What Are The Complications Of Bedsores
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
Search Methods For Identification Of Studies
Four existing Cochrane Reviews were relevant to this NMA , and the protocol for this NMA complemented the protocols for these four reviews . We automatically included trials from these reviews in this NMA if they reported complete healing outcomes we planned to use the extracted data from these reviews where possible, supplementing if necessary which was required as some reviews had not been completed.
We conducted searches to identify relevant trials not covered by the four Cochrane Reviews as well as recently published trials. We crosschecked the identified trials against those in the 2014 NICE guideline and the 2013 US Agency for Healthcare Research and Quality guideline on treating pressure ulcers to further locate any additional trials we also checked the references of 24 systematic reviews identified by our search.
Electronic searches
We searched the following electronic databases to identify reports of relevant randomised clinical trials:
- the Cochrane Wounds Specialised Register
- the Cochrane Central Register of Controlled Trials
- Ovid MEDILINE
- EBSCO CINAHL Plus .
We also searched the following clinical trials registries:
- ClinicalTrials.gov
- WHO International Clinical Trials Registry Platform
- EU Clinical Trials Register .
Searching other resources
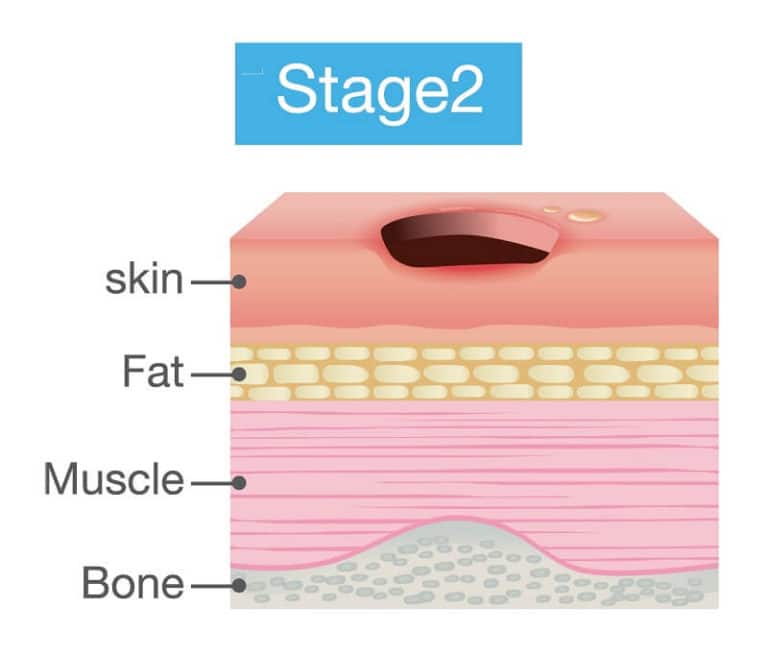
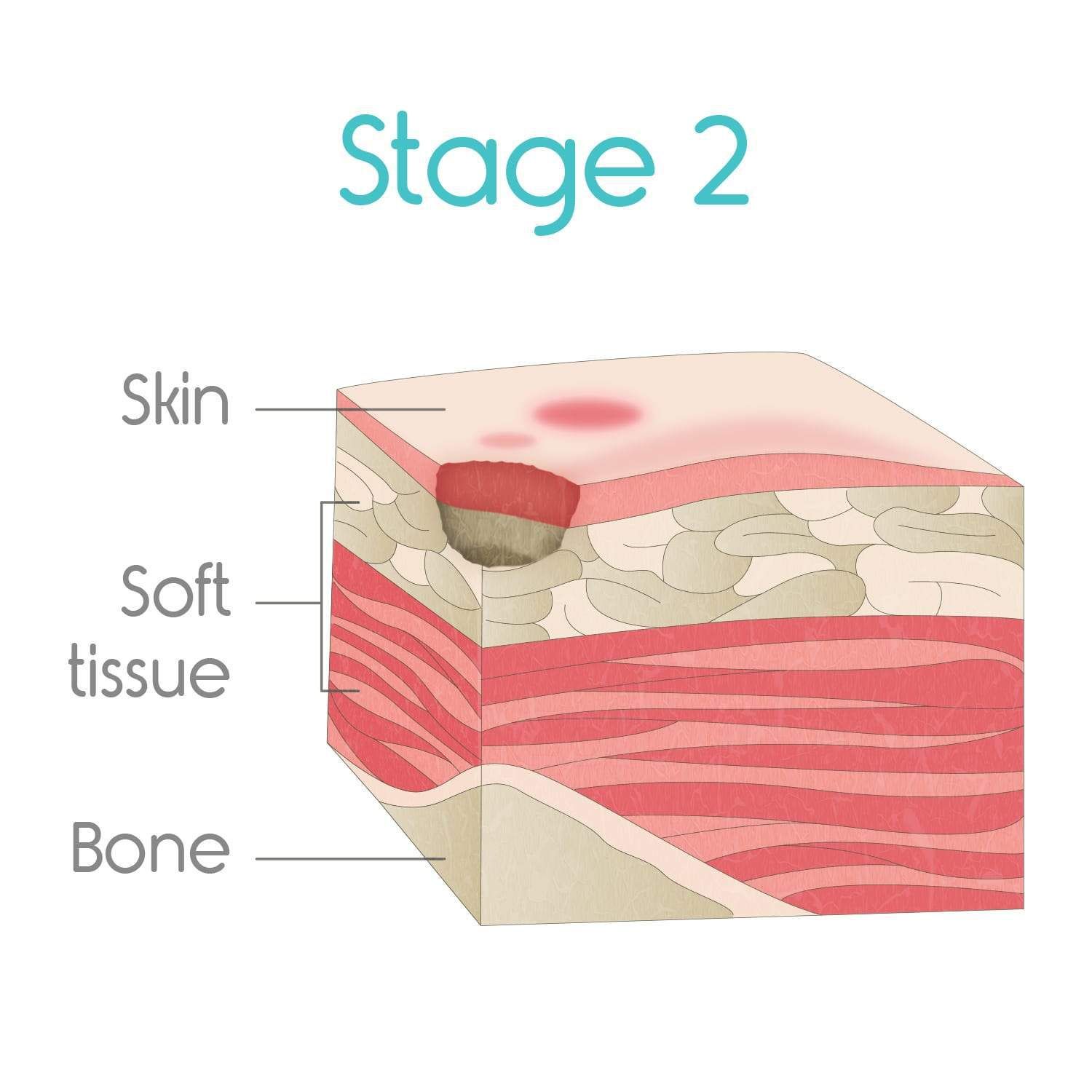
Stage 2 Bedsore Treatment
The Model Systems Knowledge Translation Center encourages people with stage 2 bedsores to see a health care provider as soon as possible.
Treatment for stage 2 bedsore typically involves:
- Bandaging: Bandages help keep bedsores dry and reduce the risk of infection.
- Cleaning: Doctors may use a saltwater solution called saline to clean the open wound when bandages are changed.
- Debriding: The Mayo Clinic notes that damaged and dead tissue must be removed so the bedsore can heal properly. This process is known as debridement.
