Pressure Ulcer Prevalence Varied By Age Sex And Length Of Time Since Admission To The Nursing Home But Not By Race
Residents aged 64 years and under were more likely than older residents to have pressure ulcers . Pressure ulcers were more common in males than in females . Residents in nursing homes for 1 year or less were more likely to have pressure ulcers than those with a longer length of stay . There was no significant difference between white and nonwhite populations with respect to having pressure ulcers.
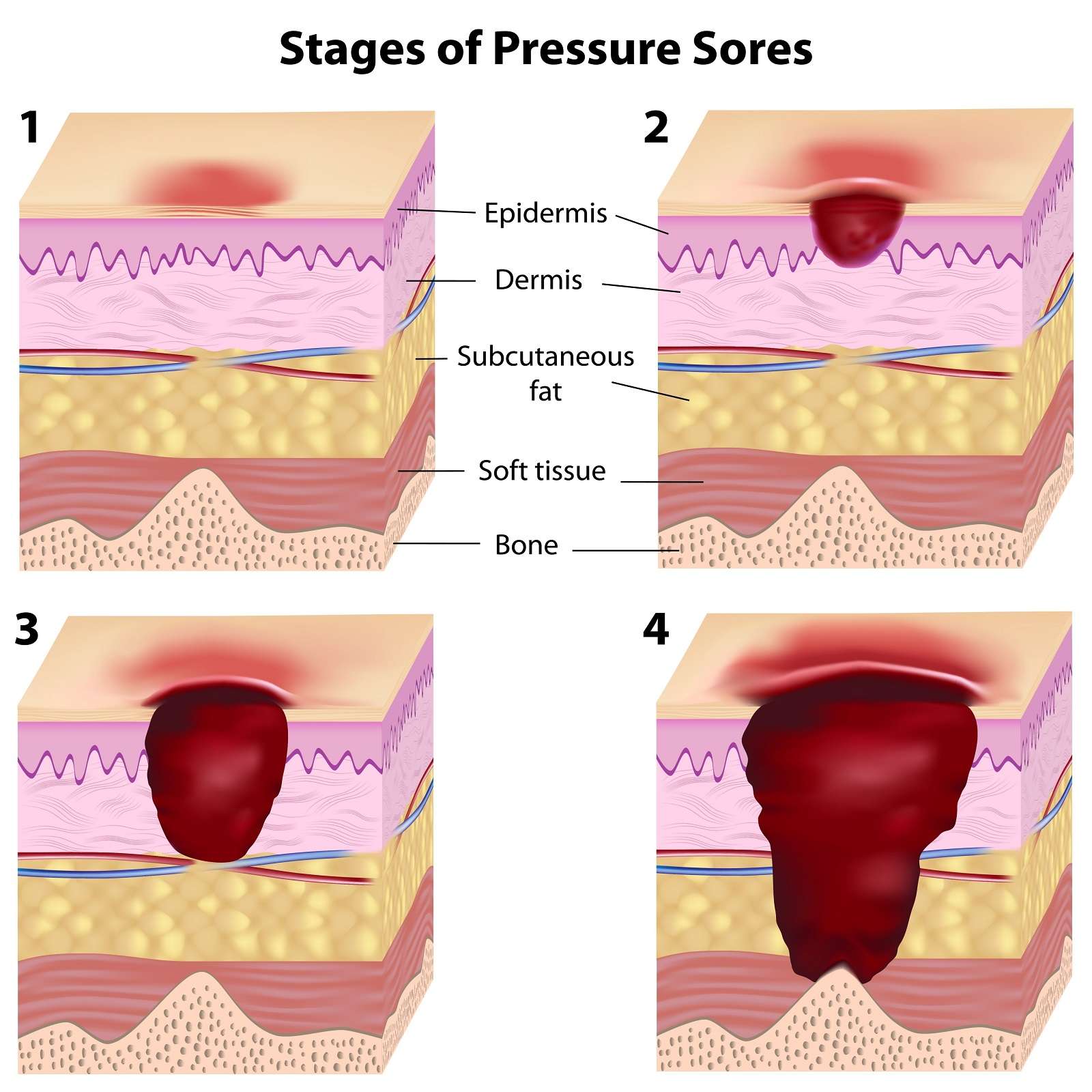
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Foam dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
What Causes Pressure Sores
Pressure sores are caused by sitting or lying in one position for too long. Its important to know that a pressure sore can start quickly. In fact, a Stage 1 sore can occur if you stay in the same position for as little as 2 hours. This puts pressure on certain areas of your body. It reduces blood supply to the skin and the tissue under the skin. If you dont change position frequently, the blood supply will drop. A sore will develop.
