Alarm Symptoms Of Ulcerative Colitis:
If you are already diagnosed with ulcerative colitis, there are several alarm symptoms to look out for. A change in your ulcerative colitis symptoms may mean that additional treatment is needed. Talk to your doctor immediately if you experience a new symptom, a change in your current symptoms or any of the following:
- An unusual amount of cankers or sores in your mouth
- Unexplained or unintentional weight loss
- Failure to gain weight
- Delayed puberty in teens
- Drainage of pus from, or severe pain near, the anus which is usually caused by an abscess.
- Anemia this blood condition results in fatigue and weakness. It is usually caused by heavy blood loss or a lack of dietary iron
- Rectal bleeding
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, persons with ulcerative proctitis generally do not have nutrient deficiencies however, other factors may influence an individuals nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, then modifications to the diet will be necessary to compensate for this.
Better overall nutrition provides the body with the means to heal itself. It is important to follow Canadas FoodGuide, but some foods may irritate the rectum and increase symptoms, even though they do not affect the disease course. The customized recommendations of a registered dietitian can address your sensitive digestive tract.
What Makes Yale Medicines Approach To Ulcerative Colitis Stand Out
At our Inflammatory Bowel Disease Program, we know the key to properly managing a patients disease is coordinating care among our specially trained physicians. Our program offers expertise in gastroenterology, surgery, pathology and radiology.
We have a team approach with doctors, physician associates, nurses and surgeons all working together, Dr. Proctor says. Plus, we have more than 25 years of experience to help our patients.
A goal is to empower people with ulcerative colitis to take an active role in their health care and improving their quality of life. To this end, Yale Medicine care providers work hard to educate patients about their disease. In our Inflammatory Bowel Disease Program, a dedicated APRN works closely with patients to offer nutritional resources, medication and surgical options and discuss topics like pregnancy and IBD and depression and chronic disease.
You May Like: Indian Diet For Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
Also Check: Low Residue Diet For Ulcerative Colitis
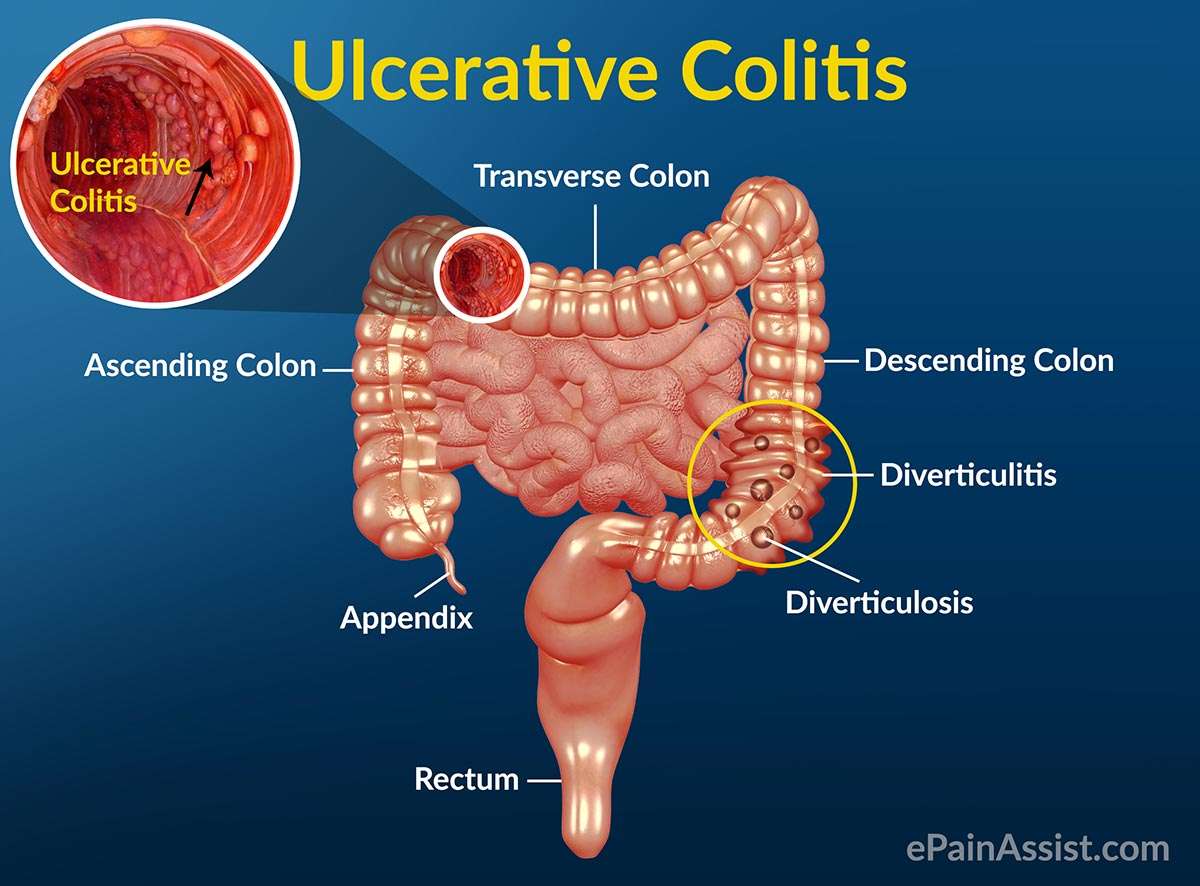
What Is Ulcerative Colitis
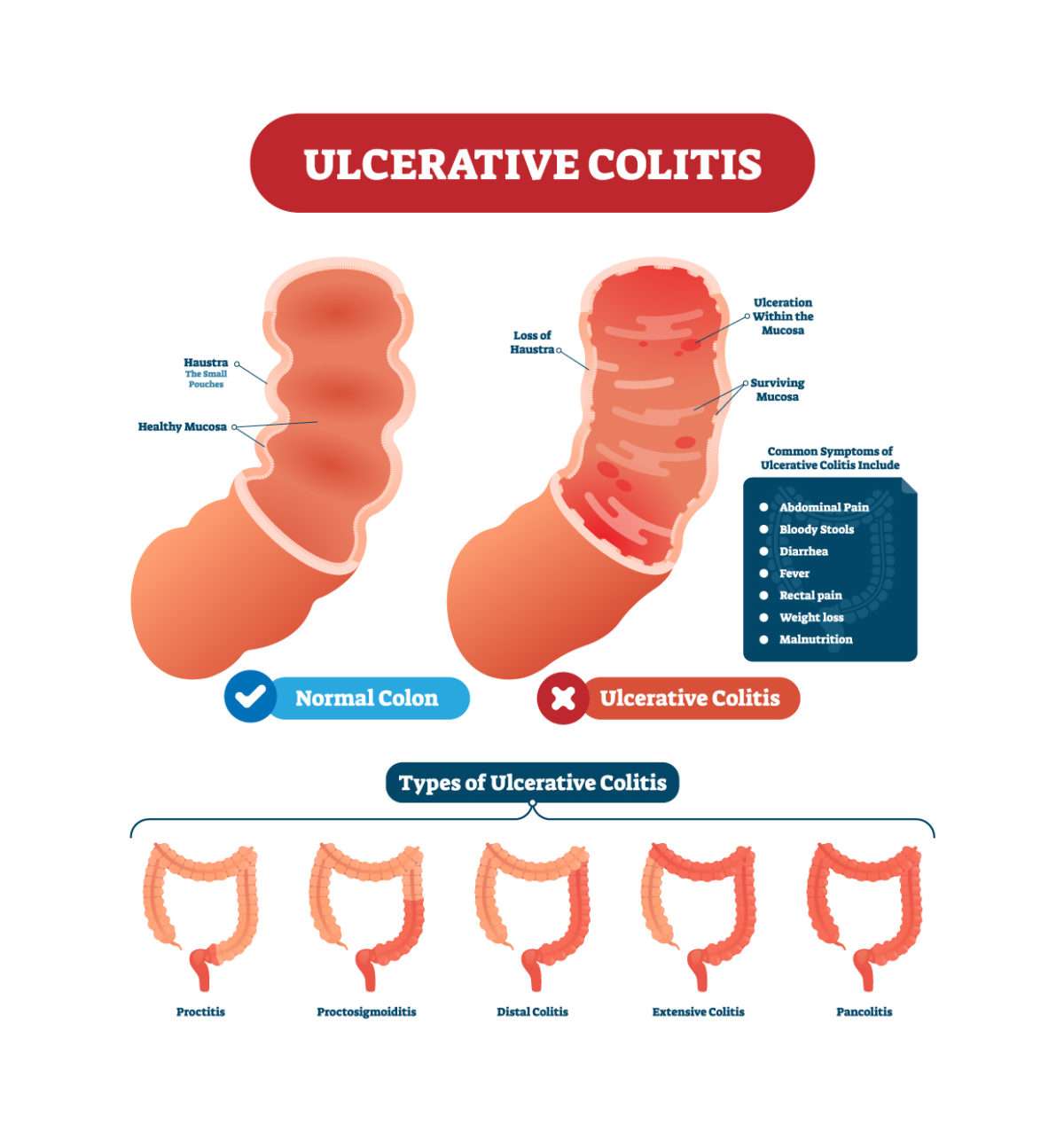
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
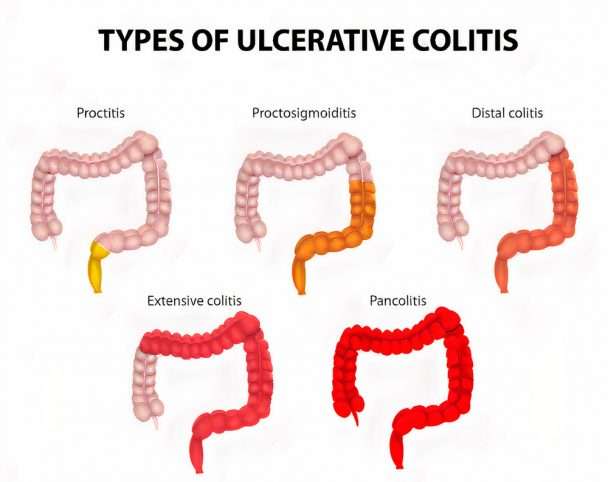
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
Urgency To Pass A Stool
Not only will the stool consistency change if you have ulcerative colitis, but the urge to pass could hit suddenly and strongly even though nothing comes out. If you have inflammation in the rectum, you have this sense of needing to get rid of something, even though its not there, says Dr. Englander.
