Stress And Psychological Disorders
Psychoneuroimmunological studies have shown mechanisms by which behavioural factors and emotions can influence inflammation and the immune system at both the systemic and local tissue levels.33 Although ulcerative colitis was called a psychosomatic disorder at the beginning of the 1950s, the renaissance of this aspect had come up in the past. Patients with remission of IBD are shown to have a considerably increased risk of exacerbation if they exhibit high scores for depression.34 These findings are supported by experience from daily clinical practice, as well as by prospective studies suggesting that emotionally negative life events can provoke relapses of ulcerative colitis.35,36 In contrast with these findings, no study has brought forward any evidence that therapeutic manipulation reducing stress in patients with IBD notably influences the number, duration, frequency or severity of relapses of ulcerative colitis.37 Obviously, welldesigned, prospective clinical investigations, assessing the relationships between life events and ulcerative colitis patterns, are difficult to carry out.
How Common Is Ulcerative Colitis With Constipation
Studies show 30%-50% of people with UC sometimes get symptoms of constipation. It seems more likely to happen in people who:
- Have left-sided colitis
- Have an active flare
- Are female
Constipation can happen to anyone. But it seems to occur less often in people with colitis throughout most or all of their large intestine. You may hear this called extensive colitis, pancolitis, or total colitis. If you have this kind of UC, youâre more likely to have frequent diarrhea or fast-moving stool.
Id Like To File A Complaint Against Ulcerative Colitis
Let me be the first to say that Im all about finding the glass-half-full perspective on any situation. It took a lot of therapy to get to this point, but when I focus on the silver linings and sunshine over the clouds, it makes the hard stuff feel more liveable. This isnt to say Im walking around dishing out toxic positivity rather, I prefer to find the deeper purpose in things that happen for me, not to me.
However, when you live with a chronic illness like ulcerative colitis , this proves to be easier said than done on some days. I recently gave birth to my son via an unplanned C-section, and Im still experiencing some post-surgery gut struggles nearly six weeks removed from the procedure. So let me start my formal complaint here: Every time I have a grumbling stomach, I think its flare number three coming to my door. Call it a form of PTSD from two previous flare-ups or whatever makes sense for you the reality is that any stomach issue equals flare fear for me. So Im walking around in my life not only waiting for that shoe to drop, but also believing my fear has come to life every time I get a normal stomach pain.
Read Also: Best Dressing For Decubitus Ulcers
New Treatments And Expanding Interest
In the decades following 1909, the medical community’s understanding of UC grew in leaps and bounds. This period included Lewisohn’s detailed demonstrations of familial predisposition Hewitt’s association between UC and polyps and Wangensteen’s recognition that it heralded colon cancer. The first report of UC in children came in 1923 by Helmholz, which included children from ages 8 to 15. Advances in treatment, such as ileostomy and blood transfusion were proposed and then validated as therapeutic measures useful for patients with UC.
Initially, surgical treatment of UC was sporadic and mostly experimental. But after 1930, surgical interventions for UC gradually became standardized. Several of these techniques were later abandoned, but a few are still in use today. Surgical therapies that were eventually discarded include: therapeutic pneumoperitoneum, appendostomy and vagotomy. Surgical interventions that have withstood the test of time include: ileostomy and subtotal or total colectomy. Medical interventions also ranged from the benign to the whimsical. These included feeding raw porcine small bowel to patients , and using ionization therapy. The latter entailed irrigating the bowel with a zinc solution and then running an electric current through the solution.
Stanford Scientists Link Ulcerative Colitis To Missing Gut Microbes
Bacteria normally inhabiting healthy peoples intestines and the anti-inflammatory metabolites these bacteria produce are depleted in ulcerative colitis patients, a Stanford study shows.
Aida Habtezion is the senior author of a study that describes how people with ulcerative colitis have insufficient amounts of a metabolite produced by a family of gut-dwelling bacteria.Steve Castillo
About 1 million people in the United States have ulcerative colitis, a serious disease of the colon that has no cure and whose cause is obscure. Now, a study by Stanford University School of Medicine investigators has tied the condition to a missing microbe.
The microbe makes metabolites that help keep the gut healthy.
This study helps us to better understand the disease, said Aida Habtezion, MD, associate professor of gastroenterology and hepatology. We hope it also leads to our being able to treat it with a naturally produced metabolite thats already present in high amounts in a healthy gut.