- Getting Good Nutrition: The MSKTC recommends a diet rich in vitamin A and C, protein, zinc, and iron as part of a stage 2 bedsore treatment plan. Drinking enough water is also important. Johns Hopkins Medicine found that bedsores wont properly heal without these dietary changes.
- Reducing Pressure: Taking pressure off the bedsore will prevent it from getting worse and allow the skin to start repairing itself.
Seek medical advice from trusted doctors or nurses to learn more about treating pressure sores.
Don’t Miss: How To Heal Stomach Ulcers Naturally
Treatments Your Physician May Prescribe
In addition to self-care, your doctor might prescribe special pads or mattresses. Special dressings may be used, and whirlpool baths or surgery may be recommended to remove dead tissue. Infection requires antibiotic treatment. Sometimes deep wounds may require surgery to restore the tissue. Experimental work is now being done using honey preparations, high-pressure oxygen, and application of chemicals that stimulate cell growth .
Recommended Reading: Can You Drink Ensure With Ulcerative Colitis
Diagnosis Of A Decubitus Ulcer
Wound care physicians and nurses experienced in pressure ulcers are often consulted for decubitus ulcer diagnosis. Medical personnel may take samples of the pressure ulcer tissue and fluid to look for bacteria or cancer. They may also do blood cultures, bone scans or other tests depending on the seriousness of the ulcer. In addition, they will evaluate the condition of the ulcer according to:
- The size of the decubitus ulcer and depth of the crater
- What kind of tissue is affected by the ulcer: skin, bone, or muscle
- The color of the ulcer and skin around it
- The tissue death caused by the ulcer
- The presence of infection, bleeding or foul odor
Recommended Reading: Pressure Ulcer Prevention Care Plan
Who Is At Risk Of A Pressure Ulcer
People immobile due to illness or injury are at greatest risk of getting a pressure ulcer.
