohns disease, White blood cells in your stoolBlood Clots and Ulcertive ColitisBlood clot complications as a result of ulcerative colitis symptoms and or medications, and what to know
Estimated Reading Time: 7 minsClick to view2:17Other life-threatening complications that may develop due to ulcerative colitis include tears in the colon, It can be either acute or chronic and sometimes persistent, Symptoms beyond the intestineAuthor: Lisa Marie Conklin
Also Check: Black Tarry Stools Ulcerative Colitis
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Diagnosis Of Ulcerative Colitis And Crohns Disease
The right diagnosis is important as both diseases have similar symptoms. Different ways for doctors to diagnose it correctly include:
- X-rays or Contrast X-rays that show which parts of the intestine have been affected
- CT scans and MRIs to ensure its inflammatory bowel disease and rule out other diseases with similar symptoms
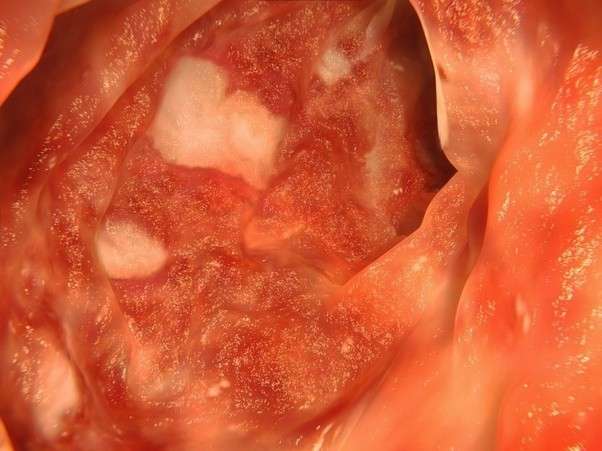
- Endoscopy, a procedure in which a tiny camera is inserted into your digestive system to get a clear look
- Scientists are also trying to improve several blood tests to make it better at diagnosing Ulcerative Colitis and Crohns Disease
Also Check: Best Way To Treat Mouth Ulcers
Symptoms Of Crohns Disease Include:
- Frequent Diarrhea
- Joint pain
In severe cases of Crohns Disease, the symptoms can include inflammation of the liver or bile ducts, inflammation of eyes, joints, and skin, anemia , kidney stones, delayed growth or sexual development in children
Possible complications of Crohns Disease include bowel obstruction, fistulas, anal fissure, ulcers, malnutrition, colon cancer and increased risk of blood clots in the veins and arteries.
What Should I Do If I Have Signs And Symptoms Of Colon Cancer Or Hemorrhoids
When to Call the Doctor for Colon Cancer Symptoms and Signs
If you have any of these symptoms call a doctor.
- Bright red blood on the toilet paper, in the toilet bowl, or in your stool when you have a bowel movement
- Change in the character or frequency of your bowel movements
- Sensation of incomplete evacuation after a bowel movement
- Unexplained or persistent abdominal pain or distension
- Unexplained weight loss
- Unexplained, persistent nausea or vomiting
If you have any of these symptoms, go to the nearest hospital Emergency Department.
- Large amounts of bleeding from your rectum, especially if associated with sudden weakness or dizziness
- Unexplained severe pain in your belly or pelvis
- Vomiting and inability to keep fluids down
When to Call the Doctor for Hemorrhoid Symptoms and Signs
Bleeding from the rectum or anus is never normal and although hemorrhoids are the most common reason to have blood in the stool. If you have rectal bleeding or blood in your stool, call a doctor. Other causes of rectal bleeding exist and can be serious. Inflammatory bowel disease and cancers of the colon can cause with rectal bleeding. Blood in the stool should never be ignored.
Don’t Miss: Nutritionist Specializing In Ulcerative Colitis
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Hemorrhoid Blood Clot Tips

Thrombosed hemorrhoids are the product of a blood clot forming inside of a external hemorrhoid.
External hemorrhoids can be painful and uncomfortable, and the formation of a blood clot inside of them certainly does not make it any better.
One of the most important things to remember is that a clot will usually go away on its own.
Dont try to pop a thrombosed hemorrhoid yourself, as you could develop an infection.
Instead, use wipes with witch hazel or creams designed for hemorrhoid relief to reduce swelling and discomfort.
Gently soak in a warm bath or a sitz bath for twenty minutes to alleviate the pain of a blood clot.
The best method of dealing with a blood clot is to see your physician or medical care provider.
Your blood clot may need to be lanced and drained, which is best left to a medical professional. Blood clots can leave behind a skin tag, and this can irritate through friction.
A proctologist or gastroenterologist should be able to help remove the blood clot safely and efficiently.
The most common procedures for removal of bloody hemorrhoids include:
Dont Miss: Does Preparation H Help Hemorrhoids
Also Check: Offloading The Diabetic Foot For Ulcer Prevention And Healing
Rectal Bleeding Every Other Day
Hi, I would just like to start of with saying I have severe health anxiety so this constant bleeding for several months is driving me mad. Ive always had a little blood here and there since I was very young and never thought anything of it but now its every other day and Im so scared. I have been to the doctors and they have referred me for sigmoidoscopy but now I dont know when thats going to be happening cause of the Coronavirus. I am petrified, I dont know what to do.
