Mild To Moderately Active Disease
Am J Gastroenterol.J Crohn’s Colitis.Gut.Cochrane Database Syst Rev.Am J Gastroenterol.J Crohn’s Colitis.Cochrane Database Syst Rev.Gut.
- Sninsky C
- et al.
Am J Gastroenterol.
- Lindgren S
- et al.
Gut.
- Dallaire C
- et al.
Can J Gastroenterol.
- Feagan BG
- et al.
Gastroenterology.Cochrane Database Syst Rev.World J Gastroenterol.J Crohn’s Colitis.Gastroenterology.BMJ.
Gut.Dig Dis Sci.N Engl J Med.
- Hommes DW
- et al.
Gut.
- Middleton S
- et al.
J Crohn’s Colitis.Am J Gastroenterol.
Clinical Presentation And Differential Diagnosis
Ulcerative colitis phenotypes by Montreal Classification
Extraintestinal manifestations can occur in about a third of patients with ulcerative colitis, and up to a quarter might have extraintestinal manifestations before inflammatory bowel disease diagnosis ., Peripheral arthritis appears to be the most common extraintestinal manifestation primary sclerosing cholangitis and pyoderma gangrenosum are more common in ulcerative colitis than in Crohns disease., The risk of venous thromboembolism in patients with inflammatory bowel disease is increased three to four times, and is greater when the patient is admitted with a flare or being treated with corticosteroids. Clinicians should have a high index of suspicion for venous thromboembolism, and hospitalised patients with ulcerative colitis should be prescribed venous thromboembolism prophylaxis.
Clinical Presentation Of Ibd
Crohns Disease and Ulcerative Colitis are chronic ongoing and life-long conditions in which symptoms vary from person to person and may range from mild to severe.
Symptoms may also change over time, with periods of good health when you have few or no symptoms alternating with times when your symptoms are more active .
THE MAIN SYMPTOMS OF IBD
-
Diarrhea. This is sometimes mixed with blood, mucus and pus
-
Cramping pains in the abdomen. These can be very severe and often occur before passing a stool
-
Tiredness and fatigue. This can be due to the illness itself, from anemia from the side effects of some of the drugs used for IBD or from a lack of sleep if you have to keep getting up at night with pain or diarrhea
-
Feeling generally unwell. Some people may feel feverish
-
Loss of appetite and loss of weight. Weight loss can be due to the body not absorbing nutrients from the food you eat because of the inflammation in the gut
-
Anemia . You are more likely to develop anemia if you are losing a lot of blood and are not eating much
-
Mouth ulcers
COMPLICATIONS
Some people with IBD, particularly Crohns Disease, may develop complications, including:
EXTRAINTESTINAL MANIFESTATIONS
IBD can sometimes affect other parts of the body, including joints, eyes and liver. Please refer to Extraintestinal Manifestations section for more information.
MANAGING IBD SYMPTOMS
You May Like: Foods That Cure Ulcerative Colitis
Infectious Colitis And Other Differential Diagnoses
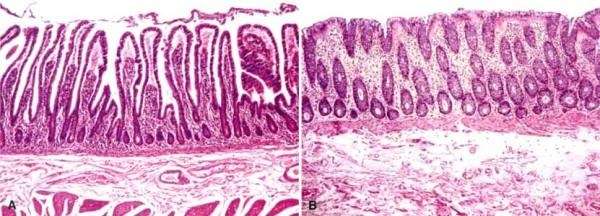
The differential diagnoses to CD and UC include chronic and acute intestinal infections, drug induced colitis and gastritis, graft-versus-host-reactions, ischemic colitis, vasculitis, intestinal lymphoma and other causes of chronic diarrhea such as microscopic colitis. Some of these have specific histological characteristics . Whereas others, such as infectious and drug induced colitis can show the same histological changes of acute and chronic inflammation as seen in IBD.
The diseases of microscopic colitis, that is lymphocytic colitis and collagenous colitis, are also considered a subtype of IBD. They cause chronic diarrhea, but are in contrast to UC and CD, characterized by a macroscopic normal mucosa, with some characteristic microscopic findings. Lymphocytic colitis is diagnosed by an increased number of intraepithelial lymphocytes , whereas a thickened subepithelial collagenous band of more than 10 µm defines collagenous colitis . Crypt architectural distortion is uncommon, and the distinction from UC and CD is often unproblematic. Drug-induced inflammation in the GI-tract can also be a histopathological differential diagnosis to IBD, sharing many of the same microscopic features. Colitis can be caused by a variety of drugs including but not limited to: non-steroid-anti-inflammatory drugs , checkpoint-inhibitors and chemotherapeutics. Here knowledge of clinical history is extremely important to avoid a misdiagnosis of IBD.
