How To Prevent Diabetic Foot Ulcers
The first line of defense in preventing diabetic wounds is to follow the guidelines recommended to keep the disease itself under control:
- Maintain healthy blood sugar levels through a healthy diet and by taking medications as instructed by your doctor.
- Keep your blood pressure within a healthy range.
- Avoid alcohol and tobacco.
You should also take measures to avoid causing sores or wounds on the feet:
- Never walk barefoot.
- Wear shoes that fit properly and dont rub the skin.
- Wash your feet daily with mild soap and lukewarm water to prevent the buildup of bacteria on the skin, which can cause infection even in the tiniest skin breaks.
Because a loss of sensation in the feet may mean theres no pain felt even when an ulcer is present, its also extremely important for those with diabetes to regularly check for any foot sores or skin irritation. This way, the ulcer can be properly treated as early as possible.
Preventing A Diabetic Foot Ulcer
Holistic treatment of the individual with diabetes can help treat the underlying health issues and not only promote faster wound healing but also minimize risk factors that may have contributed to the development of a diabetic foot ulcer. Good diabetic control and lifestyle modification include:
- Keeping blood glucose levels optimal.
- Good nutrition and eating habits.
- Reducing high blood pressure.
- No smoking.
Individuals with diabetes should be instructed to:
- Examine their feet daily with a mirror and to look carefully for fungal infections or any abnormality.
- Wash and dry feet at least once a day in lukewarm water , paying special attention to dry between the toes.
- Not use heating pads or put feet close to heaters.
- Always use footwear inside and outdoors.
- Use close-toed shoes if they can’t feel their feet.
- Always use socks and change them daily.
- Have their nails cut carefully straight across by a trained professional .
- Treat dry feet with lubricants containing urea or salicylates, but don’t apply between toes.
In addition, every patient with diabetes should have a comprehensive foot exam yearly. Along with a careful physical exam, health care professionals should reinforce best practices of diabetic foot self-care at each visit to make sure the individual understands the recommendations and importance of caring for their feet.
Caution About Diabetic Foot Ulcer:
- Caution should be exercised in case of sudden pain and swelling of the legs, blisters, small sores, piercing of the feet, hot water or hot objects.
- If the toenails become thick and curved and enter the toes, if there is any structural defect in the toes. If you have a history of any previous wound on your feet, the sensation of the feet is so low that you do not feel the feeling of cold or heat, but you should be careful and seek medical attention. It is best to have your feet checked every three to six months.
- Wear flat, soft, hard-soled leather shoes instead of sandals when going out. So that no sharp object pierces the sole of the shoe and creates sores on the feet. I also want the size of the shoes to be right, so that it is neither big nor small.
You May Like: What Not To Eat With Bleeding Ulcers
Diabetic Foot Ulcer Home Treatment
A diabetic foot ulcer is an open wound that happens due to uncontrolled sugar levels in diabetes patients. It is a troublesome condition that hinders a person from carrying on their daily routines. The worst part about diabetic foot ulcers is that person may not even be aware of its growing seriousness due to the damaged sensation of the affected area.
If you suffer from this problem of a diabetic foot ulcer, here is a sigh of relief for you in the name of home treatments or remedies. Yes, there are things that you can try at home to treat diabetic foot ulcers to some extent.
Diabetes And Diabetic Foot Ulcers
According to the Centers for Disease Control , an estimated 30 million people in the United States have diabetes, including 7 million who are unaware they are living with the disease. The percentage of adults with diabetes increases with age, reaching a high of 25 percent among those aged 65 years or older, according to the Amputee Coalition. In addition to age, risk factors for diabetes also include diet, activity level, obesity and heredity.
Diabetes may be accompanied by other co-existing conditions such as blindness, heart disease, kidney failure or lower-limb amputation.
High blood sugar levels, poor circulation, immune systems issues, nerve damage and infection may contribute to a non-healing diabetic foot ulcer. Four to 10 percent of people living with diabetes will develop a foot ulcer. An estimated 15 percent of people with foot ulcers will experience a major amputation. Even more alarming, people with an amputation have a 50 percent mortality rate within five years.
There are several common factors of diabetic foot ulcers including neuropathy, peripheral arterial disease , deformities and Charcot foot. Neuropathy is a result of damage to peripheral nerves and often causes weakness, numbness and pain in hands and feet. Similarly, PAD is caused by narrowed arteries which reduces blood flow to the limbs. Charcot foot is a deformity that results from nerve damage in the foot or ankle, which may cause injuries to go untreated, leading to the breakdown of joints.
