Talk To Your Gastroenterologist And Your Obstetrician
UC doesnt usually affect a womans ability to become pregnant, unless there is scar tissue from surgery that blocks the fallopian tubes, according to the American Gastroenterological Association . If you do have scar tissue and are trying to conceive, in vitro fertilization may be an option.
While UC doesnt necessarily interfere with the ability to get pregnant, women with UC need to plan a pregnancy carefully. Thats because if you conceive during a flare, theres a chance your symptoms could worsen throughout the pregnancy.
If a woman is considering starting a family, we always like to have a discussion ahead of time to try to plan things as much as possible, says Bellaguarda. According to the data and studies that have been published, the best time to conceive for a woman is when shes feeling well and the disease is in remission.
According to Bellaguarda, women who become pregnant while in remission tend to have a much easier pregnancy than those who conceive while the disease is active. the chance of them having a flare is the same as if they were not pregnant, says Bellaguarda. Conversely, if a woman conceives during a flare, the disease is likely to remain active or worsen during pregnancy, according to the Crohns and Colitis Foundation.
Genitourinary Syndrome Of Menopause
Menopause is a transitional period that occurs in women due to hormonal changes. Menopause can lead to several syndromes, such as weight changes, mood fluctuations, and many more. This is something that occurs at a certain age in every woman. Genitourinary syndrome of menopause is a chronic condition that …
Is It Ibd Or Is It My Period
Some females have gastrointestinal symptoms around the time of their period. This can include symptoms like nausea, vomiting, or lack of appetite.
Other symptoms that occur with IBD include trouble sleeping, depression, feeling irritable, and aches and pains. It may be challenging to figure out when signs and symptoms arise from IBD and when they are related to the menstrual period.
However, its important to know if any symptoms in the digestive system are related to menstruation and not IBD. This way you can avoid changing medications unnecessarily if it turns out that symptoms are not caused by the IBD.
One study of 47 females who had IBD and 44 who did not, found that those with IBD had symptoms more often during their menstrual cycle. Some of the more common signs and symptoms included abdominal pain, nausea, and gas. However, the researchers note that IBD symptoms did not change much during this time.
Another study compared symptoms during menstruation. It compared 139 females who had IBD and 258 who did not have IBD. The researchers noted a number of symptoms, including irritability, nervousness, restlessness, headache, anxiety, nausea, vomiting, leg swelling, low back pain, constipation, excessive urination, abdominal pain, and fatigue were significantly more common in females who had IBD.
Don’t Miss: When Was Ulcerative Colitis Discovered
Menstrual Cycle And Ibd Flares: Whats The Connection
Inflammatory bowel disease is the umbrella term that describes two conditions involving chronic inflammation of the digestive tract Crohns disease and ulcerative colitis . Both Crohns and UC can impact a persons menstrual cycle in several ways.
Some people with IBD who menstruate may experience irregular periods or even stop menstruating due to the impact of flares on their hormonal function. On the other hand, IBD flares are also associated with worse premenstrual syndrome and worse menstruation symptoms such as cramping, pain, and bleeding. People may also have more severe Crohns and colitis symptoms during their periods.
If this describes your experience, the good news is that getting flares under control can often help you return to a regular menstrual cycle. Here, well explore the connection between IBD and menstruation, including how the two affect each other and how their symptoms can be managed.
Menstrual Periods May Aggravate Your Uc
More than half of women say their IBD symptoms get worse when theyre on their period, according to a study of more than 1,000 females published in January 2018 in the journal Inflammatory Bowel Diseases.
These symptoms may include increased frequency of bowel movements, more gas or bloating, or increased abdominal pain, says Emanuelle A. Bellaguarda, MD, an assistant professor at the Feinberg School of Medicine at Northwestern University in Chicago.
Experts arent exactly sure why women experience more symptoms during menstruation, but the Inflammatory Bowel Diseases research suggests it may be caused by hormonal changes. During menstruation, women produce more hormone-like compounds called prostaglandins, which cause increased contractions of the smooth muscles in the colon. This may cause gastrointestinal problems such as diarrhea and abdominal cramps.
The good news is that these symptoms dont necessarily lead to a flare or increased inflammation, says Dr. Bellaguarda, and they should subside after your monthly period. I reassure my patients that theyre not experiencing a flare every month, she says.