- They may be unable to change position without assistance eg, see Skin complications of paraplegia and tetraplegia.
- They may have nerve damage from injury or illness, such as spina bifida, diabetes or stroke, and are unable to sense pain or the signals that normally make people move.
- Older people are at greater risk because their skin is thinner and more fragile.
- A pressure ulcer may develop underneath a plaster of Paris or fibreglass plaster .
Stage 2 Bedsore Prevention
Stage 2 bedsores can be prevented if stage 1 bedsores are treated early on. This involves removing pressure from the bedsore, cleaning and drying it, and seeking medical care if it doesnt clear up in 2-3 days.
Family members or loved ones can look for stage 1 bedsores marked by discolored, painful patches of skin when visiting a nursing home resident. Nursing home residents can also prevent stage 2 bedsores by noting signs or symptoms of stage 1 bedsores and voicing their concerns to caregivers.
If a resident believes that the staff members arent listening to their worries, they can talk to a trusted family member or long-term care ombudsman. The family may be able to intervene on the residents behalf, and ombudsmen are trained to resolve issues between nursing home staff and residents.
You May Like: Ulcerative Colitis Surgery Success Rate
How Can I Prevent Pressure Ulcers
Pressure ulcers can be avoided, but often you may need help. If you have difficulty moving, preventing pressure ulcers might require a team effort, involving your health team, carer or a family member.
To protect your skin and prevent pressure ulcers, the following will help:
- Keep active and move as much as you can .
- Eat a variety of nutritious foods, including plenty of fruits and vegetables.
- Drink plenty of fluids to make sure you are hydrated.
- Avoid smoking because this reduces blood flow to your skin.
- Avoid firm massage, especially over bony areas.
- Keep your skin dry as far as possible.
- If you feel any skin pain or a feeling of burning, tell your doctor.
There are several things that will help you care for your skin:
- Instead of soap, use a mild cleanser and dry the skin gently afterwards.
- Apply moisturisers if the skin is dry, flaky or seems to crack easily.
- Use barrier cream in skin folds.
- Use warm water when having a bath or shower.
It is important to move around as often as you are able. Continuous pressure on the same areas can lead to a pressure ulcer developing very quickly. The following may help you avoid this:
- Change positions in bed at least every 30 minutes and, if you can, stand up and walk around.
- If you cant stand, move as much as you are able for example, lean forward or move side to side in your chair for 2 minutes to take the pressure off your bottom and hips.
- Try to avoid slumping or sliding forward in your chair.
Causes Of Pressure Ulcers
Pressure ulcers are caused by sustained pressure being placed on a particular part of the body.
This pressure interrupts the blood supply to the affected area of skin. Blood contains oxygen and other nutrients that are needed to help keep tissue healthy. Without a constant blood supply, tissue is damaged and will eventually die.
The lack of blood supply also means that the skin no longer receives infection-fighting white blood cells. Once an ulcer has developed, it can become infected by bacteria.
People with normal mobility do not develop pressure ulcers, as their body automatically makes hundreds of regular movements that prevent pressure building up on any part of their body.
For example, you may think that you are lying still when asleep, but you may shift position up to 20 times a night.
Pressure ulcers can be caused by:
- pressure from a hard surface such as a bed or wheelchair
- pressure that is placed on the skin through involuntary muscle movements such as muscle spasms
- moisture which can break down the outer layer of the skin
The time it takes for a pressure ulcer to form will depend on:
- the amount of pressure
- how vulnerable a person’s skin is to damage
Grade 3 or 4 pressure ulcers can develop quickly. For example, in susceptible people, a full-thickness pressure ulcer can sometimes develop in just 1 or 2 hours. However, in some cases, the damage will only become apparent a few days after the injury has occurred.
Recommended Reading: Home Remedies For Oral Ulcers
Keep Skin Clean And Dry
- Bathe daily with mild soap and warm water and rinse and dry thoroughly. Pay particular attention to keeping the genital area and skin folds clean and dry.
