Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compliance With Ethical Standards
Newcastle upon Tyne Hospitals and York Health Economics Consortium are funded by NICE to act as an EAC for the Medical Technologies Evaluation Programme.
This summary of the Medical Technology Guidance was produced following publication of the final guidance report. This summary has not been externally peer reviewed by Applied Health Economics and Health Policy. Seven of the authors work or worked for the EAC, but otherwise have no conflicts of interest. TO is an employee of NICE.
Hydrogel Dressings Consist Of A Starch Polymer And Up To 96% Water
Pressure ulcer prevention, operating room, wound dressing, friction. Managing sacral pressure ulcers with hydrocolloid dressings: Secondary outcomes were time to heal, ulcer area healed per day, linear healing of wound edge, and cost of therapy. Pressure ulcers will not heal by dressings alone, but need the pressure eliminated, . Treating the underlying cause will often address and promote wound healing. Analysis by intention to treat revealed . These dressings can absorb wound exudate or rehydrate a wound depending on . The use of duoderm® dressings has proven advantages to support wound healing. Dressing, nursing time, wound cleansing and debridements 8. Hydrogel dressings consist of a starch polymer and up to 96% water. Hydrocolloid is made for difficult to dress wounds. Hydrocolloid dressing reduce the risk of pressure ulcer .
These dressings can absorb wound exudate or rehydrate a wound depending on . Pressure ulcers will not heal by dressings alone, but need the pressure eliminated, . Hydrocolloid dressing reduce the risk of pressure ulcer . Pressure ulcer prevention, operating room, wound dressing, friction. The use of duoderm® dressings has proven advantages to support wound healing.
Recommended Reading: Diet For Gerd And Ulcers
Are There Lower Cost Alternatives To Mepilex Border Sacrum Dressings
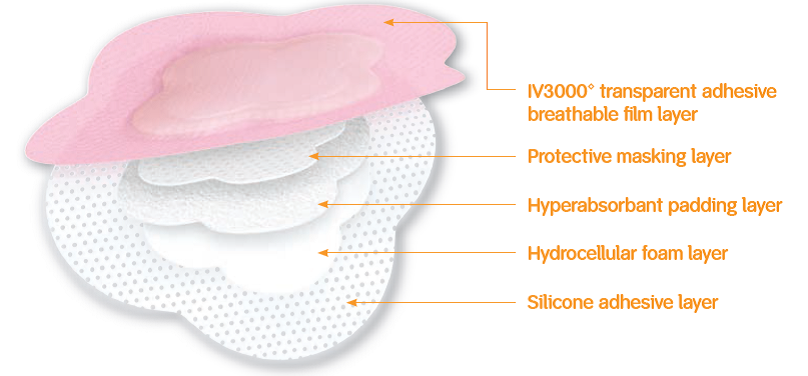
DeRoyal Polyderm GTL is a silicone foam sacral dressing with an adhesive border. Polyderm GTL protects wounds while reducing the risk of pressure ulcers and pressure related injury. Its gentle material and unique heart shape make this dressing ideal for the sensitive sacral area. The dressing conforms to the sacrum tailbone area of the body and provides protection. The foam core helps to absorb fluid from draining wounds. This helps avoid skin breakdown and protects healing skin. The dressing gently tapers at the edges to prevent it from rolling up off the skin. It can also be adjusted without weakening the adhesive. The top film of the dressing is water resistant and helps to block bacteria which helps the wound stay clean and heal faster.
What Causes Sacral Pressure Ulcers

Pressure ulcers occur when there is prolonged pressure to the skin, usually over bony areas such as the elbows, spine, or sacral area .
Compression of the soft tissue causes blood vessels to collapse and reduces blood flow and oxygen delivery. This localized tissue damage usually happens when a person sits or lays for long periods of time in a chair, wheelchair, or bed.
Pressure ulcers begin forming under the skin, making them difficult to catch before a wound is actually visible. So its important to take these steps to help prevent sacral pressure ulcers from happening.
Read Also: Nursing Care Plan For Pressure Ulcer Prevention
Background To The Indication And Devices
Pressure ulcers are localised injuries to the skin and/or underlying tissue as a result of pressure, or pressure in combination with shear . Pressure ulcers can range in severity and can be classified into the following categories or stages :
-
Stage 1 Intact skin with non-blanchable erythema of a localised area. Discoloration of the skin, warmth, oedema, hardness or pain may also be present.
-
Stage 2 Partial thickness loss of dermis presenting as a shallow open ulcer with a red/pink wound bed, without slough or bruising. It may also present as an intact or open/ruptured serum-filled blister.
-
Stage 3 Full thickness tissue loss. Subcutaneous fat may be visible, but bone, tendon or muscle are not exposed. Some slough may be present. It may include undermining and tunnelling.
-
Stage 4 Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. It often includes undermining and tunnelling.