When the researchers compared two groups of patients one group with ulcerative colitis, the other group with a rare noninflammatory condition who had undergone an identical corrective surgical procedure, they discovered that a particular family of bacteria was depleted in patients with ulcerative colitis. These patients also were deficient in a set of anti-inflammatory substances that the bacteria make, the scientists report.
You May Like: Food For Ulcerative Colitis Flare Ups
Why Online Claims Of A Cure Are False
Ulcerative colitis and Crohns disease are chronic diseases. Either of these can go into remission for long periods but remission is not a cure. Theres always the chance of a relapse.
Theres no shortage of online or word-of-mouth claims of a cure for IBD. They usually involve sales of expensive:
- dietary supplements
- herbal products
- probiotics
While some of these things may improve symptoms, they are not a cure. And even natural products can interfere with medications or increase symptoms of IBD. Consult with a doctor before making drastic changes to your diet or taking new supplements of any kind.
You can learn more about complementary therapies from the National Center for Complementary and Alternative Medicine.
Maintaining a healthy diet can help manage symptoms. But theres no specific diet known to cure IBD. Its important to continue with regular medical check-ups even when youre in remission.
Why Choose Mount Sinai
Mount Sinai has a unique and rich tradition of specialized and individualized treatment and scientific research and discovery in ulcerative colitis. The physicians/scientists in the Mount Sinai Health System are constantly conducting clinical trials and are developing new drug therapies to help patients manage their disease. Learn more about ulcerative colitis.
There are 3 basic tests for colon cancer a stool test , sigmoidoscopy , and colonoscopy . All 3 are effective in catching cancers in the early stages, when treatment is most beneficial.
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
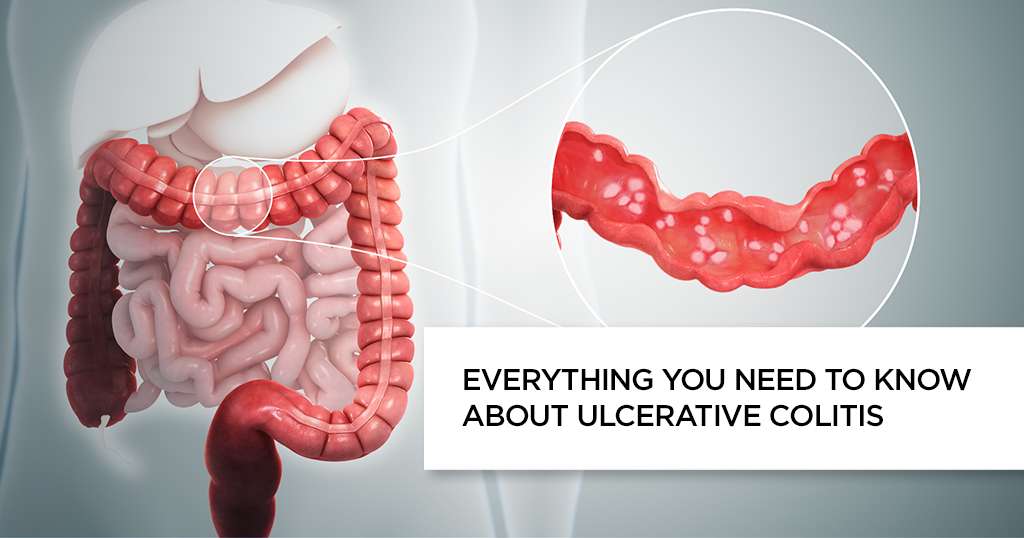
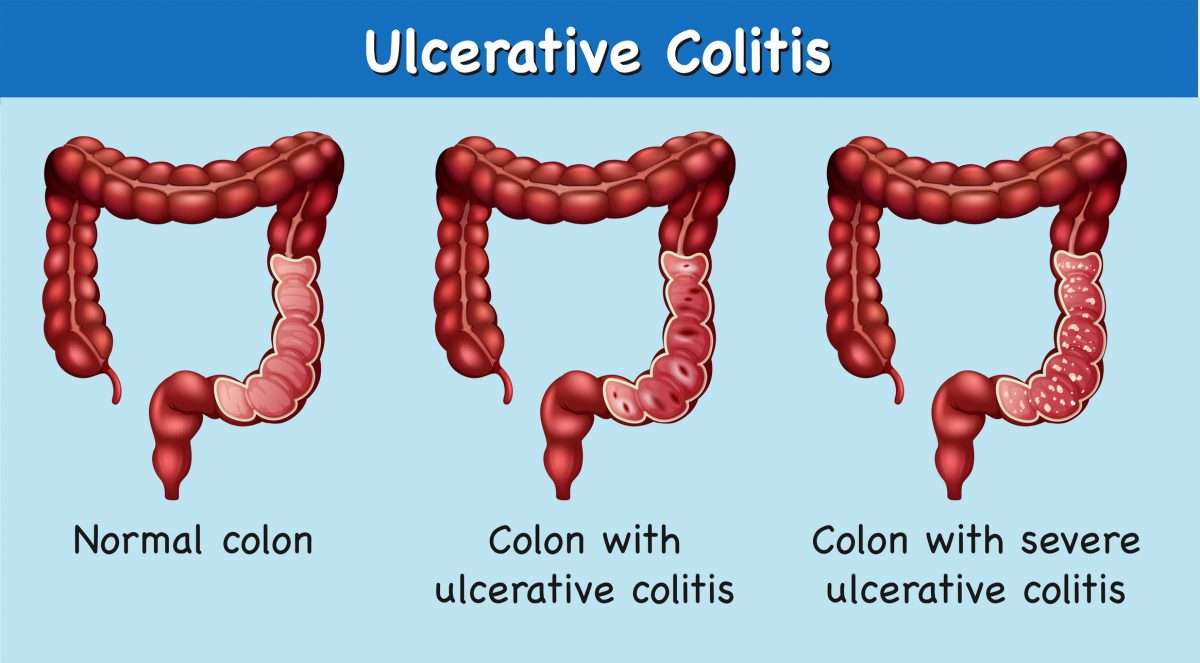
Ulcerative colitis is categorized according to location. Proctitis involves only the rectum. Proctosigmoiditis affects the rectum and sigmoid colon. Left-sided colitis encompasses the entire left side of the large intestine. Pancolitis inflames the entire colon.
Recommended Reading: What Foods Are Good To Eat With Ulcerative Colitis
Complications Of Ulcerative Colitis
UC increases your risk of developing colon cancer. The longer you have the disease, the higher your risk of this cancer.
Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when you receive your diagnosis.