Read Also: Best Diet For Peptic Ulcer
How Your Period Affects Your Digestive Tract
So, why do some people experience a worsening of GI symptoms during their period? More research is needed, but some evidence suggests that fluctuations in hormones throughout the menstrual cyclesuch as estrogen, progesterone and prostaglandinsmay be to blame.
Prostaglandins, for example, are responsible for the smooth muscle contractions that help the uterus shed its lining during menstruation, so they may also trigger muscle contractions in the intestines, according to Freeman. Other data says that, among those with slow-transit constipation, progesterone receptors in the GI tract may respond to fluctuations in prostaglandin levels.
Dr. Freeman adds, Even in women who dont have Crohns, there tends to be a prolonged GI transit time during the luteal phase of their cycle. That means you tend to have worsened gastrointestinal symptoms during this phase.
Growth And Development Problems For Children
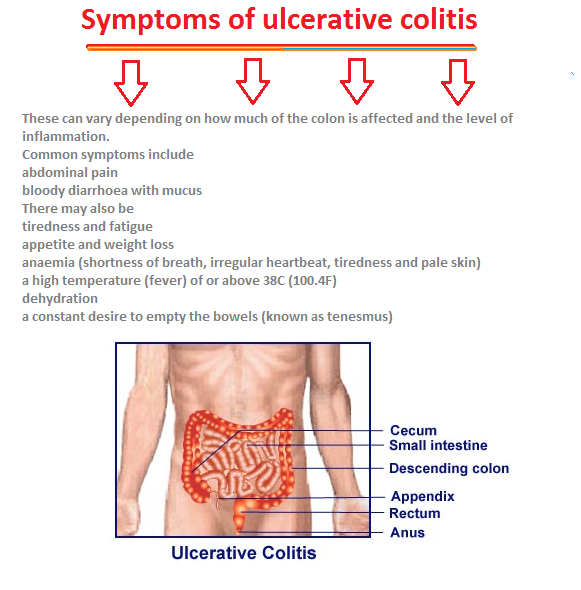
You can get ulcerative colitis at any age, but its more common among 15- to 30-year-olds. A child with UC may:
- Red or discolored
Continued
Talk to your doctor right away if youre worried that you might have DVT. Its possible for a deep-vein blood clot to break loose and get stuck in a lung artery. If that happens, its an emergency called a pulmonary embolism . You could have symptoms like shortness of breath, sharp chest pain, and a cough with or without blood. Call 911 if you have these signs.
Doctors can treat DVT and pulmonary embolisms with medications, a filter through a vein that removes the clot, or surgery.
You could be more likely to get DVT or PE if you:
- Have ulcerative colitis that flares often or affects a large amount of your colon.
- Get surgery for severe ulcerative colitis.
Some studies also link certain ulcerative colitis meds, like steroids or tofacitinib, to DVT and PE.
Don’t Miss: Things To Eat When You Have An Ulcer
What Are The Causes And Risk Factors Of Ulcerative Colitis
Ulcerative colitis is believed to be caused by an abnormal response by your bodys immune system.
Your immune system is supposed to defend you against harmful invasive bacteria and viruses. But in some people, the immune system mistakenly attacks the bodys own tissue.
While we dont know exactly what causes ulcerative colitis, there are two leading theories:
Experts believe that ulcerative colitis develops because of a combination of environmental factors and genetic predisposition.
Fatty cold-water fish such as mackerel, tuna, salmon, sardines, and herring are rich sources of omega-3 fatty acids.
Editorâs Picks
Also Check: What Foods To Eat When You Have Ulcerative Colitis
Is Your Ibd Messing With Your Periods A Gastroenterologist Says Yes
If you have inflammatory bowel disease , talking about topics that other people may find embarrassing has probably become quite natural for you. It may have been a challenge at first, but giving your doctor detailed accounts of your bowel habits is now as effortless as discussing the weather.
While the focus of IBD symptoms and treatment tends to be on the digestive system, if youre a woman living with IBD, its important for women to also understand the effect IBD can have on the menstrual cycle. Many women think that their gastroenterologists do not want or need to hear about their periods, but this could not be further from the truth!