Also Check: How Do They Check For Ulcers
How To Care For Diabetic Foot Ulcers
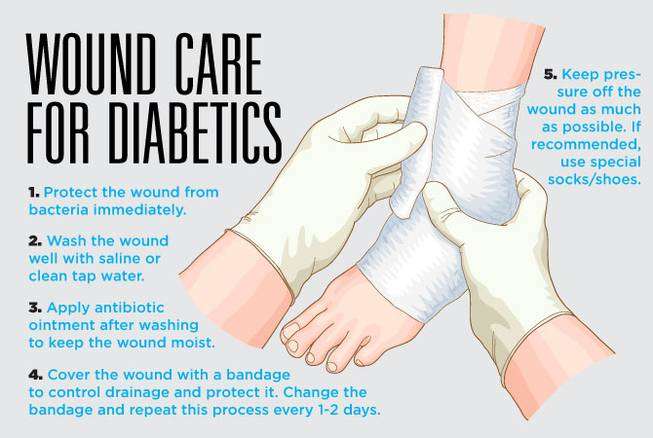
Here are some tips on how to care for diabetic foot ulcers:
- Keep the wound dry.
- Change the dressing every day.
- Change the dressing when it gets wet or dirty.
- Clean between the toes with a cotton ball each day, using soap and water. This is important for preventing infections between your toes, where it might be hard to see any signs of infection until it becomes very serious and causes deep problems for your feet.
- Keep the bandage dry and clean at all times change out for a clean and fresh dressing as needed .
Symptoms And Treatment Of Diabetic Foot Ulcers
It is important to recognize the symptoms of a foot ulcer, so you can seek treatment immediately. Some people with diabetes have decreased feeling in their feet that can cause them to not realize that they even have a foot ulcer. Some common symptoms of diabetic foot ulcers include:
- Visible open sore on the foot
- Pain and irritation
- Discharge or leaking from the sore
- Black tissue forming around the sore
- Foul-smell coming from the area of the sore
- Numbness
- Thickened skin near the sore
If you have an ulcer on your foot that is not healing or is getting worse, consult with your Keller wound care specialist. Your specialist can examine and evaluate your foot ulcer and recommend necessary treatment based on the severity of the problem.
Some wound care treatment options for a foot ulcer include:
Also Check: Wound Vac For Pressure Ulcers
Symptoms Of Diabetic Ulcers
Look for signs of bleeding or infection on or around the persons feet. Blood or discharge, an infectious odor, or sections with yellow discoloration can reveal that an infection has taken hold. If any areas have turned black, that indicates gangrene, or tissue death. The same rules apply if the infection is present in a different location, such as the hands, legs, or anywhere on the skin.
Diabetic Foot Ulcer Management Strategies
Effective treatment of DFUs starts with physical examination. Patients suspected of having the condition should be examined for signs of clinical presentation. Patients with peripheral vascular disease should immediately receive compression therapy to reduce their risk of developing DFUs. If an ulcer is found, the treatment focus should be on achieving rapid and complete wound healing. The wound should be regularly debrided to keep it free of non-viable tissue, and clinicians should select dressings that reduce bacterial load and provide an optimal healing environment.3
You May Like: Surgical Management Of Ulcerative Colitis Ppt
Advanced Therapies For Diabetic Foot Ulcers
Physicians of individuals with diabetic foot ulcers may have difficult decisions to make if wounds do not heal. Many of these patients have a significant cardiac risk and health care practitioners need to make complicated decisions about whether to perform invasive procedures like angiography. Other options can be:
- Covering the wound with cultured human cells.
- Heterogenetic dressings or grafts with recombinant growth factors.
- Hyperbaric oxygen therapy.
Visit A Doctor Regularly
Theres only one person who can give you special advice on how to best take care of your diabetic foot ulcer. He can give you medicine prescriptions, tips on how to make it better, and even offer to dress it for you. Also, he can notify you of changes and advise you on what to do. Note that though there are a lot of doctors who are an expert in the field of diabetes, only a few dwell so much into this type of condition, so choose your doctor well.