Pressure ulcers can have a significant impact on a patients quality of life, both physically and psychologically. They can also lead to further health complications such as infection, extended hospital stays, restricted rehabilitation and restricted treatment options for other medical conditions .
All patients are at risk of pressure ulcers. However, Mepilex Border dressings have been indicated for use in people identified as either at risk or at high risk of developing a pressure ulcer.
Guy reports that risk factors for pressure ulcers include:
Silicone Adhesive Multilayer Foam Dressings To Prevent Pressure Ulcer
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : February 22, 2018Results First Posted : April 26, 2021Last Update Posted : April 26, 2021 |
- Study Details
The objective of this study is to determine if silicone adhesive multilayer foam dressings applied to the sacrum, heels and greater trochanter in addition to standard prevention reduce pressure ulcer incidence category II, III, IV, Unstageable and Deep Tissue Injury compared to standard pressure ulcer prevention alone, in at risk hospitalised patients. In particular, this trial extends previous trial results obtained in ICU setting. Therefore, only a maximum of 25% of patients will be recruited from ICU settings.
| Phase | ||
|---|---|---|
| Pressure Ulcer | Device: Allevyn® brand silicone adhesive multilayer foam dressingsDevice: Mepilex® brand silicone adhesive multilayer foam dressings | Not Applicable |
A multicentre randomised controlled open label parallel group medical device trial in approximately 8 hospitals in Belgium.
Patients will be randomly allocated to three study arms based on a 1:1:1 allocation:
Study arm 1 :
Study arm 2 :
Study arm 3 :
| Experimental: Study Arm 1 |
Recommended Reading: Worst Foods For Stomach Ulcers
Description Of The Condition
Pressure ulcers, also known as pressure injuries, bedsores, decubitus ulcers or pressure sores, are localised areas of injury to the skin, the underlying tissue or both. They often occur over bony prominences such as the sacrum and heel , and are caused by external forces such as pressure, or shear, or a combination of both .
Risk factors for pressure ulcer development have been summarised into three main categories: a lack of mobility poor perfusion and low skin status the latter category includes the presence of stage 1 pressure ulcers or incontinence or both, which also increases the risk of ulceration by producing a detrimental environment for the skin .
Prevalence
Pressure ulcers are one of the most common types of complex wound. Prevalence estimates differ according to the type of population assessed, the data collection methods used and period of data collection and whether Stage 1 ulcers were included).
One large European study estimated a hospital pressure ulcer prevalence of 10.5% whilst a US study estimated a prevalence of 9.0% across acutecare, longterm care and rehabilitation settings ). In the UK, national pressure ulcer data are collected across community and acute settings as part of the National Health Service Safety Thermometer initiative . About 4.4% of patients across these settings were estimated to have a pressure ulcer in November 2014 .
Treatments for pressure ulcers
Impact of pressure ulcers on patients and financial costs
Keep Skin Clean Dry And Moisturized
In addition to pressure, the sacral area is at risk for breakdown due to the potential for sweat and other body fluids to sit on the skin.
These sources of moisture cause irritation, and can result in maceration-or softening of the tissue. Because this weakens the skin, it can make the tissue more susceptible to sacral pressure ulcers forming.
To avoid this, ensure the area is completely cleaned and dried after any contact with sweat, urine, or stool. And to prevent wounds due to weakened or cracking skin resulting from dryness, apply a moisture barrier or moisturizing lotion as needed throughout the day.
Don’t Miss: Sample Meal Plan For Ulcerative Colitis
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Management Of Sacral Ulcers Varies By Ulcer Stage
It is important to properly stage pressure ulcers for several reasons, but two of the most important are for prognosis and management planning. Stage 1 and stage 2 pressure ulcers heal by regenerating tissue in the wound. Stage 3 and stage 4 pressure ulcers, on the other hand, heal through scar formation, which means the borders of the wound contract as it heals.
For Stage 1 sacral ulcers, the primary goal of therapy is to ensure adequate tissue perfusion and to protect the wound from further damage.2 This means preventing the sacrum from chronically squeezing the skin and preventing blood flow to the area. The goal of therapy for Stage 2 ulcers is to encourage tissue regeneration and protect the wound surface. For stage 3 or 4 ulcers, management efforts are focused on promoting tissue granulation and epithelialization.
Don’t Miss: Signs And Symptoms Of Peptic Ulcer
Is This Guidance Up To Date
Next review: 2022
NICE medical technologies guidance addresses specific technologies notified to NICE by sponsors. The case for adoption is based on the claimed advantages of introducing the specific technology compared with current management of the condition. This case is reviewed against the evidence submitted and expert advice. If the case for adopting the technology is supported, then the technology has been found to offer advantages to patients and the NHS. The specific recommendations on individual technologies are not intended to limit use of other relevant technologies which may offer similar advantages.
This guidance replaces NICE medtech innovation briefing on Mepilex Border dressings for preventing pressure ulcers .