David A. Schwartz, MD, FACG, Gastroenterologist and Director of the Vanderbilt University Inflammatory Bowel Disease Center, has helped answers your most pressing questions about the role IBD plays in puberty and the menstrual cycle.
Can IBD delay puberty?
Before we dive into the effects of IBD on the menstrual cycle, lets talk about how IBD can influence the start of puberty.
According to Dr. Schwartz, active IBD can lead to a delayed onset of puberty.4 Researchers found that the average age of a girls first period was 12.6 years old for those with IBD compared to 11.1 years old for those without IBD .4
Dr. Schwartz also highlighted that when scientists focused on women with Crohns disease , they found that the average age of their first period was 13.9 years old .7
Can IBD mess with my menstrual cycle?
References
Recommended Reading: What Can I Eat Ulcerative Colitis
Inflammation From Ulcerative Colitis
It seems that arthritis, or inflammation of the joints, is a common IBD complication. This problem limits ones mobility and potentially causesdaily pain that, in turn, affects work, exercise, or life in general.
For me, I detect it most at night. The throbbing pain awakens me many times throughout each night. If I lie in certain positions too long, my elbows shoot pain up my arms. Often, it hurts to move and stretch my arms out fully. Sometimes, my fingers and elbows seem to be at war with one another as in which area wants to cramp and hurt the most.
But this pain doesnt just occur at night. During the day, I also experience the aches, screams, and complaints of my elbows, ankles, and fingers. I never even realized the connection between my IBD and joint pain until a friend of mine with Crohns happened to mention it one day.
In my head, I thought, Really? As if a life of bloating, gut pain, diarrhea, and rectal bleeding arent enough with colitis? So, my online investigation on the connection between joint pain and ulcerative colitis began.
Ibd And Irregular Periods
An irregular period is when the timing of the menstrual cycle is out of what is considered the normal range of variation. That could mean having periods that are sometimes closer together or sometimes further apart.
Irregular periods are a reason to see a healthcare professional. The three times when an irregular period may be on the spectrum of normal are:
- The first year or two after menstruation starts
- During perimenopause
- After a miscarriage, pregnancy termination, or giving birth.
In one study of 121 females, researchers used a type of survey called the Inflammatory Bowel Disease Questionnaire to understand how their periods affected them. The IBDQ is often used in clinical studies and helps researchers understand how IBD is affecting a person’s quality of life, with low scores correlating with a lower quality of life.
The researchers found a connection between IBDQ scores and irregular cycles.
- Those people who said their menstrual cycle was fairly regular had lower IBDQ scores than those who said their cycle was regular.
- People who said their cycles were irregular also had lower IBDQ scores when compared to those who said their cycle was fairly regular.
Also Check: Ulcerative Colitis And Inflammatory Bowel Disease
Higher Risk Of Iron Deficiency
People who menstruate and live with UC may face an increased risk for anemia.
IBD, including UC, increases the risk of iron deficiency and anemia. According to research from 2018, as many as 45 percent of people with IBD have anemia.
UC can put you at risk for iron deficiency anemia for several reasons:
- The long-term irritation and swelling in your intestines can interfere with your bodys ability to absorb iron as well as other nutrients.
- You might not tolerate foods that are high in iron.
- You might have low appetite.
- Intestinal bleeding from ulcers causes blood loss.
The risk of anemia is even higher if you have a heavy period. Losing a lot of blood during your flow can use up more red blood cells than your body can produce, thus reducing your iron stores.
If you have UC and a heavy flow, you may want to look out for symptoms of anemia, including:
- skin that looks paler than usual
- shortness of breath
- faster or slower heart rate
- irregular heart rate
- cold hands or feet
While mild anemia is usually easily treated, more severe cases can lead to serious health consequences and can sometimes be life threatening. Talk with a doctor if you experience symptoms of anemia or iron deficiency. They can check your iron levels and provide treatment recommendations, if necessary.
Univariate Comparison Of Muscle Strength Physical Performance Tests And Habitual Physical Activity Between Uc Patients And Controls
The results for HGS, QS, ST, GS and the HPA evaluation for UC patients and controls are summarized in . QS was significantly decreased in UC patients compared with controls . UC patients were significantly slower than controls at the ST and at the GS test . In addition, HPA levels were significantly decreased in UC patients compared with controls . There was no significant difference in HGS between both groups.