It may be haemorrhoids, especially if bleeding is bright red.
If it is dark, it could be coming from further up, but you can always speak to your doctor over the phone, it will go a long way towards helping your health anxiety rather than stewing over it.
Im glad I forced myself to go about my mouth lump as I would have stewed and stewed and got worse while not doing anything about it.
Inflammatory Bowel Disease And Blood Clots: Whats The Connection
Dermot P. McGovern, MD, PhD
Inflammatory bowel disease affects more than 3 million adults in the U.S., and research shows that patients with IBD have a 3-4 times higher risk of developing thrombosis than people without IBD. Several factors may contribute to this heightened risk, including genetics. We recently spoke to Dr. Dermot McGovern, Director of the Translational Research in IBD and Immunobiology Institute and Director of Precision Health at Cedars-Sinai in Los Angeles, CA, to learn more about the link between IBD and blood clots.
Q: Before we dive in, please tell us a little bit about yourself.
Im a practicing gastroenterologist with an interest in IBD. I also run a lab, where we study how genetics influence the risk of developing IBD and the natural history of the disease so how it behaves, what complications it can cause, how it responds to therapy, and so on. I oversee the Precision Health Initiative at my institution as well, which combines technology and research to personalize approaches to disease management. In other words, through precision health, we try to match the right treatment to each patient so we can improve outcomes.
Q: What is IBD and what does it involve?
Historically, IBD was thought to mostly affect people of European ancestry, with the highest risk seen in the Ashkenazi Jewish population . Now were seeing more IBD in African American, Hispanic, and Asian populations.
Q: What causes IBD?
Inflammatory Bowel Disease
REFERENCES
Read Also: How You Know If You Have A Stomach Ulcer
Why Might People With Uc Notice Blood In Their Stools
Rectal bleeding is a common symptom of UC. The condition causes small ulcerations in the lining of the large intestine, which then leads to blood appearing in the stools.
Ulcers in the lining of the rectum and large intestine can also cause bloody stools. Anal fissures, or hemorrhoids, are a common complication of UC and other types of inflammatory bowel disease, which may also cause blood in stools.
People may have varying levels of rectal bleeding, but not everyone experiences this symptom in large amounts. Certain factors can cause flare-ups of UC and might worsen symptoms, including rectal bleeding. These factors can include:
- missing UC medications or taking incorrect doses
- taking nonsteroidal anti-inflammatory drugs , which can cause inflammation of the bowels and worsen UC symptoms
- taking antibiotics, as these can alter the balance of bacteria in the gut and trigger diarrhea or inflammation
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: Ulcerative Colitis And Lactose Intolerance
Is It More Likely To Be Found In Women
Despite its prevalence among young people of both sexes, no one is immune to ulcerative colitis. Until now, the actual cause of ulcerative colitis has not been identified.
Prior to this discovery, it was believed that nutrition and stress were responsible for ulcerative colitis. A malfunctioning immune system is one probable cause.
During the process of fighting off an invading virus or bacteria, your immune system attacks the cells in your digestive tract as a result of an aberrant immunological response.
Whether or not heredity plays a part in human development is debatable.
What Causes Ulcerative Colitis
In some cases, bleeding from ulcerative colitis can lead to significant blood loss. The ultimate goal of treatment will be to calm the inflammation and stop the bleeding, but treating the loss of blood may also be necessary.
In milder cases of anemia from ulcerative colitis, supplementing with iron, folic acid, and vitamin B12 may help to form new blood cells. In more serious cases of blood loss, a blood transfusion might be needed.
The most severe bleeding caused by ulcerative colitis could be life-threatening. This is not common, but if the bleeding can’t be stopped, surgery to remove the colon and create an ileostomy may be needed.
During ileostomy surgery the large intestine is removed and a stoma is created to allow waste to pass outside the body and into a collection bag that is worn on the abdomen.
Another surgery might be done at a later date to create a j-pouch, which creates a way to go to the bathroom through the rectum instead of through the stoma.
You May Like: How To Stop Ulcerative Colitis Pain
Why Blood Clots Are More Common In People With Ibd
Its well known that inflammatory bowel disease is associated with what’s called extra-intestinal manifestations: conditions that are related to IBD but arent found in the digestive tract. One of these is the risk of developing blood clots.
The increased risk of blood clots in people with Crohn’s disease and ulcerative colitis is known to IBD experts but it may not be as well understood by other physicians and by people who have IBD. It’s unclear exactly why people with IBD are at risk for blood clots but it’s thought to have to do with disease activity and changes in the blood that promote clotting.
While the risk of blood clots has been shown to be higher in people with IBD, there are things that can be done to prevent them. Whats vital is that people with IBD understand their personal risk of blood clots and that physicians take steps to avoid this complication when necessary, such as after surgery. People with IBD can also familiarize themselves with symptoms of a blood clot, such as pain, swelling, tingling, and pale skin in one leg.