Don’t Miss: Is Soy Sauce Ok For Ulcerative Colitis
Examples Of Good Practice
SSkin offers 5 simple steps to prevent and treat pressure ulcers.
Stop the Pressure provides details of many pressure reduction and pressure prevention initiatives across England.
PUinfo App by Buckinghamshire New University provides information to prevent pressure ulcers for people at risk and their carers.
The Eatwell Guide shows the proportions in which different types of foods are needed to have a well-balanced and healthy diet.
React to Red has been developed by the University Hospitals Coventry and Warwickshire NHS Trust, encouraging patients, carers and families to react to red skin over bony areas and ask for help and advice from a healthcare professional.
When To Get Medical Advice
If you’re in hospital or a care home, tell your healthcare team as soon as possible if you develop symptoms of a pressure ulcer. It’ll probably continue to get worse if nothing is done about it.
You should be regularly monitored and offered advice and treatment to reduce the risk of pressure ulcers, but sometimes they can develop even with the highest standards of care.
If you’re recovering from illness or surgery at home, or you’re caring for someone confined to bed or a wheelchair, contact your GP surgery if you think you or the person you’re caring for might have a pressure ulcer.
Get medical advice immediately if there is:
- red, swollen skin
- pus coming from the pressure ulcer or wound
- cold skin and a fast heartbeat
- severe or worsening pain
- a high temperature
These symptoms could be a sign of a serious infection that needs to be treated as soon as possible.
Recommended Reading: Is Ulcerative Colitis An Inflammatory Bowel Disease
The Reactive Hyperaemia Cycle
Unlike in water, all animals on land are unsupported by the medium they find themselves in. Therefore, all soft-bodied animals must develop mechanisms to ensure they do not suffer damage when their tissues are distorted by contact with whatever is supporting them. Despite this being an essential requirement of survival on dry land, little or no research seems to have been done to identify what physiological mechanisms exist to prevent pressure damage.
However, it is reasonable to assume that tissue distortion, when it occurs, causes ischaemia. This in turn stimulates protective movements to relieve distortion, and circulatory activity which aims to restore normal blood perfusion in the affected areas. The majority of protective movements are reflexes and the person is unaware of making them. However, if these prove insufficient to relieve ischaemia, the central nervous system is stimulated by discomfort and ultimately by severe pain. This generally ensures that pressure is relieved before permanent damage has been done.
Apart from restoring tissues to their resting state after an ischaemic episode, the circulatory system has a direct role in optimising perfusion of the tissues during distortion. Studies have shown that adaptive changes occur in the microcirculation in response to repeated loadings of tissue , although little is known about their triggers and mechanisms.
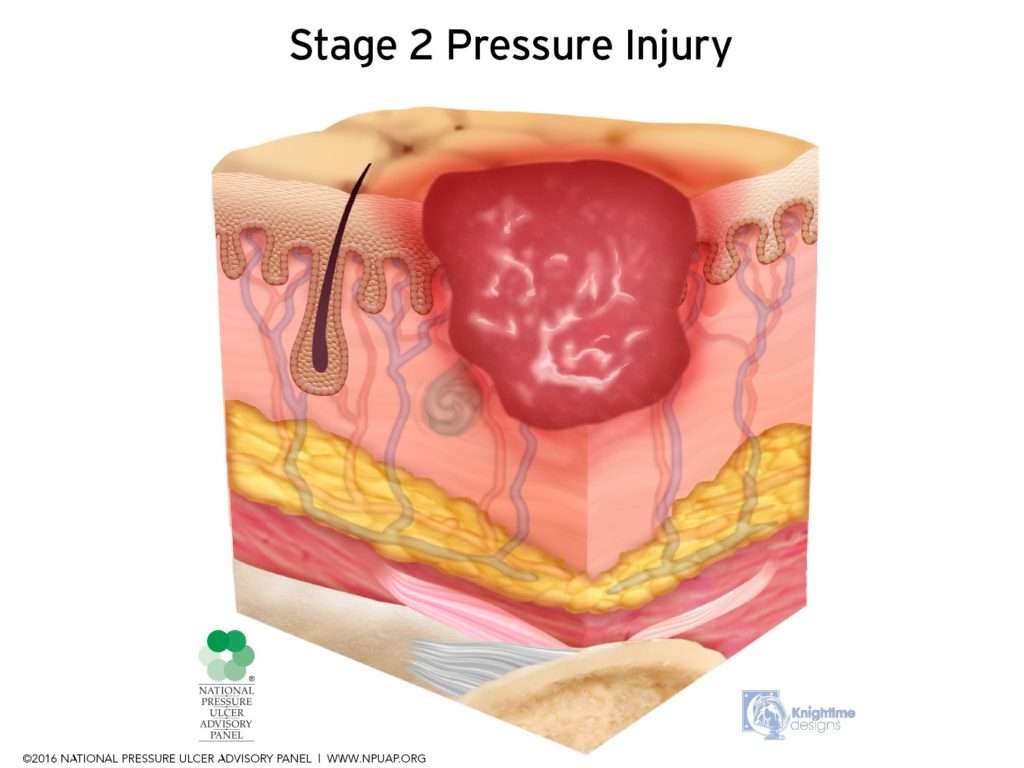
How Are Pressure Sores Diagnosed
Your doctor will do a physical exam to look at the sores. They will examine the size and depth of the sore and look to see if blood or fluid is oozing from the sore. Your doctor will check to see if your sore has a bad smell. They also will check for additional sores.
Testing may help to diagnose pressure sores or their complications. These tests might include a blood test. Another test would be to take a sample of the tissue from the sore. This is done by scraping or cutting it from the sore. That sample is sent to the lab for examination.
