When Does Cramping Usually Happen
UC cramps can be exacerbated by food, so many people notice cramping after eating or before a bowel movement, says Ha. Cramping can also be tied to eating trigger foods, which often include high-fiber fruits and veggies, lactose, nonabsorbable sugars, high-fat or sugary foods, alcohol, and caffeine.
The hormone fluctuations that occur during a womans menstrual cycle may also trigger UC cramping, according to a study published in January 2018 in Inflammatory Bowel Diseases.
Cramping can occur at all times and throughout the night. Medication and other treatments can help reduce symptoms.
What Causes Back Pain In Ulcerative Colitis
- Fatigue
- Weight loss
A person having backaches may not realize its related to digestive problems or think to mention it to their doctor. However, ulcerative colitis can cause extraintestinal symptoms including back pain.
Although back pain can result from other causes, such as injury or overexertion, UC-related back pain stems from inflammation. Generally speaking, people with ulcerative colitis can trace their back pain to spondyloarthritis. Spondyloarthritis, also known as spondylitis, is a type of arthritis that causes inflammation specifically in the axial joints those of the spine, chest, and pelvis. Spondyloarthritis includes axial arthritis and ankylosing spondylitis.
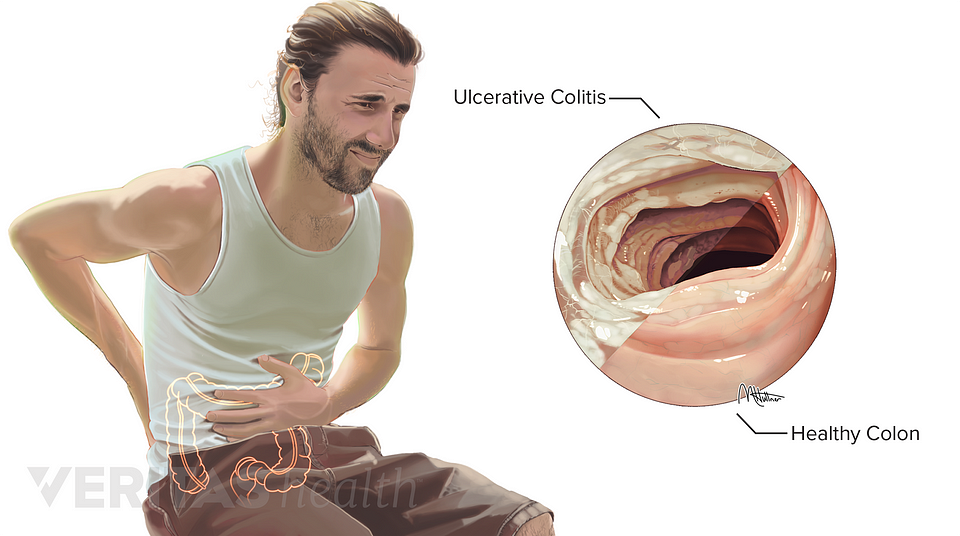
What Causes Ulcerative Colitis
Unfortunately the cause of ulcerative colitis is unknown, although both genetic and the environmental causes have been proposed.
Most patients with ulcerative colitis do not have anyone else in the family with ulcerative colitis. However up to 20 percent of patients with ulcerative colitis have at least one relative with either ulcerative colitis or Crohn’s disease. The genes involved in ulcerative colitis are not as well understood as in Crohn’s disease, and there are no commercially available genetic tests we currently recommend for the diagnosis of ulcerative colitis.
The increase in ulcerative colitis in some populations around the world has led some researchers to believe there may be environmental causes for ulcerative colitis. Infections and diet are among other potential environmental causes for ulcerative colitis however there is not enough information in this field to make any firm conclusions. There is still much to learn in these areas and research is ongoing to determine the cause of ulcerative colitis.
Don’t Miss: Foods Bad For Ulcerative Colitis
My Experience With Severe Pain In My Back
In 2008, I had such severe back pain I couldnt walk. I tried to go to school but needed my dad and male friends to literally carry me into class. It came on suddenly and was just so random to me.
I went to a ton of doctors, went through a lot of tests, physical therapy, acupuncture, etc. Nothing showed up and nothing helped. At my last appointment with an orthopedist, the doctor told me he had been thinking about my case for a while in between the tests and visits to other specialists. He even brought in colleagues to try and help him figure things out.
The conclusion was that there was nothing structurally wrong with my back. He believed the intense pain I was experiencing was from all of my abdominal surgeries. He thought my stomach muscles were so weak that it forced my back to pick up the slack, so to speak.