Dysplasia And Carcinoma In Ulcerative Colitis

About 3-5% of patients with ulcerative colitis will develop adenocarcinoma, and this outcome is thought to be the result of a progression of a precursor dysplastic lesion in most cases. Accordingly, screening endoscopy in ulcerative colitis patients focuses on dysplasia, a lesion that may be quite focal in its early presentation, despite what appears to be a clonal overgrowth of the chromosomally unstable cell population that ultimately exhibits dysplastic histology.
Hence, patients with ulcerative colitis will require screening colonoscopies more often than do patients without inflammatory bowel disease . The risk of malignancy in ulcerative colitis is definitely higher than in patients unaffected by idiopathic inflammatory bowel disease, and it also appears to be higher than the risk in patients without inflammatory bowel disease who have had multiple adenomas, adenomas with high-grade dysplasia, or a previous colonic malignancy.
The American College of Gastroenterology guidelines, updated in 2010, recommend annual or biannual surveillance colonoscopy after 8-10 years of colitis. Patients with primary sclerosing cholangitis are recognized to be at greater risk for colonic neoplasia than other ulcerative colitis patients are and thus should begin surveillance at the time of diagnosis of PSC and yearly thereafter.
You May Like: What Is The First Sign Of Stomach Ulcer
Pyodermatitis Vegetans Pyostomatitis Vegetans Pyodermatitispyostomatitis Vegetans
Pyodermatitis vegetans , a rare skin manifestation of IBD and often regarded as one of clinical forms of PG, has histopathology similar to pyostomatitis vegetans but with treatment similar to PG . PDV occurs mainly in skin folds such as axillary or inguinal area, but can also be present on the trunk or extremities. These lesions are characterized by pustules that quickly rupture, forming erosions with hemorrhagic ground, developing large raised well-demarcated plaques with surrounding pustules .
Pyodermatitis vegetans was first reported by Hallopeau when he described two patients with unusual pustular dermatosis and oral lesions for which he named pyodermite vegetans . McCarthy proposed the term pyostomatitis vegetans after he observed similar lesions isolated in the oral cavity . Recently these two entities are considered to be variants of the same disease termed pyodermatitispyostomatitis vegetans . PDV and PSV are rare cutaneous manifestation of IBD . In general, bowel disease antedate oral involvement by several years . The rash of PPV has been reported to correlate with underlying bowel disease activity . The pathogenesis of PSV, PDV, or PPV is not clear, but has been hypothesized to be due to aberrant immune responses in IBD to cross-reacting antigens in the skin and bowel resulting in mucocutaneous manifestations .
Biopsies All Submitted In One Bottle
COLON , BIOPSIES:- MODERATE CHRONIC ACTIVE COLITIS.- NEGATIVE FOR DYSPLASIA.- PLEASE SEE COMMENT.COMMENT:The sections show colorectal-type mucosa with focal cryptitis and rare neutrophilic cryptabscesses.Mild architectural changes, suggestive of a chronic colitis, are present. No granulomas areidentified. Lymphoid aggregates with germinal centre formation are present in multiplefragments. The lamina propria has abundant plasma cells throughout the fragments no fragments have apparent relative sparing. Paneth cells are present focally however, the significance of the paneth cells cannot determined as the biopsy sites are not known. The findings are compatible with inflammatory bowel disease and chronic active infectiouscolitides. Clinical correlation is suggested.
Don’t Miss: Low Residue Diet For Ulcerative Colitis
Ulcerative Colitis Vs Crohns Disease: How These Bowel Diseases Differ
It’s understandable if you confuse ulcerative colitis with Crohn’s disease. Both of these chronic conditions are a type of inflammatory bowel disease that targets the digestive system with painful and burdensome symptoms. They both cause stomach pain and cramping, an urgent need to move the bowels, diarrhea, and fatigue. And they both have two phases of activity: flares and remission. On the surface, it can be hard to tell these inflammatory bowel diseases apart.
When it comes to ulcerative colitis vs. Crohn’s disease, the key differences lie where they are located in the body.
Signs And Symptoms Of Ulcerative Colitis
Recognizing the symptoms of ulcerative colitis is your first step toward knowing when your disease is in a flare and when to seek medical attention.
The symptoms of ulcerative colitis vary from person to person and about half of all ulcerative colitis patients experience mild symptoms. If you experience any of these symptoms, consult your healthcare provider.