- Immediately wash and dry skin and change clothing after any leakage of stool or urine.
- Avoid harsh soaps, skin agents with alcohol, and antibacterial or antimicrobial soaps. Do not use powders. Use a moisturizer that has been approved by your health care provider.
Hydrogel Dressings For Treating Pressure Ulcers
Background
Pressure ulcers, also known as bedsores, decubitus ulcers and pressure injuries, are areas of injury to the skin or the underlying tissue, or both. Pressure ulcers can be painful, may become infected, and affect quality of life. Those at risk of pressure ulcers include those with spinal cord injuries and people who are immobile or who have limited mobility such as some elderly people and people with acute or chronic conditions. In 2004 the total annual cost of treating pressure ulcers in the UK was estimated as being GBP 1.4 to 2.1 billion, which was equivalent to 4% of the total NHS expenditure. Pressure ulcers have been shown to increase length of hospital stay and the associated hospital costs. Figures from the USA suggest that pressure ulcer was noted as a diagnosis for half a million hospital stays in 2006 for adults, the total hospital costs of these stays was USD 11 billion.
Dressings are one treatment option for pressure ulcers. There are many types of dressings that can be used these can vary considerably in cost. Hydrogel dressings are one type of available dressing. Hydrogel dressings contain a large amount of water that keeps ulcers moist rather than letting them become dry. Moist wounds are thought to heal more quickly than dry wounds. In this study we investigated whether there is any evidence that pressure ulcers treated with hydrogel dressings heal more quickly than those treated with other types of dressings or skin surface treatments.
Don’t Miss: How Long Do Stomach Ulcers Last
Preventing Stage 2 Bedsores
The best way to prevent stage 2 bedsores is to identify stage 1 bedsores and treat them before they worsen. Stage 1 bedsores have not broken the skin and usually look like reddish or discolored spots on the body. Stage 1 bedsores usually can be cured within a few days while stage 2 bedsores can take a few weeks to heal.
Nursing home attendants and nurses should regularly check residents at risk for signs of developing bedsores. Caretakers should check patients skin from head to toe. These skin assessments should take place at least once a day.
Patients who are at high risk of developing bedsores should be checked as often as is reasonable. Those at risk are often elderly or have a health condition that limits their mobility. People are at higher risk of developing bedsores if they use a wheelchair, spend a lot of time in bed, or need assistance to move. Conditions that can raise the risk of developing sores include mental conditions like alzheimers and physical conditions like paralysis.
How Do You Treat Pressure Sores On The Buttocks
Pressure sores on the buttocks are treated by proper wound care and by repositioning to remove the pressure source, states ClinicalKey. Pressure sores on the buttocks are due to long periods of uninterrupted pressure on the skin, soft tissue, muscle and bone.
There are four stages of pressure sores, according to ClinicalKey. The first stage is redness of the skin, and the second stage is partial thickness skin loss involving the epidermis and dermis. The third stage is full thickness skin loss involving the subcutaneous tissue. The fourth stage involves muscle and bone.
Prevention is the most important factor in managing pressure sores, explains ClinicalKey. For necrotic, deep and poorly healing wounds, surgical debridement may be necessary. If infection of the soft tissue or bone is present, antibiotics are needed.
Pressure sore develop in people who are chair- or bed-bound, elderly patients, hospital inpatients and people with spinal cord injuries, notes ClinicalKey. Those who are more predisposed to developing pressure sores are patients with conditions causing poor wound healing, such as diabetes and nutritional insufficiency, and those with conditions causing low tissue oxygen tension. People with fecal or urinary incontinence are also more prone to developing pressure sores, as urine and feces act as skin irritants to break down skin.
Don’t Miss: Best Nsaid For Stomach Ulcers
Questions For Your Doctor
- What should I do if I or a loved one has pressure sores and is too heavy to move?
- Does an adjustable bed help reduce the risk of pressure sores?
- Can you die from an infected pressure sore?
- Is diabetic foot ulcer the same as a pressure sore?
- Can you get pressure sores from sitting in the same position in your job for longer than 2 hours at a time?
How The Intervention Might Work
Animal experiments conducted over 40 years ago suggested that acute wounds heal more quickly when their surfaces are kept moist rather than left to dry and scab . A moist environment is thought to provide optimal conditions for the cells involved in the healing process, as well as allowing autolytic debridement , which is thought to be an important part of the healing pathway .
