Ulcerative Colitis And Cancer: What Is The Connection
People living with ulcerative colitis are 4 to 10 times more likely to be diagnosed with colorectal cancer compared with the general population.
This is because UC patients have higher levels of inflammation in the colon and an increased risk of developing inflammatory polyps in the lining of the colon or rectum. The majority of polyps are benign , but over time, some polyps can become cancerous.
The exact risk of colorectal cancer for people with UC varies depending on these three factors:
- Duration of the disease: It is believed that the risk of developing colorectal cancer starts to increase eight to 10 years following the onset of UC symptoms. One meta-analysis of 116 studies found that 10 years after onset, the risk is 1.6% at 20 years, it increases to 8.3% and 30 years after onset, it increases to 18.4%.
- Severity of inflammation: The more inflammation that is in your colon or rectum, the more damage there is to cells in the colon lining. This causes more cell turnover, which allows more opportunity for mutations in the DNA of these cells that can lead to cancer.
- How much of the colon is affected: Those with UC of the entire colon are at the highest risk. If UC only affects the left side of the colon, the risk of developing cancer is lower. And those with UC only in the rectum don’t have a heightened risk of colorectal cancer.
How Do I Spot The Signs And Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are abdominal pain and diarrhea, which often contains blood or pus.
Symptoms of the disease typically develop gradually and come and go.
Periods without active disease known as remission may last for months or even years.
Over time, ulcerative colitis can progress to cover more of the colon. This typically leads to more severe disease and greater symptoms.
If left untreated, UC can also lead to a number of complications, including:
- Malnutrition
Research And Statistics: How Many People Have Ulcerative Colitis
People of European descent have a higher risk of developing ulcerative colitis than do those of African or Hispanic descent.
People of European Jewish descent have an especially high risk.
Ulcerative colitis tends to run in families, affecting men and women equally overall. But older men are more likely to develop it than older women, according to the Crohns and Colitis Foundation.
Recommended Reading: How Does Ulcerative Colitis Affect The Body
What Medications Treat Ulcerative Colitis Symptoms
Medications that are used in the treatment of ulcerative colitis may be divided into two groups, anti-inflammatory and immune suppressive agents. The decision as to which medication regimen should be used will depend upon the severity of the ulcerative colitis. Physicians and patients need to discuss the benefits and risks of recommended treatments.
If the patient has mild or moderate colitis, the first line of treatment is the use of 5-ASA agents-a combination of two drugs sulfonamide and salicylate that helps to control the inflammation. Sulfasalazine is the most commonly used of these drugs. Sulfasalazine can be used for as long as needed and can be given along with other drugs. If the patient does not do well on sulfasalazine, they may respond to the newer 5-ASA agents. The side effects of 5-ASA preparations include nausea, vomiting, heartburn, diarrhea, and headache.
Drug therapy for active inflammatory bowel disease includes the following:
If the patient has severe colitis or does not respond to mesalamine preparations, they may be treated with corticosteroids. Prednisone , methylprednisolone , budesonide , budesonide MMX and are used to reduce inflammation. These drugs are taken during a flare-up, but are not used for maintenance when the ulcerative colitis is in remission. Corticosteroids can be taken by mouth, IV infusion, through an enema, or as a suppository, depending upon the location and severity of the inflammation.
- Hospital admission
Where To Buy Supplements For Ulcerative Colitis

You can purchase these supplements for ulcerative colitis at BulkSupplements.com. The company is an industry-leading manufacturer and distributor of pure dietary supplements.
BulkSupplements.com is not just a consumer brand. It also supplies pure ingredients to other food and supplement brands to make their products. All products at BulkSupplements.com are manufactured and tested according to current and proper manufacturing practices.
Are you interested in trying any of these supplements mentioned in this article as a possible solution to helping you with your ulcerative colitis? Contact BulkSupplements.com to place an order today.
Recommended Reading: Carbohydrate Diet For Ulcerative Colitis
Prognosis Of Ulcerative Colitis
Ulcerative colitis is usually chronic, with repeated flare-ups and remissions . In about 10% of people, an initial attack progresses rapidly and results in serious complications. Another 10% of people recover completely after a single attack. The remaining people have some degree of recurring disease.
People who have ulcerative proctitis have the best prognosis. Severe complications are unlikely. However, in about 20 to 30% of people, the disease eventually spreads to the large intestine . In people who have proctitis that has not spread, surgery is rarely required, cancer rates are not increased, and life expectancy is normal.