You May Like: Prednisone For Ulcerative Colitis Reviews
Comorbidities And Pressure Ulcers Development
The common age-related chronic diseases are identified as cardio-vascular, diabetes, lung, renal, musculoskeletal, neurodegenerative diseases. Exploring the impact of these diseases provides insight into multidimensional effects on older patients regarding clinical symptoms, complications, consequences and effectiveness of treatment. Progression of these diseases can be manifested through impaired motor, sensory, immune and hormonal systems and lead to frailty, disability, geriatric syndromes and isolation. The combined effect of these impaired systems and organs may result in associated complicating conditions including malnutrition, anemia of chronic disease, recurrent infection, polypharmacy and hospitalization. The significance of comorbidity risk factors in the pathogenesis of PU requires further investigation, recognizing the insolvability of PU prevention solely with external relief devices.
Who’s Most At Risk Of Getting Pressure Ulcers
Anyone can get a pressure ulcer, but the following things can make them more likely to form:
- being over 70 older people are more likely to have mobility problems and skin that’s more easily damaged through dehydration and other factors
- being confined to bed with illness or after surgery
- inability to move some or all of the body
- medical conditions that affect blood supply, make skin more fragile or cause movement problems such as diabetes, peripheral arterial disease, kidney failure, heart failure, multiple sclerosis and Parkinson’s disease
Recommended Reading: What Foods To Eat With Ulcerative Colitis
Patient Positioners And Support Surfaces
Every year, hospital facilities spend an estimated $26.8 billion dollars treating hospital acquired pressure injuries and their related complications. The Centers for Medicare and Medicaid consider HAPIs to be “never events” and in 2008 eliminated reimbursement for costs associated with them. According to the Agency for Healthcare Research and Quality, HAPIs have continued to increase, therefore, adding additional expenses to healthcare systems.
For over 50 years, Action Products has designed and manufactured patient positioners and support surfaces that help protect your patients against pressure injuries. Our products provide pressure relief and shear reduction in a variety of surgical settings including preoperative, perioperative and postoperative.
From pediatrics to bariatrics, our proprietary Akton® viscoelastic polymer has revolutionized the positioning market because of its unique attributes:
Incidence Mortality And Costs
The incidence rates of pressure ulcers vary greatly with the health care settings. The National Pressure Ulcer Advisory Panel says the incidence ranges from 0.4 percent to 38 percent in hospitals, from 2.2 percent to 23.9 percent in skilled nursing facilities, and from 0 percent to 17 percent for home health agencies. There is ample evidence that the majority of pressure ulcers occur relatively early in the admissions process. For patients in the hospital, they can occur within the first 2 weeks. With the increased acuity of elderly patients admitted and decreased lengths of stay in hospital, new data suggest that 15 percent of elderly patients will develop pressure ulcers within the first week of hospitalization. For those elderly residents admitted to long-term care, pressure ulcers are most likely to develop within the first 4 weeks of admission.