While this made sense, I had no idea what to expect for the future. Was this just how it was now? Did I just have to accept I would be this way forever?
Whats A Good Plan To Manage Uc Cramping
Monitor your medications. Talk to your doctor about any prescription, over-the-counter, or herbal medications youre taking. Iron deficiency is common with UC, but oral iron supplements have been shown to increase the risk of inflammation and cramping. Some antibiotics and pain relievers, such as ibuprofen, may also increase flare-ups and cramping.
Review your diet. Keep a food diary and note the connection between the foods you eat and your UC symptoms. In general, its smart to stay away from processed foods and those high in saturated fat and sugar. High-fiber foods and dairy products can also cause UC cramping, but check with your doctor before eliminating foods from your diet, to ensure youre getting the nutrients you need.
Eat frequent, small meals. Instead of two or three large meals, eat four to six smaller meals spaced more closely throughout the day. Also, take your time while eating and chew thoroughly.
Skip caffeine and carbonated drinks. Caffeine can cause gas, intensifying abdominal cramping. It is also a stimulant, which can make cramping and diarrhea worse.
Drink enough water. People with UC may be at increased risk of dehydration, so be sure to drink plenty of H2O. A good rule of thumb, according to the Crohns and Colitis Foundation, is to aim for about 64 ounces or eight 8 oz glasses per day.
Also Check: Is Nausea A Symptom Of Ulcer
What Is Uc Cramping
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.
Conditions That Cause Lower Back Pain And Constipation
It is also possible that you do not have IBS, but have constipation, which is also linked to lower back pain. Both constipation and lower back pain are fairly common medical issues, and are often nothing to be concerned about, but if they occur suddenly at the same time, it is advisable to see a doctor, as it might be a sign of a more serious issue. For example, the following are examples of conditions that cause both constipation and lower back pain to occur at the same time:
- Bowel obstruction
A bowel obstruction is a gastrointestinal condition in which digested material cannot pass normally or as it should through the bowel. A bowel obstruction can be caused by fibrous tissue that compresses the gut, which can develop many years after abdominal surgery. With a bowel obstruction, the blockage in your colon or rectum can create a dull pain that extends from the abdomen to the lower back.
- Endometriosis
Endometriosis is a condition in which the tissue that normally lines the uterus grows outside the uterus. In individuals with endometriosis, the tissues that should be lining the uterus can be found on the ovaries, fallopian tubes, or the intestines. Bowel symptoms are very common with endometriosis, as is back pain. This is because endometrial cells can stick to the lower back and the front of the pelvic cavities.
- Fibromyalgia
- Liver disorders
- Peritonitis
- Urinary tract infections
Read Also: Things To Eat When You Have An Ulcer
Duration And Intensity Of Pain Episodes In Ibd
The pain attacks most often had a duration of minutes to hours , in 11% the pain duration was seconds and in 10% up to 3 days with only 73 patients reporting pain over more than 5 days. 153 patients did not specify the pain attacks . In the subgroup analysis in the group of CD patients similar results were found with a pain duration of minutes to hours , in 13% the pain duration was seconds and in 11% up to 3 days with 8% reporting pain over more than 5 days. 74 patients did not specify. In the group of UC patients there was a pain duration of minutes to hours , in 10% the pain duration was seconds and in 9% up to 3 days with 8% reporting pain over more than 5 days. 78 patients did not specify. There was no statistically difference between CD und UC .
Breast Lung Abdomen Colon Pancreas Gallbladder
These types of cancers can metastasize to the spine and cause back pain. Also with abdominal cancers, pancreatic and gallbladder cancers, you can get the referred visceral pain even before they metastasize, says Dr. Crooks. When cancers do spread to the spine, you can have severe spinal pain.
Depending on the type of cancer, treatments like intrathecal pain pumps can deliver medicine like an anesthetic, nerve pain medicine, or a narcotic in small doses straight to the spine without negative effects like tolerance, addiction, and overdose. Stimulation to the spinal nerve root and spinal blocks are also effective treatments for spinal pain.
Wheres the pain? Depending on the type of cancer, back pain can be in the upper, mid, or lower spine
What are the other possible symptoms? Fatigue that doesnt improve with rest, unexplained weight loss or gain, loss of appetite, nausea, vomiting, swelling or lumps, skin changes, hoarseness, persistent cough, change in bowel habits, vision or hearing problems, headache, and others
What does it feel like? Back pain can range from mild to severe depending on the type of cancer and location and may not respond to OTC pain relievers
While your primary care doctor or specialist helps keep your medical issue in check, a pain specialist can improve chronic musculoskeletal pain that stems from inflammation and overstimulated nerves that can occur when you have one of these conditions.