What Causes Ulcerative Colitis In A Child
Healthcare providers don’t know what causes this condition. It may be triggered by a virus or bacteria. This interacts with your childs immune system and causes an inflammatory reaction in the intestinal wall.
Children with ulcerative colitis often have problems with their immune system. But healthcare providers don’t know if these issues are a cause or a result of the disease.
Theres no cure for this condition, except to take out your childs colon with surgery. However, the symptoms can be managed medically.
Read Also: Symptoms Of Bleeding Ulcer In Esophagus
First Symptoms Of Ulcerative Colitis Causes & Treatment
Ulcerative colitis is a chronic condition in which the large intestine becomes inflamed with ulcers that cause diarrhea and bleeding. Ulcerative colitis generally affects the lower part of the colon and the rectum, though can affect the entire colon.
Ulcerative colitis is a type of inflammatory bowel disease . Another type of IBD is Crohns disease, which can affect any part of the gastrointestinal tract from the mouth to the anus.
Symptoms of ulcerative colitis vary and mild symptoms occur in about half of all patients. The first symptoms of ulcerative colitis may include:
- Loose and urgent bowel movements
- Frequent need to empty the bowels
- Bloody stool
- Persistent diarrhea accompanied by abdominal pain and blood, mucus, or pus in the stool
Other symptoms of ulcerative colitis may include:
Patients with ulcerative colitis often have relapses, when inflammation and symptoms worsen , followed by periods of remission, that can last months to years when symptoms subside.
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
Ulcerative proctitis has very few complications but with increased irritation to the anal and rectal area, hemorrhoids may occur. Only rarely do other complications occur, such as abscesses and extra-intestinal manifestations. Individuals with ulcerative proctitis are not at any greater risk for developing colorectal cancer than those without the disease.
You May Like: Best Treatment For Diabetic Foot Ulcer
Keep Up With Regular Physicals
Getting an annual physical is always smart, but it’s especially important if you have UC.
During the checkup, your healthcare provider will ask whether your treatments are going well and ensure that screening is performed at the appropriate intervals to catch any cancer in the early stages. Even if your UC symptoms are in remission , seeing a healthcare provider regularly can help ensure that you stay on the healthy track.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: Can A Heating Pad Help Ulcerative Colitis
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Living With Ulcerative Colitis
With careful management, most people with UC are able to enjoy life, including work, travel, recreation, sex and having children.
To keep healthy, consider:
- eating a nutritious diet to help with healing and reduce fatigue
- keeping a food diary to check if there are any foods that make your symptoms worse during a flare-up
- asking your doctor about supplements if you think you may be malnourished
- exercising regularly to lift your mood and help relieve stress
- learning some relaxation techniques to help manage stress
Also Check: Wound Care For Stage 4 Pressure Ulcer
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Feeling Comfortable With Your Doctor
Its not always easy to talk about your bowel habits. Talking about poop can be embarrassing, and many people may not be ready to open up to their doctor about it.
Others may ignore the changes to their stool or think that nothing is wrong. However, ignoring symptoms will only make things worse.
Your doctor has studied the gastrointestinal tract along with all that it does and produces. They have seen and heard it all. Nothing you say about your bowel symptoms is going to offend or shock them.
Its part of their job to know about any changes in your symptoms. Your doctor is there to help you, not to judge you.
You dont have to know any fancy medical terms when talking with your doctor about your symptoms. Share your concerns and any changes in your bowel habits you have noticed. Talking with them about changes in your stool can only help get you closer to resolving the problem.
Recommended Reading: Does Turmeric Help Ulcerative Colitis
What Are The Treatments Complications And Risk Of Cancer For Diverticular Disease Vs Ulcerative Colitis
Diverticular Disease Treatment
A high-fiber diet is the mainstay of diverticulosis and diverticulitis prevention.
- Start a high-fiber diet because it will decrease the risk of complications and the accompanying symptoms however, will not make the diverticula a person has gone away. Foods high in fiber include:
- Whole-grain cereals and bread
- Fruits
- Vegetables
- Beans, peas, and lentils.
In the past patients with diverticulosis/diverticulitis were told that foods to avoid included seeds, corn, and nuts because it was thought fragments of these foods would get stuck in the diverticula and cause inflammation. However, current research has not found this to be the case, and the fiber content of such foods may benefit individuals with diverticulosis/diverticulitis. Discuss your diet or potential diet changes with your doctor.
Treatment for diverticulitis depends on the severity of the condition.