Mortality is also associated with pressure ulcers. Several studies noted mortality rates as high as 60 percent for older persons with pressure ulcers within 1 year of hospital discharge., Most often, pressure ulcers do not cause death rather the pressure ulcer develops after a sequential decline in health status. Thus, the development of pressure ulcers can be a predictor of mortality. Studies further suggested that the development of skin breakdown postsurgery can lead elders to have major functional impairment post surgical procedure.
Also Check: Are Ulcerative Colitis And Ibs The Same
Chronic And Acute Susceptibility
To formulate effective plans for the prevention and management of pressure ulcers it is important to understand that regardless of aetiology patients at risk of pressure damage fall into one of two groups – those who are acutely susceptible and those who are chronically susceptible.
Acute susceptibility arises due to sudden illness or trauma or due to an operative procedure. It is likely to be of relatively short duration and once the underlying causes are resolved, the patient will usually be susceptible no longer. For example, a patient admitted for surgery may only require high-dependency care for a short period on the day of the operation and overnight but will not be susceptible the following day when no longer ventilated and sedated. Following an acute episode, however, the patient may remain chronically susceptible if the acute episode causes permanent damage to the bodys defence mechanisms against pressure damage. For example, immediately following spinal injury there is an acute phase when there is very high susceptibility . This resolves after a period of time but the patient remains susceptible to some degree for the rest of their life.
Chronic susceptibility can be exacerbated by acute episodes. For example, an illness such as a chest or urinary tract infection may reduce tissue tolerance to pressure and increase susceptibility acutely for the duration of the illness.
Symptoms Of Pressure Ulcers
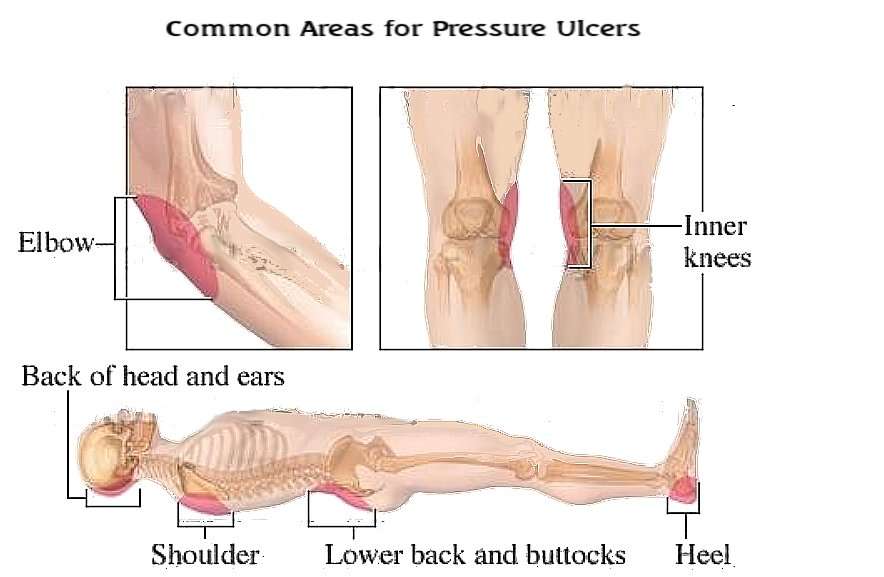
The parts of the body most at risk of developing pressure ulcers are those that are not covered by a large amount of body fat and are in direct contact with a supporting surface, such as a bed or a wheelchair.
For example, if you are unable to get out of bed, you are at risk of developing pressure ulcers on your:
- shoulders or shoulder blades
- knees, ankles, heels or toes
- spine
- tail bone
If you are a wheelchair user, you are at risk of developing pressure ulcers on:
- your buttocks
- the back of your arms and legs
- the back of your hip bone
Don’t Miss: Best Protein For Ulcerative Colitis
How Should A Standardized Pressure Ulcer Risk Assessment Be Conducted
As discussed above, one purpose of comprehensive skin assessment is to identify visible changes in the skin that indicate increased risk for pressure ulcer development. However, factors other than skin changes must be assessed to identify patients at risk for pressure ulcers. This can best be accomplished through a standardized pressure ulcer risk assessment.