Read Also: Ulcers In Small Bowel Crohn’s
Ulcerative Colitis Symptoms You Should Never Ignore
Ulcerative colitis is an autoimmune disease in which the immune system attacks the colon and causes a range of symptoms, both in the GI tract and around the body.
Symptoms of ulcerative colitis, a type of inflammatory bowel disease , can vary widely depending on how much inflammation a person has and where the inflammation is located.
Abdominal pain and bloody diarrhea are the most common warning signs of UC, and can range from mild and intermittent to severe and chronic. The pain of UC is quite common and can significantly impact quality of life. Ulcerative colitis symptoms tend to come and go, often with extended periods of time in between flares. These are called remission periods.
The disease tends to develop gradually over time, so you might not automatically think of ulcerative colitis or IBD if you have occasional abdominal pain or digestive distress.
Ongoing inflammation along with ulcers and abscesses in the intestines are additional common causes of pain. Scarring in the lining of the intestinal tract can lead to painful obstructions. Pain may occur in different areas such as the abdomen or rectal area, depending where the inflammation is located. For example, people may experience moderate to severe pain on the left side of the abdomen if the UC affects the rectum and the lower segment of colon.
UC symptoms might ebb and flow, but they wont go away unless you see a gastroenterologist and start treatment.
Ulcerative Colitis : Causes Symptoms Types Diagnosis & Treatment
Ulcerative colitis is an inflammatory bowel disease that affects the large intestine, especially the lower colon and rectum. Inflammatory bowel disease is a term that describes a group of diseases that affects the gastrointestinal tract. Inflammatory bowel disease involves Crohns disease and ulcerative colitis. Ulcerative colitis affects the inner lining of the colon, rectum, or both, which leads to inflammation, irritation, and ulceration. Ulcerative colitis may cause mild or severe symptoms, such as abdominal pain, diarrhea, bleeding per rectum, anemia, and weight loss. It may be dangerous and cause life-threatening complications that affect the skin, joint, bone, eye, liver, and lung. Also, ulcerative colitis may end in toxic megacolon or cancer colon. Ulcerative colitis is a chronic disease, and its symptoms develop gradually over a long period. Ulcerative colitis usually occurs in an intermittent course. Intermittent course means that there are asymptomatic periods between acute attacks of symptoms.
Ulcerative colitis affects both sexes in equal rate. It is common in those between 15 and 30 years old, but it also may occur in children or the elderly. Ulcerative colitis affects about 20 per 100000 people every year. In 2015, inflammatory bowel disease affected about 11 million people and caused about 50000 death. It is more common in the United States, Canada, and Europe than in other areas of the world.
Page 1 of 18
Don’t Miss: Foam Boots For Pressure Ulcers
What Is Uc Cramping
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.
Symptoms Of Chronic Ulcerative Colitis
Symptoms vary among patients depending upon where in the colon and rectum inflammation resides as well as its intensity. Inflammation may affect a small portion of the colon and rectum or, in worse cases, engulf the entire large intestine.
Patients with chronic ulcerative colitis are at risk of: anemia, from bleeding within the colon and rectum bone disorders, including osteoporosis, because nutrients are not being absorbed by the intestines and skin and eye disorders, common among patients with immune system diseases, such as rheumatoid arthritis. Patients with chronic ulcerative colitis also are at a higher risk of developing primary sclerosing cholangitis, a disorder of the bile ducts in the liver, and colon cancer.