You May Like: Ulcer In My Stomach Symptoms
What Are The Complications Of Ulcerative Colitis
Colon Cancer
Although most patients with ulcerative colitis will not develop colon cancer, patients with ulcerative colitis are at a 2 to 5 fold increased risk of developing colon cancer compared to persons without ulcerative colitis. Researchers believe the increased risk of colon cancer is related to chronic inflammation in the colon. In order to detect colon cancer at an early stage, most patients with ulcerative colitis will need to undergo colonoscopies on a regular interval that is more frequent than for patients without ulcerative colitis. The risk of colon cancer may be even higher in individuals who have a condition of the liver called primary sclerosing cholangitis or with family members who have had colon cancer. All patients with ulcerative colitis should discuss the timing and frequency of colonoscopy with their gastroenterologist.
Surgery
Patients with ulcerative colitis may have symptoms in parts of their bodies outside of the digestive system.
Joints
There are forms of arthritis and back pain that are related to ulcerative colitis. Some of these conditions improve with medications for the digestive symptoms of ulcerative colitis. The use of over-the-counter pain medications such as ibuprofen, naproxen, and aspirin may increase the symptoms of ulcerative colitis. Patients with ulcerative colitis should speak with their gastroenterologist before using these medications.
Eyes
Skin
Other Complications
Duration And Evolution Of Pain In Ibd
Pain was a longstanding problem for the majority of the patients with 52% of patients experiencing pain > 5 years. Fifteen patients reported pain since < 1 month, 57 patients suffered from pain since 1 month½ year, 59 patients since ½ year 1 year, 79 patients since 12 years and 215 since 25 years . When comparing CD and UC 388 of the 556 UC patients reported pain in general. Of these the majority reported to suffer from pain more than 5 years. The 679 CD patients on the other hand also reported about pain in 71% of these a majority also suffered from pain > 5 years. When comparing the duration of pain statistically more UC patients only suffered from pain in the last 12 years compared to CD . For the other durations of pain there was no statistical difference .
Also Check: Diabetic Foot Ulcer Icd 10
Research And New Developments
Previous research has shown that ankylosing spondylitis has a strong genetic component and were currently funding several research projects to further understand this. Previously, we part funded research that identified a specific gene, called IL23R, thats linked to the condition. Were now funding a follow-on project to investigate how changes in this gene lead to the development of ankylosing spondylitis.
Were also supporting a study thats investigating a gene called RUNX3. Researchers are investigating whether this molecule can be targeted with drugs. Results from this research may lead to the development of new and more effective drug treatments.
Were funding a project investigating the protein HLA-B27. This protein is found in over 90% of people with ankylosing spondylitis. Its thought that HLA-B27 proteins tend to fold incorrectly inside cells, which may lead to the immune system releasing chemicals that cause inflammation. This research aims to generate HLA-B27 specific treatments that overcome the problems associated with current treatment options.
Pain As A Tool For Diagnosis
Because pain can come from different sources, and pain in the abdomen is particularly difficult to pinpoint, it is not a symptom that is normally used to diagnose IBD or a particular form of IBD.
Rather, the type and location of pain is more often used together with other signs and symptoms when diagnosing IBD or other conditions. In other words, it might be a starting point to help a healthcare provider know where to start looking for inflammation, but it’s only one part of the picture.
You May Like: How Long Does An Ulcerative Colitis Flare Up Last
Is Severe Back And Leg Pain A Side Effect Of My Ulcerative Colitis Or My Meds Asacol And Remicade
- Asked
- 23 Jul 2012 by Poopbuckets
- asacol, remicade, ulcerative colitis, colitis, pain, side effect, doctor
I’m on 4,800 mg Asacol and Remicade infusions . The pain is really bad . Should I ask my doctor for some sort of pain meds ? Was diagnosed dec 2011. My legs ache all night . My joints are stiff and achey knees are also aching.Keeps me up at night . Doc wanted to put me on prednisone but I refused . I’ll go see my family doc tomorrow.
If you are in severe pain for any reason, definitely talk to your doc. Pain is a symptom of a bunch of things. Your doc needs to be told ASAP and a determination will be made how to best proceed with your health care.Best wishes and hope you find the reason for your increased pain.Peace,
endlessPred
My GI doc said that if I have severe pain and even a little sign of blood to head straight for the E R. Last time I lost a lot of blood in a very short time. Pain and vomiting were first. You know your symptoms best, but they did ask me why I waited. I realized I wasn’t very smart about it. Four days in the hospital. They told me it was safer to come in and be sent home than guess wrong. Let me know how it goes.