3.3.1 What is a standardized pressure ulcer risk assessment?
After a comprehensive skin examination, pressure ulcer risk assessment is the next step in pressure ulcer prevention. Pressure ulcer risk assessment is a standardized and ongoing process with the goal of identifying patients at risk for the development of a pressure ulcer so that plans for targeted preventive care to address the identified risk can be implemented. This process is multifaceted and includes many components, one of which is a validated risk assessment tool or scale.
Other risk factors not quantified in the assessment tools must be considered. Risk assessment does not identify who will develop a pressure ulcer. Instead, it determines which patients are more likely to develop a pressure ulcer, particularly if no special preventive interventions are introduced. In addition, risk assessment may be used to identify different levels of risk. More intensive interventions may be directed to patients at greater risk.
Action Steps
Ask yourself and your team:
3.3.2 Why is a pressure ulcer risk assessment necessary?
Action Steps
Ask yourself and your team:
How Do Hospitals Prevent Pressure Ulcers
Skin care in hospital
Don’t Miss: Arterial Ulcer Vs Venous Ulcer
Implementing A Prevention Plan
Preventing pressure ulcers can be nursing intensive. The challenge is more difficult when there is nursing staff turnover and shortages. Studies have suggested that pressure ulcer development can be directly affected by the number of registered nurses and time spent at the bedside., In contrast, however, one recent study suggested that there was no correlation between increasing the nurse-to-patient ratio and the overall incidence of pressure ulcers. Donaldson and colleagues noted that this particular study was limited by the fact that the researchers could not affirm compliance with ratios per shift and per unit at all times. Given that the cost of treatment has been estimated as 2.5 times that of prevention, implementing a pressure ulcer prevention program remains essential.
A key component of research studies that have reported reduction of pressure ulcers is how to sustain the momentum over time, especially when the facility champion leaves the institution. It is clear from the evidence that maintaining a culture of pressure ulcer prevention in a care setting is an important challenge, one that requires the support of administration and the attention of clinicians.
If You Use A Wheelchair
Make sure your wheelchair is the right size for you.
- Have your doctor or physical therapist check the fit once or twice a year.
- If you gain weight, ask your doctor or physical therapist to check how you fit your wheelchair.
- If you feel pressure anywhere, have your doctor or physical therapist check your wheelchair.
Sit on a foam or gel seat cushion that fits your wheelchair. Natural sheepskin pads are also helpful to reduce pressure on the skin. DO NOT sit on a donut-shaped cushions.
You or your caregiver should shift your weight in your wheelchair every 15 to 20 minutes. This will take pressure off certain areas and maintain blood flow:
- Lean forward
- Lean to one side, then lean to the other side
If you transfer yourself , lift your body up with your arms. DO NOT drag yourself. If you are having trouble transferring into your wheelchair, ask a physical therapist to teach you the proper technique.
If your caregiver transfers you, make sure they know the proper way to move you.
Also Check: Pepto Bismol And Ulcerative Colitis
Treatments For Pressure Ulcers
Treatments for pressure ulcers depend on how severe they are.
For some people, they’re an inconvenience that needs basic nursing care. For others, they can be serious and lead to life-threatening complications, such as blood poisoning.
Ways to stop pressure ulcers getting worse and help them heal include:
- applying dressings that speed up the healing process and may help to relieve pressure
- moving and regularly changing your position
- using specially designed static foam mattresses or cushions, or dynamic mattresses and cushions that have a pump to provide a constant flow of air
- eating a healthy, balanced diet
- a procedure to clean the wound and remove damaged tissue
Surgery to remove damaged tissue and close the wound is sometimes used in the most serious cases.
Read more about the treatments for pressure ulcers.
How Can Pressure Sores Be Prevented In The Elderly
7 Steps to Prevent Pressure Sores
Don’t Miss: How To Fix A Stomach Ulcer
Why Are Older Adults At Risk For Pressure Ulcers
Diseases related to neuromotor and skeletal muscle disorders impair quality of life, self-care, and functional capacity among the elderly, consequently interfering with nutrition and levels of sensory perception, mobility, activity, and moisture, which are classic risk factors for pressure ulcer development.
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Also Check: What Can I Take For A Stomach Ulcer
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.