More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Soothe Skin Irritation And Pain
Bouts of diarrhea often can bother your skin. Use moist towelettes for wiping. Follow up with a petroleum jelly ointment. Need more relief? Soak in a saltwater bath, which may ease soreness. Try acetaminophen for pain, but avoid NSAIDs, such as ibuprofen and naproxen. They can trigger flares and cause other problems.
3
Don’t Miss: Can You Get An Ulcer In Your Intestines
Treatment Of Ibd Complications
Treatment depends on the particular complication, but may include:
- complications caused by nutritional deficiencies vitamin and mineral supplements , changes to diet or a liquid diet in severe cases
- inflammation in other body areas usually ease when the bowel inflammation is controlled with medication
- fistulas small openings that often heal by themselves, with treatment to ease the inflammation. A person may need surgery to close a larger fistula. Abscesses may need antibiotics and surgical drainage
- intestinal obstruction in some cases, medical treatment to ease the inflammation will clear the obstruction. In severe cases, the person will need surgery
- toxic megacolon the person goes to hospital, and receives fluids and nutrients intravenously instead of by mouth, plus antibiotics and steroids to reduce inflammation. Sometimes, the doctor will remove the contents of the persons stomach with a slender tube . A ruptured bowel needs surgical repair or removal. In severe cases, the whole of the large bowel may need to be surgically removed.
Complications Caused By Nutritional Deficiencies

Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
Don’t Miss: What Should You Eat With Ulcerative Colitis
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Prediction Of Outcome And Surgical Therapy
In a recent population-based European study, the global risk of colectomy in UC was 8.7% over 10 years. Efforts have been made to identify patients who are at high risk of not responding adequately to pharmacological therapy. In Crohns disease, factors such as young age at first diagnosis, early steroid use, ileal disease, mucosal healing, and smoking were identified as important for developing disabling disease or for major abdominal surgery. Much less is known in UC. According to data from different population-based studies, including the recent 10-year data from the Norwegian IBSEN cohort, initial extensive colitis, elevated ESR and sclerosing cholangitis were associated with an increased risk of colectomy. In contrast, older age at disease onset and smoking reduced the risk of subsequent colectomy. In a prospective study evaluating 49 hospitalized patients with severe UC, patients treated with steroids and/or CsA, a stool frequency of > 8/d or 3-8 stools/d, and increased CRP on day 3 predicted the need for colectomy with 85% certainty. Further work to identify predictive parameters of refractory courses should help to prevent a delay in inevitable surgical therapy.
Emergency indications for surgery includes refractory toxic megacolon, perforation and continuous severe colorectal bleeding . In this situation the recommended operation is colectomy and ileostomy, leaving the rectum in situ, since reconstruction is not an option in the acute setting .
Don’t Miss: How To Treat Bleeding Ulcer In Stomach
Medical Management Of Crohns Disease
The severity of CD is more difficult to assess than UC. The general principles are to consider the site , pattern and activity of the disease before treatment decisions are made in conjunction with the patient.
An alternative explanation for symptoms other than active disease should be considered and disease activity confirmed before starting steroids. Individuals with CD have many investigations over their lifetime and imaging should not be repeated unless it will alter management or a surgical decision depends on the result.
Patients should be encouraged to participate actively in the decision to treat with high dose aminosalicylates, different corticosteroids, nutritional therapy, antibiotics, new biological agents, or surgery. Infliximab is considered in section 6.5.
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
Also Check: Nasal Cannula Pressure Ulcer Prevention
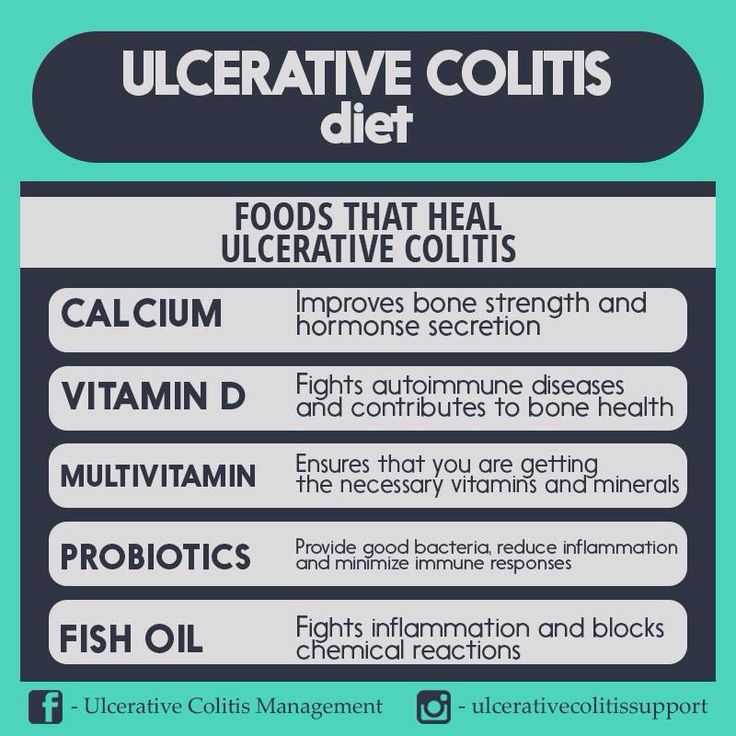
Vitamin And Mineral Supplements For Ibd
A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
Easing Symptoms During A Flare
The below suggestions can also help ease symptoms or help keep your body healthy during a flare-up.