-
Loose and urgent bowel movements
-
Bloody stool
-
Persistent diarrhea accompanied by abdominal pain and blood in the stool
Also Check: How To Treat An Ulcer After Gastric Bypass
Panel: Major Differential Diagnoses In Diagnostic Examination Of Ulcerative Colitis74
-
Infectious colitis: bacterial, viral, fungal , mycobacterial, and Clostridium difficile
-
Ischaemic colitis
-
Medication-induced colitis
-
Crohns disease
-
Sexually transmitted diseases : Chlamydia trachomatis, Neisseria gonorrhoeae, herpes, and syphilis
-
If predominant symptom is diarrhoea and not bleeding: coeliac disease, microscopic colitis, lactose or other food intolerances, and irritable bowel syndrome
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your anus. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
Read Also: Mouth Ulcer On Tongue Remedies
A Close View On Histopathological Changes In Inflammatory Bowel Disease A Narrative Review
Lauge Kellermann1^, Lene Buhl Riis2^
1Department of Gastroenterology, Herlev Hospital, University of Copenhagen 2Department of Pathology, Herlev Hospital, University of Copenhagen , Denmark
Contributions: Conception and design: All authors Administrative support: None Provision of study materials or patients: None Collection and assembly of data: None Data analysis and interpretation: None Manuscript writing: All authors Final approval of manuscript: All authors.
^ORCID: Lauge Kellermann, 0000-0001-8554-3538 Lene Buhl Riis, 0000-0003-4669-3159.
Correspondence to:
Keywords: Histopathology histological remission histological index Crohns disease ulcerative colitis
Received: 12 January 2021 Accepted: 19 March 2021 Published: 30 March 2021.
doi: 10.21037/dmr-21-1
Clinical Management Of Uc Patients In Surveillance Program
Histological interpretation of surveillance biopsies plays an essential role in clinical management. There is unanimous agreement in the literature that the detection of flat HGD or a DALM with any degree of dysplasia carries a sufficiently high risk of prevalent CRC or short-term and high-risk progression to CRC to warrant immediate colectomy . The natural history of LGD is more controversial but, in two studies, LGD was associated with a 20% risk of prevalent CRC in patients who underwent immediate colectomy or colectomy within 6 months and 14.519.4% risk of progressing to CRC in patients who continued on surveillance alone . While outcome data are scarce for UC with changes indefinite for dysplasia, this diagnosis is associated with significant risk of prevalent HGD and significant progression rates to dysplasia and advanced neoplasia , suggesting that UC patients with this finding warrant close follow-up.
Conflict of interest: none declared.
Read Also: How Long Does An Ulcerative Colitis Flare Up Last
Secondary Cutaneous Manifestations Due To Adverse Effects Of Ibd Treatment
Skin manifestations from adverse effects can result in a broad range of secondary cutaneous manifestations, such as drug eruptions, urticaria, angioedema, hair loss, lichen planus, erythema multiforme, bullous dermatosis/reaction, StevensJohnson syndrome, acne, psoriasis and so on . The following are examples of drugs used in IBD treatments that can cause secondary cutaneous complications: 5-ASA, metronidazole, ciprofloxacin, azathioprine, 6-MP, methotrexate, cyclosporine, steroids, anti-TNF- agents, etc. .
Anti-TNF- agents have been used successfully in the treatment of IBD and psoriasis, but when treating IBD, anti-TNF- agents such as infliximab and adalimumab can paradoxically induce psoriasis lesions after the third or fourth infusion . The psoriasis lesions regressed after withdrawing the anti-TNF- agents in 16 out of 17 patients . Although there have only been 18 reported cases of anti-TNF induced psoriasis in the IBD population, but clinicians should still be aware of this potential side effect . It has been suggested that inhibition of TNF- induces over-expression of cutaneous IFN- which then causes predisposition to psoriasis . The treatment of psoriasis induced by anti-TNF- agents is cessation of the offending agents and topical steroid therapy .
Presence Of Cancer And Dysplasia
Patients with ulcerative pancolitis for more than 8 years are at increased risk of colorectal cancer, approximating 0.5% to 1% per year.57 Those persons with primary sclerosing cholangitis as a complication of their ulcerative colitis have been shown to have an even higher incidence of dysplasia and cancer. Colonoscopic surveillance with random and chromoscopic-directed biopsies has been recommended in patients with long-standing ulcerative colitis. An obstructing lesion and unresectable dysplasia generally warrant surgery. Historically, high-grade dysplasia and multifocal low-grade dysplasia were widely accepted as clear indications for colectomy because of the high rate of an occult malignancy within the colon.8,9 However, there are circumstances in which dysplastic lesions within a field of normal colonic mucosa can be adequately managed endoscopically.10 This is an evolving area of management that requires a clear understanding of the lesion itself, the patient’s disease course, and the comfort of the treating physicians.