Signs and symptoms of chronic ulcerative colitis can include:
- Persistent diarrhea or loose stools
- Bloody stools
Also Check: How Serious Is A Stomach Ulcer
Diagnosing Colitis And Chronic Ulcerative Colitis
Your gastroenterologist may suspect colitis based on your medical history and a review of your symptoms. He or she will have you undergo a colonoscopy procedure using a colonoscope to view the colon and rectum, and may take a tissue sample to help determine the cause. Other tests and procedures include:
- BLOOD TESTSBlood tests are taken to determine both red and white blood cell counts. A low red blood cell count can indicate anemia, from bleeding within the colon and rectum. Elevated white blood cells, which fight infection, indicate inflammation within the colon and rectum.
- STOOL SAMPLEA stool sample may be taken to rule out a parasitic infection that can cause colitis.
- CT SCANIn addition to a colonoscopy, a CT scan can determine what areas of the rectum and colon are inflamed.
Classification of chronic ulcerative colitis
Gastroenterologists categorize chronic ulcerative colitis based on the location and extent of inflammation within the colon and rectum. For most patients, the affected area remains the same during the course of the disease.
How Serious Is Left
Its logical to reason that if your UC is restricted to just the left side, its probably not as severe as UC that affects your entire colon. Not true. It all depends on the degree of inflammationnot where the inflammation is locatedas well as how well a person responds to medication.
If a patient has refractory left-sided colitis, they can be quite ill, with debilitating bloody diarrhea leading to anemia, malnutrition, and weight loss, says Jeffry A. Katz, M.D., a professor of medicine at Case Western Reserve University School of Medicine in Cleveland, OH.
Read Also: Can I Donate Blood If I Have Ulcerative Colitis
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
You May Like: Food To Avoid For Ulcer Patient
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Complementary And Alternative Remedies
Alternative treatments such as acupuncture may help to reduce and regulate bowel inflammation, reducing UC pain.
Another form of alternative treatment called moxibustion may also have a positive effect on UC symptoms. Moxibustion is a type of heat therapy. It uses dried plant materials burned in a tube to warm the skin, often in the same areas targeted by acupuncture.
Read Also: Ulcerative Colitis Social Security Disability
Types Of Ulcerative Colitis
Becoming well-informed about your chronic illness is a helpful part of your journey. It is important to learn all you can about your diagnosis and how it may affect you. We can help you understand the different types of ulcerative colitis, as well as the common symptoms and complications.
Ulcerative colitis is a chronic illness that can affect different parts of the colon and rectum. There is a wide array of symptoms and complications depending on the extent of your disease and the type of ulcerative colitis you have.
Getting diagnosed with a chronic, lifelong disease is overwhelming. It is important to learn all you can about your diagnosis and how it may affect you. We can help you understand the different types of ulcerative colitis, as well as the common symptoms and complications.
What Inflammatory Bowel Disease Pain Feels Like
Symptoms of inflammatory bowel disease can include diarrhea, blood in the stool, weight loss, and abdominal pain. The type and location of abdominal pain is different, not only between the two main forms of IBD but also within the subtypes of these diseases.
Further, pain is even more individual to each person, to the point where people with the same subtype of Crohn’s disease or ulcerative colitis may experience pain in a different way.
In fact, some people with IBD don’t have any abdominal pain at all during IBD flare-ups. In addition, abdominal pain can be related to other issues , such as appendicitis, gallstones, or gastroesophageal reflux disease .
But as abdominal pain is a common symptom of IBD, here is an overview of the types of abdominal pain that are most often experienced by people with IBD.
Read Also: Does Ulcer Pain Come And Go
Complications Of Ulcerative Colitis And How To Avoid Them
Learn how to identify and avoid potentially life-threatening complications of ulcerative colitis.
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
“It’s easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,” says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
How Is The Disease Diagnosed
Physicians make the diagnosis after taking a careful patient history, examining the patient and ordering a series of tests. The first goal of these tests is to make sure that an infection is not causing the diarrhea. Stool specimens are taken, blood tests are analyzed and a barium enema X-ray of the colon may be ordered if the patient is not too sick. The barium shows up white on the X-ray, providing a detailed picture of the colon. Finally, the patient may have a colon evaluation through a sigmoidoscopy or a colonoscopy.
In a sigmoidoscopy, the doctor passes a flexible instrument into the rectum and lower colon. The doctor then can see how much inflammation is in those areas. A total colonoscopy is similar, but it looks at the entire colon to detect bleeding, inflammation or ulcers on the wall. During these procedures, the physician usually takes a sample called a biopsy.
You May Like: Stomach Ulcer Blood In Stool
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.