The back and leg pain is from the pressure you are feeling, I think. If you are doubled over from pain, you belong in the hospital. Please do not wait.
+0HeadStarter
I wish you a smoother journey through this life and one that holds more hope, too.
jebnow+0Poopbuckets+0Poopbuckets+0sasha223+0adamblake21Bowskiter+0ckret23+0
Lower Back Pain With Ulcerative Colitis
Lower back pain and its relationship to inflammatory bowel disease has been talked about fairly often in our community. While there is no one reason for experiencing lower back pain , you are not alone if you experience this type of pain along with your Crohns disease or ulcerative colitis.
Before I continue, I want to reiterate that I am not a medical professional and if you are having this type of pain, I do highly suggest you bring it up to your doctor. There is often a reason for this pain that may require medical attention so I dont suggest waiting, if possible.
Recommended Reading: How Do Stomach Ulcers Heal
What Makes It Worse
The reasons why aren’t totally clear. Doctors don’t know why it affects only a small section in one person, but spreads through the entire colon in another. But certain triggers sometimes play a role. These include:
Food. It’s different for everyone, but certain foods can irritate your symptoms. For example:
- Caffeine can make severe diarrhea worse
- Dairy may lead to more diarrhea, gas, and pain
- Fizzy drinks can be a problem if you have gas
- Greasy and fried foods often lead to gas and diarrhea
- High-fiber foods, such as fresh fruits and veggies, whole grains, corn, nuts, and seeds, can be hard on you
- Spicy foods can be tough to handle
Stress. It can trigger flare-ups and make your symptoms much harder to deal with. It’s especially challenging because just having ulcerative colitis can bring on more of it.
Skipping meds. Even when you’re in remission, it’s very important to take your meds. In the best case, they prevent flare-ups. And even if not, they can help keep things under control.
Follow these 5 tips to help control your ulcerative colitis flare-ups.
Why Does Ulcerative Colitis Cause Joint Pain
As you can probably guess, the joint pain that occurs as a symptom of some type of Enteropathic Arthritis develops because of the inflammation caused by Ulcerative Colitis.
And no, the cause for this is yet to be found out. In normal circumstances, for some unknown reasons, inflammation occurs and affects some or more than one joint, what is later diagnosed as some type of Arthritis.
So it is not a different story this time it is still the inflammation that has first occurred because of the Ulcerative Colitis that has later only spread and affected some joints in the body, causing the common Arthritis symptoms to develop as well.
But the good news is that there are some promising suggestions for a colectomy to make the Arthritis symptoms, as well as the Ulcerative colitis symptoms, to go away.
Recommended Reading: How To Reduce Bloating With Ulcerative Colitis
Questions To Ask Your Doctor
- How will my inflammatory bowel disease be treated?
- Will I need surgery? Are there other options?
- What lifestyle changes can I make to help inflammatory bowel disease?
- What are some medicines used to treat inflammatory bowel disease and what are the possible side effects?
- Are my children at risk of inflammatory bowel disease?
Back Pain Often Comes Directly From Back Or Spinal Structures But Sometimes Its A Sign Of A Medical Condition Elsewhere In Your Body Heres What Else Could Be Causing Your Back Pain
Heres a scene that plays out every day, all over the world: Someone thinks they have a little back strain. Perhaps they lifted something wrong or moved the wrong way. It was just a twinge, so they waited it out a few days for the pain to go away. It doesnt, so they head to their doctor. Turns out, they hadnt lifted anything wrong at all. It was the start of a kidney infection, or a UTI, or pancreatitis.
Here’s how to tell the difference between a back strain and something more serious going on.
How do you know when the root cause of back pain is elsewhere in your body? There are two types of pain we look at, explains Matthew Crooks, MD, a pain specialist at Pinnacle Pain and Spine in Scottsdale, Arizona: visceral pain and somatic pain. Visceral pain is pain from an organ or internal pain that can radiate to the spine with conditions like pancreatitis, ulcerative colitis or Crohns disease, gall stones, cancers, kidney pain, and urinary tract infection, says Dr. Crooks.
Whats more, thanks to aging, injury, or a sedentary lifestyle, almost everyone has some wear and tear in the spine and pain in the musculoskeletal system . When you do develop visceral pain, it can flare up your somatic pain. And thats separate from the pain thats radiating from an organ, says Dr. Crooks. It can be activated from overall inflammation and the stress of the body dealing with the medical issue. Its the BOGO special that you never want.
You May Like: Can Ulcerative Colitis Go Into Remission