Also Check: Black Tarry Stools Ulcerative Colitis
Wash Your Foot With Hot Water
Make sure that the water is at a bearable temperature, otherwise, youll risk scalding the skin, and thats one more thing to worry about. As bacteria are not capable of surviving in very warm temperatures, washing your foot in hot water will surely cleanse them. Not only that, but the heat can also loosen the veins in your foot, regulating blood circulation.
What If A Diabetic Foot Ulcer Recurs Even After The Home Treatment

The aforementioned home treatments for diabetic foot ulcers usually work wonderfully. But in some cases, these ulcers tend to reappear again or get aggravated with another flare-up. In such cases, timely medical attention is a must for diabetic foot ulcers. To bring it to your awareness, diabetic foot ulcers can have serious health complications if you leave them untreated for a prolonged time.
So, reach out to a specialist doctor to discuss the treatment options for a diabetic foot ulcer. Depending upon the symptoms, the doctor will recommend the best-suited treatment.
Read Also: How To Treat A Diabetic Ulcer
Research Design And Methods
The data of the present study are derived from a large, prospective multicenter trial that compared a collagen/oxidized regenerated cellulose dressing with moistened gauze in management of diabetic foot ulcers. The methods and results of the study have been reported elsewhere . In brief, the trial was a multicenter study conducted in 11 U.S. sites it was a prospective randomized, controlled trial that was open label with a parallel study design. The study duration was 12 weeks. Patients were eligible for enrollment in the study if they had diabetes and a foot ulcer of at least 30 days duration with an area of at least 1 cm2 . All foot ulcers were uncomplicated by infection or ischemia.
Types Of Diabetic Ulcers
There are several types of diabetic foot ulcers
- Neuropathic ulcers occur where there is peripheral diabetic neuropathy, but no ischemia caused by peripheral artery disease.
- Ischemic ulcers occur where there is peripheral artery disease present without the involvement of diabetic peripheral neuropathy.
- Neuroischemic ulcers occur where the person has both peripheral neuropathy and ischemia resulting from peripheral artery disease.
Arriving at the correct diagnosis and identifying the cause of a diabetic ulcer is critical since it affects the treatment plan.
You May Like: What To Avoid With An Ulcer
How To Treat Ulcers
If you do get an ulcer or notice a change in your skin that youâre not sure about, tell your doctor right away. Youâll likely get a procedure called debridement, which removes unhealthy tissue from the wound to spur healing.
Your doctor will also work with you to try to keep your sore or ulcer from getting infected and becoming bigger. Some of the steps they may recommend include:
Clean your ulcer daily. Use soap and water, unless your doctor recommends another cleanser. Donât use hydrogen peroxide or soak your wound in a bath or whirlpool, because this could reduce healing and may boost your odds of infection.
Keep your ulcer bandaged or covered with a wound dressing. While you may have heard that itâs important to âair outâ wounds, experts now know that not covering a wound actually increases the odds of infection and slows healing.
Keep pressure off your ulcer, especially if itâs on your foot. This may mean you need to use crutches, special footwear, a brace, or other devices. Reducing pressure and irritation helps ulcers heal faster.
Use the topical medications your doctor recommends. These may be saline, growth factors, and/or skin substitutes.
Keep your blood sugar under control. In addition to reducing your risk of ulcers, tight blood sugar control helps your body heal existing ulcers.
Why Are People With Diabetes More Prone To Foot Ulcers
Diabetes increases a patients chances of having a foot ulcer. However, diabetics tend not to notice blood loss and wounds as quickly as those without diabetes because they are less sensitive to pain.
Often, this means that diabetics will suffer more tissue damage than normal because of a delayed reaction to the njury. Therefore, you may find that people with diabetes are more likely to need amputations on certain parts of their lower body. Fortunately, seeking proper diabetic foot ulcer care can help reduce your chances of needing amputation later in life.
You May Like: Low Residue Diet For Ulcerative Colitis
Keep Your Nails Clean
Whether you have diabetes or not, neglecting your toenails unclean and unhygienic. It is not advisable for diabetic patients to trim their nails. But dont let this be an excuse for you to go on with unclean toenails, as bacteria could easily reproduce and reach your wound, leading to infection. There are doctors who specialize in foot care called podiatrists, and they will help you keep your foot maintained and your foot ulcer safe.
Wound Care And Dressings
Care for your wound as instructed by your provider. Other instructions may include:
- Keep your blood sugar level under good control. This helps you heal faster and helps your body fight infections.