Drink water: In UC, the large intestine can have a hard time absorbing water and salt, which can contribute to diarrhea and dehydration. Drinking plenty of water or an electrolyte replacement drink can help avoid dehydration if youre experiencing a flare.
Eat plain, easy-to-digest foods: During a UC flare, its common to lose your appetite. To keep your energy levels up and avoid malnutrition and weight loss, its important to continue to fuel your body with food. Unfortunately, fruits and vegetables, particularly when raw, are bothersome for many people with UC. Avoid fatty and greasy foods as well. Your doctor may also suggest meal replacement drinks if youre losing weight from UC flare-ups.
Get some exercise: If youre experiencing symptoms like stomach pain and diarrhea, exercise may sound like the last thing you want to do. But in addition to the well-known mood and health-boosting benefits of exercise, a workout can also have specific benefits for UC symptoms. Uncontrolled inflammation in the intestinal tract leads to UC symptoms. Exercise has an anti-inflammatory effect that can help these symptoms.
Also Check: What Can I Take For Ulcerative Colitis Pain
Read Also: Signs Of A Bleeding Stomach Ulcer
Why Working With A Qualified Care Team Is So Important When It Comes To Managing Ulcerative Colitis
People being treated for UC typically arent getting dietary or lifestyle advice, which is a huge disservice, says Cohen. But managing ulcerative colitis and preventing flare-ups can be done! You just might need a little help from the experts.
Because UC isnt one-size-fits-all and triggers are highly individual, enlisting the help of a care team like the clinicians at Parsley Health is wise. Providers can provide individualized supplement protocols based on lab testing, customized eating plans for periods of remission and flares, and communicate with your current GI doctor if necessary to streamline care.
Does Ulcerative Colitis Make You Immunocompromised

Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Read Also: Lion’s Mane Ulcerative Colitis
Recommendations For Cancer Surveillance
Patient with UC have an elevated risk of developing colon cancer. After 8-10 years of colitis, annual or biannual surveillance colonoscopy with multiple biopsies at regular intervals should be performed . Detection of high grade dysplasia in flat mucosa has to be confirmed by a second pathologist and is an indication for colectomy .
The sensitivity of random biopsies is a matter of debate and uncertainty as dysplasia in flat mucosa can be easily overlooked. Implementation of advanced endoscopic imaging techniques such as high-resolution white-light endoscopy, autofluorescence and narrow-band imaging may help to better identify pathological lesions and optimize cancer surveillance in inflammatory bowel disease in the future.
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
11
Don’t Miss: Good Foods To Eat With Stomach Ulcer
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
Home Remedies For Ulcerative Colitis Symptoms
Is there any cure for ulcerative colitis? If you are looking for solutions for ulcerative colitis, then you should not skip this article. Here, we will provide you with natural home remedies for ulcerative colitis symptoms which do not involve with medications or drugs. However, to be honest, natural remedies will not cure the inflammatory bowel disease , but they could alleviate the flare-ups and inflammation.
Basically, ulcerative colitis is considered the most common type of inflammatory bowel disease. Its symptoms may make mundane everyday activities rather daunting and might impact self-esteem, careers and relationships.
The following parts introduce to you basic information about ulcerative colitis, including what it is, what causes it, what common signs and symptoms are, what risk factors are, etc.
You May Like: Stress And Ulcerative Colitis Flares
How Much Prednisone Will I Take
The amount of prednisone your doctor prescribes will depend on your specific condition and the stage of your disease. You might get a high dose for a short time if youâre having a flare-up. Or your doctor may put you on a lower dose for what they call bridge therapy while youâre waiting for another medication to take effect. Many people take a low maintenance dose for a long time to keep inflammation levels in check.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Also Check: Can Ulcer Cause High Blood Pressure
Tips On How To Stop A Flare
Learning how to stop, manage, or decrease symptoms during a flare-up can help improve the quality of life of people with UC.
Although managing flare-ups is important, knowing what can trigger a flare-up can help stop one from happening in the first place.
Some of the following strategies may be helpful to implement.
How To Prevent Ulcerative Colitis Flare
What are actionable steps you can take to make your symptom-free stretches last as long as possible? and stress management are probably the two biggest things as far as prevention goes, says Cohen. Parsley Health providers and health coaches often work with members who have ulcerative colitis to find a diet that helps them minimize flares and a stress management routine. Below, well dive into some specific ways to optimize your diet with natural remedies and make adjustments to your lifestyle while living with ulcerative colitis.
You May Like: Diet For Crohn’s Disease And Ulcerative Colitis
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.