The desire to maintain a moist wound environment is a key driver for the use of wound dressings and related topical agents. Whilst a moist environment at the wound site has been shown to aid the rate of epithelialisation in superficial wounds, excess moisture at the wound site can cause maceration of the surrounding skin , and it has also been suggested that dressings that permit fluid to accumulate might predispose wounds to infection . Wound treatments vary in their level of absorbency, so that a very wet wound can be treated with an absorbent dressing to draw excess moisture away and avoid skin damage, whilst a drier wound can be treated with a more occlusive dressing or a hydrogel to maintain a moist environment.
Some dressings are now also formulated with an ‘active’ ingredient .
Read Also: Could I Have A Stomach Ulcer
Compensation For Stage 2 Bedsores
You may be able to access compensation for stage 2 bedsores by taking legal action against a nursing home and its staff.
Nursing home compensation can help pay for:
- Medical treatments
Breaking News for Older Veterans: President Biden Signs The PACT Act
The vast majority of Americans are united in believing that older adults, especially veterans and their loved ones, should receive quality care and dignity from a grateful nation. Horrifyingly, we have documented the dangers of nursing home abuse of military veterans, shining a light in dark places to expose the truth. We rarely get toRead More
Elder abuse is considered a serious crime, but it often goes unreported. Older adults and their loved ones may be afraid that reporting abuse will lead to worse treatment. Thankfully, there are laws at both the federal and state levels to ensure punishments for elder abuse are carried out. Learn more about what to doRead More
Handling Abuse Allegations in Nursing Homes
Nursing home abuse is a serious claim that many people may feel uncomfortable making. However, because nursing home residents are usually frail and often cannot defend themselves, all allegations of abuse must be taken seriously. Learn how to handle abuse allegations in nursing homes and keep your loved one safe. Nursing Home Abuse Allegations: WhatRead More
Sores On Buttocks Cheek
The buttocks cheek is prone to skin infections that may be difficult to notice. Infection of the hair follicles also called folliculitis are common. Such infection will in most cases heal on their own without treatment. They may also spread causing boils which will require antibiotics to cure.
Sores on buttock cheek are likely to affect people who are bed bound. The sores can become quite severe leading to ulceration and a significant loss of skin around the buttocks. A number of causes that could lead to sores on buttocks include:
- Skin conditions such as rashes
Below are the pictures of how sores on buttocks look like
Recommended Reading: Boots To Prevent Pressure Ulcers
How To Prevent Pressure Ulcers On The Buttocks
The first article in this series identified what a pressure ulcer is and explained how pressure ulcers can form when pressure is applied to an area of the body over a long period of time. This pressure restricts the blood flow through the skin and tissue, starving the bodys cells of oxygen and causing them die and causing the skin and tissue around the area to break down.
The prevention and treatment of pressure ulcers is essential as they can range in severity from patches of discoloured skin to open wounds that expose the underlying bone or muscle and they can be painful, debilitating and life threatening.
Spotlight On Aging: Pressure Sores
|
Aging itself does not cause pressure sores. But it causes changes in tissues that make pressure sores more likely to develop. As people age, the outer layers of the skin thin. Many older people have less fat and muscle, which help absorb pressure. The number of blood vessels decreases, and blood vessels rupture more easily. All wounds, including pressure sores, heal more slowly. Certain risk factors make pressure sores more likely to develop in older people: |
Causes that contribute to the development of pressure sores include
Pressure on skin, especially when over or between bony areas, reduces or cuts off blood flow to the skin. If blood flow is cut off for more than a few hours, the skin dies, beginning with its outer layer . The dead skin breaks down and an open sore develops. Most people do not develop pressure sores because they constantly shift position without thinking, even when they are asleep. However, some people cannot move normally and are therefore at greater risk of developing pressure sores. They include people who are paralyzed, comatose, very weak, sedated, or restrained. Paralyzed and comatose people are at particular risk because they also may be unable to move or feel pain .
Friction can lead to or worsen pressure sores. Repeated friction may wear away the top layers of skin. Such skin friction may occur, for example, if people are pulled repeatedly across a bed.
-
Assessment of nutrition status
-
Sometimes blood tests and magnetic resonance imaging
You May Like: How Do You Prevent Ulcerative Colitis