Your responsibility
This guidance represents the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, healthcare professionals are expected to take this guidance fully into account, and specifically any special arrangements relating to the introduction of new interventional procedures. The guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer.
What Is A Sacrum Dressing
- To prevent pressure ulcers from forming
- To treat already existing medium to high exuding sacral wounds like pressure injuries and ulcers
- Mepilex border combines the ability to handle and retain draining fluid so exudate is managed with less risk of maceration or skin break down.
- Mepilex uses Safetac technology which reduces pain and tissue damage during dressing changes.
- Mepilex dressings with Safetac technology do not stick to the wound bed they seal the wound edge to prevent maceration, they don’t strip skin when removed while providing an optimal wound bed for quicker healing.
- Mepilex Border Sacrum dressing is an all-in-one foam dressing for pressure ulcers and other chronic and acute wounds of the sacral area.
Read Also: What Is The Best Treatment For Ulcerative Proctitis
When To Use Mepilex Border Sacrum
Treatment
Use Mepilex Border Sacrum for medium-to-high exuding sacral wounds, such as pressure ulcers or surgical excision of pilonidal cysts. The dressing maintains a moist wound environment, which supports debridement, so you might see an initial increase in the wound size. This is normal and to be expected.
Pressure Ulcer Prevention
A recent randomised controlled trial in the USA revealed a statistically significant effect of Mepilex Border Sacrum in reducing the incidence of hospital acquired pressure ulcers by 88% You can apply the dressing prophylactically for at risk patients , such as the immobile, those with poor skin perfusion and impaired skin condition, in emergency rooms, in intensive care, or before and during long surgical interventions. Scientific studies have demonstrated that Mepilex Border Sacrum has the ability to impact on four extrinsic factors that can contribute to developing pressure ulcers: by minimising and redistributing shear, redistributing pressure, reducing friction, and maintaining an optimal microclimate .
Note: the use of dressings as part of a prophylactic therapy does not preclude the need to continue to develop and follow a comprehensive pressure ulcer prevention protocol.
Factors That Influence Sacral Ulcer Management
While wound management is a key part of sacral ulcer management, treating patients holistically is the key to success. Apart from ischemia, other factors that impede normal healing include poor nutrition, infection, edema, persistent moisture, fecal and urinary soiling, and shearing forces. One can look for, prevent, or minimize each of these risk factors. Of course, the patient should be frequently repositioned to avoid further tissue damage and to promote healing.
When selecting a dressing, the wound should be kept moist but not contain excessive amounts of exudate. Wound care professionals should consider the type of ulcer and any comorbid conditions that could complicate treatment . Arterial wounds generally require a moisture-retaining dressing, while wounds that arise from venous insufficiency usually require a dressing that absorbs excess moisture. All surfaces of the wound, including any tunnels, should be packed with the appropriate dressing.
Also Check: What Is The Medication For Ulcerative Colitis
Where Is The Sacrum Area Of The Body
The sacrum area of the body refers to the area just above what is commonly referred to as the “tailbone”, this bony area is prone to pressure wounds. Anytime you have an area of the body with the underlying bones close to the surface of the skin you run the risk of developing a pressure sore in that area. Heels, elbows, sacrum, tailbone, etc. Pressure sores are difficult to treat because in order for treatment to be successful the pressure on the area must be relieved. If the area in question is your tailbone, it is difficult to remove pressure because anytime you sit or lay on your back you are adding pressure to the area. If you are recovering from illness or if you are using a wheelchair due to a spinal injury you will be seated or laying down often. Pressure sores do not take long to form and should be avoided by careful observation of at risk areas, proper rotation of the patient, cushions that relieve pressure like ROHO air cushions, and preventive wound care like the use of sacrum dressings.
+ Hydrocolloid Wound Dressing For Pressure Ulcers Png
Read Also
Hydrocolloid dressing reduce the risk of pressure ulcer . Treating the underlying cause will often address and promote wound healing. Managing sacral pressure ulcers with hydrocolloid dressings: Secondary outcomes were time to heal, ulcer area healed per day, linear healing of wound edge, and cost of therapy. Hydrogel dressings consist of a starch polymer and up to 96% water.
You May Like: Does Stomach Ulcer Cause Pain
Frequent Movement And Repositioning
Depending on factors like age and nutrition status, pressure can cause internal tissue damage within 2-6 hours. And skin can show signs warning of breakdown after as little as 30 minutes of prolonged pressure.
To prevent sacral pressure ulcers, its important to change positions frequently, whether its taking a walk, moving from bed into a chair, or even changing the level of recline in a seated position.
Research shows that 30 degrees of wheelchair tilt helps to reduce pressure in the ischial, buttocks, and sacral areas. And alternating side lying positions or using a wedge cushion while in bed can also help to limit the burden on these areas.
While theres not one single best position to prevent sacral pressure ulcers, you can reduce your risk by moving/shifting weight frequently and avoiding prolonged amounts of time sitting or lying in one spot.