Read Also: Best Way To Heal Stomach Ulcers
Epithelium Negative For Dysplasia
In normal colonic mucosa the crypts are straight tubular structures that are regularly distributed throughout the mucosa, arranged parallel to one another, and extend to touch the muscularis mucosae. Mononuclear inflammatory cells are present in the lamina propria but should not noticeably expand it. Neither neutrophilic inflammation nor cytological atypia are present .
The category of mucosa negative for dysplasia includes normal mucosa , quiescent colitis , chronic active colitis , and the resolving phase of ulcerative colitis . In all scenarios, there are either no cytological atypia or none beyond that expected for reactive changes.
Quiescent colitis refers to architectural abnormalities of chronic colitis in the absence of significant neutrophilic crypt injury. These changes include atrophy, irregularity and shortening of crypts, thickening of the muscularis mucosae, or metaplasia .
Ascending Colon Cecum And Appendiceal Involvement As Skip Lesions In Uc
Some patients with either subtotal or left-sided colitis may show patchy, mild, cecum and/or ascending colon chronic-active inflammation which may be falsely interpreted as CD due to the impression of segmental involvement . In fact, up to 65% of UC patients present initially with limited left-sided involvement, which may spread to involve more proximal portions of the colon in 2958% of cases . In one study by DHaens et al. of 20 patients with established left-sided UC, 6 showed a sharp demarcation between affected and unaffected portions of colon, whereas 14 showed a more gradual transition . The area of transition may appear somewhat patchy and give the false impression of skip lesions. Furthermore, 75% of the latter group of patients showed an area of inflammation in the cecum, primarily in the periappendiceal mucosa, that was separate in space from the distal inflamed segment. In a previous study by our group, 14 patients with both left-sided UC and pathologically confirmed patchy right-sided chronic inflammation were compared to 35 control patients with limited left-sided UC only . These two groups of patients showed similar demographic features, extra-intestinal manifestations, severity of disease, prevalence of extension to pancolitis, and natural history which suggests that patchy right-sided inflammation in patients with left-sided colitis has little clinical significance but should be recognized by pathologists to prevent a false diagnosis of CD in this setting.
Don’t Miss: Is Nexium Good For Ulcers
Indeterminate Colitis In Colectomy Specimens
When indeterminate colitis is defined by the pathological findings in the resected colon as originally suggested, with features overlapping between UC and Crohn’s disease, the incidence of pouch complications will lie between UC and Crohn’s disease. However, if indeterminate colitis is defined as colitis showing features not classic for either UC or Crohn’s disease, the incidence of complications and pouch failure will not differ from those in UC . Regardless of the exact definition of indeterminate colitis, if there are no pathological stigmata of Crohns disease in the biopsy and colectomy, or clinical evidence of Crohn’s disease, patients with indeterminate colitis should not be denied an IPAA procedure .
Prognosis And Predictive Factors
Although the overall risk of carcinoma in a patient with ulcerative colitis is 3-5% over the patient’s lifetime, this risk is not uniform across all affected patients: those with longstanding disease and pancolitis are at the highest risk. As noted earlier, dysplasia is a histologic risk factor for carcinoma, and high-grade dysplasia is usually an indication for colectomy.
Age at diagnosis, smoking status, and extent of disease may predict disease severity and progression over time. In addition, complications can occur and may be life-threatening. These include toxic megacolon, colonic perforation, sepsis, pulmonary embolism, disseminated intravascular coagulation, hemorrhage, hypoproteinemia, and severe electrolyte disturbances.
Also Check: How To Test For Ulcerative Colitis
Sporadic Adenomas Versus Dalms
Patients with ulcerative colitis may also have sporadic adenomas, which must be distinguished from the dysplasia associated with ulcerative colitis , because sporadic adenomas do not appear to carry the same implications for carcinoma risk in these patients. It is helpful for the endoscopist to submit biopsies of the flat “shoulders” of raised lesions specimens should be in separate containers and specifically labeled.
The absence of flat dysplasia near polypoid dysplasia is helpful for distinguishing sporadic adenomas from dysplasia that may involve endoscopically flat mucosa. If dysplasia is seen in an area of active disease and is flat, one may favor a DALM however, if the patient is in remission or if a polypoid lesion is seen in a noninflamed area without adjacent flat dysplasia, one may diagnose a sporadic adenoma, especially in an older patient who has had adenomas before.
Unfortunately, it often is not possible for the pathologist to make a specific distinction, because there may be insufficient sampling of flat mucosa near the polyp or because the pathologist may not have been provided with the endoscopic or clinical information.