- Keep the ulcer clean and bandaged.
- Cleanse the wound daily, using a wound dressing or bandage.
- Try to reduce pressure on the healing ulcer.
- Do not walk barefoot unless your provider tells you it is OK.
Don’t Miss: What Are The First Signs Of A Stomach Ulcer
Preventing Diabetic Foot Ulcers
There are several ways to prevent a foot ulcer. In addition to daily checks of your feet for any signs of an ulcer or other abnormality, the following can be done to help with prevention:
- Never walk barefoot, and always wear socks to protect your feet
- Wear shoes that fit properly and do not rub
- Keep your blood sugar under control and monitored
- Eat a healthy diet
- Avoid alcohol and tobacco products
- Seek immediate medical attention if you have a foot wound that is not healing
Nonsurgical Treatment For Diabetic Foot Ulcers

To help a diabetic foot ulcer heal, doctors at NYU Langone clean and disinfect the area. If the ulcer is infected, your doctor prescribes antibiotics to clear it up and prevent it from traveling to a bone in the foot.
Your doctor can refer you to an NYU Langone vascular specialist for additional medication if you have lower extremity arterial disease, a condition that impairs blood flow to the legs and feet and can cause an ulcer to heal more slowly.
NYU Langone doctors recommend regular wound care for foot ulcers, as well as other therapies.
Don’t Miss: Food To Avoid For Ulcer Patient
Diagnosis And Treatment Of Diabetic Foot Ulcers
The primary goal in diabetic foot ulcer treatment is healing the wound as soon as possible. The faster the healing, the less chance exists for infection and amputation. There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Removing dead skin and tissue, called debridement
- Applying medications and/or dressings to the ulcer
- Prevention of infection
- Removing the pressure off the area, called off-loading
- You may be asked to wear special footgear such as a brace, castings, etc.
- Managing blood sugar levels and other health problems
- Adequate circulation
Not all ulcers are considered infected however, if your physician diagnoses an infection, a diabetic foot ulcer treatment program of antibiotics, wound care, and possibly hospitalization may be required.
Treatment Of Active Infection
Wound infection is a known predictor of poor wound healing and amputation. The appropriate recognition of infection and treatment with antibiotics in diabetic foot infection is imperative to improve outcomes. Conversely, inappropriately treating with antibiotics, often in the setting of fear of missing an infection, to reduce bacterial burden or prophylaxis is associated with several adverse effects, including antibacterial resistance. The IDSA has outlined specific guidelines for the treatment of diabetic foot infections. The IDSA recommends treatment of wounds with at least two signs or symptoms of inflammation or purulent secretion. It is recommended that, before antibiotic therapy, a deep tissue culture via biopsy or curettage after debridement be obtained. Swab specimens should be avoided, especially in inadequately debrided wounds. Antibiotic therapy should be targeted to aerobic Gram-positive cocci in mild to moderate infections. Severe infections should be treated with broad-spectrum empiric antibiotics pending cultures. IDSA recommends 1- to 2-week antibiotic course for mild infections and 23 weeks for moderate to severe infections, but antibiotics can usually be discontinued once clinical signs and symptoms of infections have resolved. To avoid antibacterial resistance and other adverse outcome of therapy, it is best practice that treatment of clinical diabetic foot infections be completed with narrow=spectrum antibiotics for the shortest duration possible.922
Read Also: Snack Ideas For Ulcerative Colitis
Caring For Wounds And Foot Ulcers In Diabetic Patients
The Centers for Disease Control and Prevention reports that there are 30.3 million people living with diabetes in the United States. Diabetes comes with many serious complications, including chronic wounds, nerve damage and foot ulcers.
The American Podiatric Medical Association reports that 15 percent of diabetic patients will develop a foot ulcer. Further, diabetes is the leading cause of nontraumatic, lower-extremity amputations in the U.S. caused by infected wounds and foot ulcers that cannot heal. While difficult to treat, foot ulcers often can be prevented.
Controlling risk factors and monitoring the skin daily is key to minimizing the negative effects of diabetes, said Nancy Estocado, Advanced Wound Care Clinical Coordinator at Sunrise Hospital and Medical Center. For anyone with diabetes, understanding how to prevent and properly address wounds especially foot ulcers is integral to living a healthy life.