Also Check: Why Did I Get Ulcerative Colitis
Recommended Reading: Alginate Dressings For Treating Pressure Ulcers
How Does Uc In Men & Women Differ
Inflammatory Bowel Disease affects differently based on the gender of the patient. Even though it sounds unfair, it is true.
The symptoms remain the same among both men and women, the latter have to face a few additional challenges with the disease. The major challenges include anaemia, change in the menstrual cycle, sexual pain, pregnancy complications. The reason for this high intense pain when compared to males is due to the shorter distance between the digestion and reproduction system.
In this article, we are going to discuss the various complications of ulcerative colitis in women and how to overcome them with a natural and healthy lifestyle.
Changes In Menstrual Cycle
Menstrual abnormalities. In a survey of women with inflammatory bowel disease, 60% reported having menstrual abnormalities.1 The abnormalities included very heavy bleeding and irregular cycles.1 In theory, the stress of having a chronic disease, surgery, or difficulty eating a balanced diet could cause changes in your cycle.4 However, very little research has been published about this.
In another study, 176 women were asked about changes in their menstrual cycle in the year before they were diagnosed with IBD.3 About one-quarter reported changes in the length of their cycle. Another 20% reported that the number of days of menstrual flow changed. There was no consistent pattern to the change in cycle length and flow duration. Some women reported an increase and others reported a decrease. About 40% of women reported pain during their period. Of this group, one-third reported that it had gotten worse before their diagnosis. The women in this study reported that over time, their cycles became much more regular.
Changes in menstrual symptoms. Menstrual symptoms have not been well studied in women with IBD. One small study showed that there was no differences in premenstrual symptoms overall.6 However, certain symptoms were more common in women with inflammatory bowel disease than in the comparison group. These symptoms were headaches, anxiety, depression, and breast pain.
Don’t Miss: Does Ulcerative Colitis Increased Risk Of Colon Cancer
Ibd And Period Irregularities
Normally, a woman gets her period every 28 days, give or take about 4 days.4 A womans first period is typically between ages 8.5 and 13 years. Women continue to have a period until menopause. The average age at menopause is 51 years.
Delayed puberty. On average, girls with IBD go through puberty later.5 In one study, nearly three-quarters of girls with Crohn’s disease got their period at or after age 16 years. Inflammation and difficulty with weight gain are some of the reasons why puberty is delayed.5
Socially, it can be difficult to go through puberty later than your friends. Delayed puberty also has an effect on growth and bone health. Hormone changes cause a growth spurt just before you stop growing.5 If you go through puberty late, you may have less of a growth spurt.5
Inflammatory Bowel Disease Affects Menstrual Cycles And Symptoms
For women, having inflammatory bowel disease such as Crohn’s disease may intensify menstrual symptoms such as PMS and cramps, and medication used to treat Crohn’s can unfortunately result in irregular menstrual cycles, and over-the-counter pain relief drugs often used for cramps are not recommended for people with IBD. The topic has been the subject of research led by Sumona Saha, MD, MS, associate professor , Gastroenterology and Hepatology.
An article in Everyday Health quoted study led by Dr. Saha in 2014. The study found that women with IBD often had more intense menstrual pain, heavier periods, and were more likely to experience irregular periods than women without IBD.
We know that there are estrogen and progesterone receptors in the GI tract, and this may explain why women are subject to GI symptoms around the time of their period, said Dr. Saha.
Not all women with IBD experience an increase in menstrual discomfort or pain about 13 percent were found to have worsened symptoms in the year prior to diagnosis. Were not clear on why some women have heightened symptoms and other women dont, said Dr. Saha.
Recommended Reading: What Is A Good Diet For Ulcerative Colitis
Ulcerative Colitis And Your Menstrual Cycle: Whats The Link
Curated by Claudia Shannon / Research Scientist / ishonest
More than 750,000 people in North America live with ulcerative colitis , an inflammatory bowel disease that causes inflammation of the lining of the large intestine.
Most people with UC and other types of IBD are diagnosed between the ages of 15 and 35 often the peak reproductive years. And while the condition is known for affecting the colon, it can also impact the reproductive system, including menstrual cycles.
Heres what you should know about UC and menstruation.