Treatment consists of IV or oral antibiotics, bowel rest, and possibly surgery.
If diverticulitis attacks are frequent or severe, the doctor may suggest surgery to remove a part of the patient’s colon.
- As with any surgery, there are risks the patient should discuss with his or her doctor.
- Sometimes the operation requires at least two separate surgeries on different occasions.
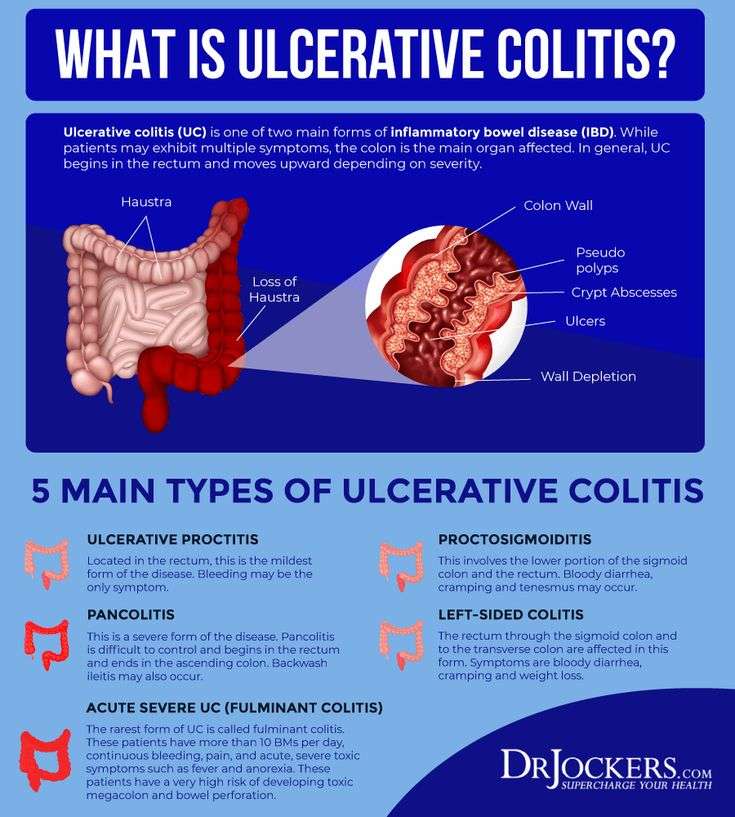
What Is Ulcerative Colitis
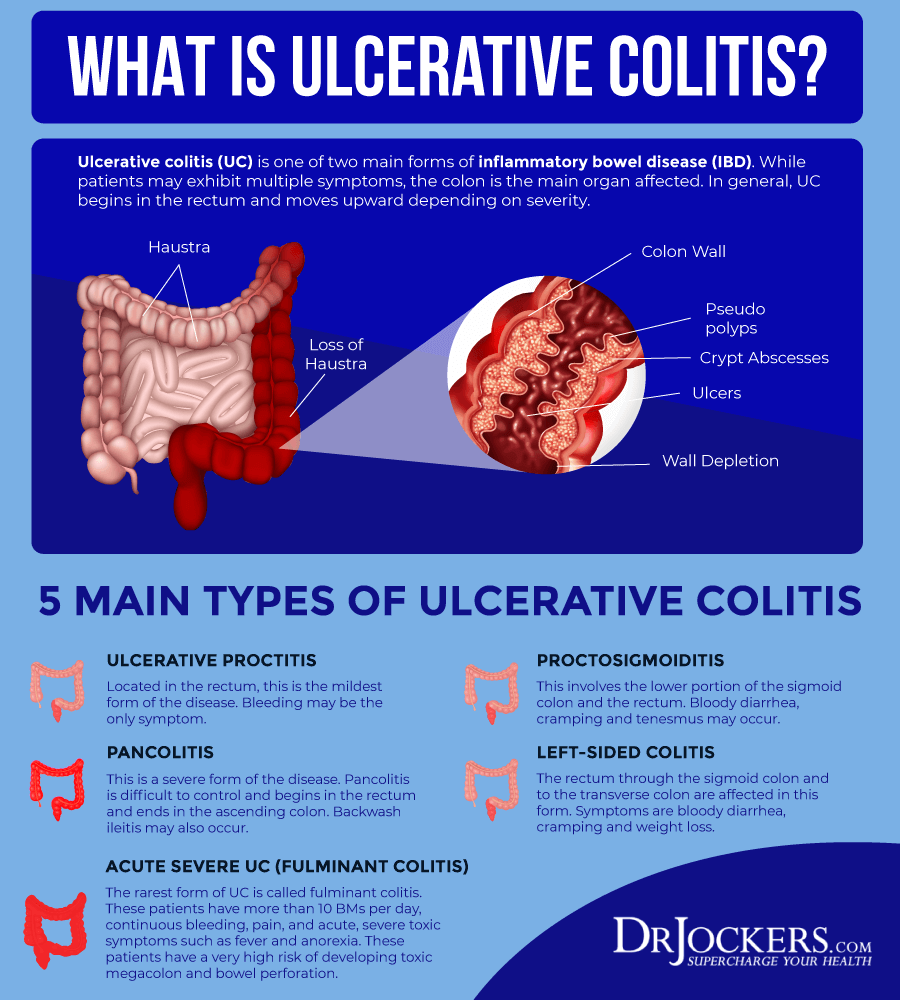
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
Recommended Reading: What Is Best Medicine For Ulcer
Is Ulcerative Colitis Curable
Currently, theres no nonsurgical cure for UC. Treatments for the inflammatory disease aim to extend periods of remission and make flare-ups less severe.
For people with severe UC, curative surgery is a treatment option. Removing the entire large intestine will end the symptoms of UC.
This procedure requires your doctor to create a pouch on the outside of your body where waste can empty. This pouch can become inflamed and cause side effects.
For that reason, some people choose to have only a partial colectomy. In this surgery, your doctor only removes the parts of the colon that are affected by UC.
While these surgeries can help ease or end symptoms of UC, they can have adverse effects and possible long-term complications. Read more about these issues to determine if surgery is an option for you.
Role Of Antibiotics In The Treatment Of Uc
Only a few trials of antibacterial agents have been carried out in UC and results are controversial. The rationale for their use is based on the possible pathogenetic role of bacteria, supported by clinical and experimental evidence.
Vancomycin, a non-absorbable antibiotic agent against Gram positive bacteria was administered orally in patients with idiopathic colitis. No overall difference in terms of efficacy was found between the two groups after seven days, but in UC patients there was a trend towards a reduction in the need for surgery.
Metronidazole, an agent effective against anaerobic bacteria, was given intravenously in severe UC as an adjunct to the intensive intravenous regimen. No benefit was observed in the group receiving metronidazole this drug was also ineffective when given orally.
Tobramycin, a non-absorbable antibiotic drug directed against Gram negative bacteria, was compared with placebo in a double blind study. Eighty-four patients with an acute relapse of UC were randomised to receive oral tobramycin or placebo for one week as an adjunct to steroid therapy. At the endpoint, 74% in the tobramycin group and only 43% in the placebo group obtained a clinical remission. No difference was found in long term activity.
Further, a combination of tobramycin and metronidazole administered intravenously together with conventional steroid treatment in acute, severe UC did not provide beneficial outcome.
Read Also: What Medicine Is Good For Ulcers
Axial Arthritis And Ulcerative Colitis
Although more common in people with Crohns disease, axial arthritis can also affect those with UC. Over time, axial arthritis causes pain and stiffness in the lower spine and sacroiliac joints, which connect the lower spine and pelvis.
The main symptoms of axial arthritis are stiffness and pain in the lower back, hips, and buttocks that persist for three or more months at a time. Flare-ups typically come on slowly, gradually worsening over a period of several weeks or months. Symptoms tend to be at their worst in the morning and wear off with time and exercise. Prolonged rest or inactivity can make joint pain worse.
I can’t bend or twist like I used to, wrote one MyCrohnsAndColitisTeam member. It hurts too bad. Being up and about helps, but getting up for those first few steps after sitting a while is so painful, and I can’t fully stand upright sometimes for a minute or so. It’s frustrating.
What Should You Eat When You Have Ulcerative Colitis
When it comes to food, theres no known dietary cause of ulcerative colitis, but different foods may aggravate or help limit symptoms of the disease.
Youre more likely to need to change your diet during periods of active disease , when eating soft, bland foods can help limit symptoms like cramping and diarrhea.
During flares, you may also want to avoid or limit high-fiber and high-fat foods, as well as caffeine, alcohol, dairy products, and spicy foods.
If youre losing nutrients and water in your diet due to diarrhea, you may need to focus on increasing your fluid intake and getting enough calories, protein, vitamins, and minerals from foods or supplements.
Read Also: What Is A Good Diet For Ulcers