Repeat screenings are recommended thereafter, according to the American Cancer Society. Regular screenings help lower your risk of colon cancer. Follow-up screenings can detect precancerous cells early.
Other complications of UC include:
- thickening of the intestinal wall
- intestinal bleeding
What Is The Role Of The Intestine’s Bacterial Contents In Ulcerative Colitis
Some of the similarities between ulcerative colitis and infectious colitides have led many investigators to search for the unidentified microorganism triggering the chronic inflammation in the large bowel. However, until now, no single microbial agent has been associated, unequivocally, with the development of ulcerative colitis. Many arguments exist against an infectious aetiology of ulcerative colitis .5
Over the past few years, we have gained considerable evidence that it is an abnormal mucosal immune reactivity, against enteric bacteria, that is the key event leading to intestinal injury in patients with IBD. Molecular biology techniques have shown that the intestinal space of an adult may contain > 500 different bacterial species some of them exert a protective role, whereas others are aggressive. The number of bacterial strains along the small bowel progressively increases, with the predominance of Gramnegative aerobes. The bacterial population in the large bowel reaches a density of around 1012 microbes per gram of luminal contents. More than 50% of the bacterial strains cannot be cultured under conditions currently available. In adults, the faecal bacterial composition is host specific and stable over time, with small fluctuations of the strains up to 20% .6
You May Like: How To Tell Stomach Ulcer
Key Growth Factor Protects Gut From Inflammatory Bowel Disease
Image demonstrating TNF-driven intestinal inflammation, where the gut-lining epithelial cells exhibit substantial cell death . Image courtesy of Dr. Lei Zhou.
A growth factor protein produced by rare immune cells in the intestine can protect against the effects of inflammatory bowel disease , according to a new discovery from Weill Cornell Medicine researchers.
In their study, published Jan. 31 in Nature Immunology, the researchers found that the growth factor, HB-EGF, is produced in response to gut inflammation by a set of immune-regulating cells called ILC3s. These immune cells reside in many organs including the intestines, though their numbers are known to be depleted in the inflamed intestines of IBD patients.
The researchers showed in experiments in mice that this growth factor can powerfully counter the harmful effects of a key driver of intestinal inflammation called TNF. In doing so, ILC3s protect gut-lining cells when they would otherwise die and cause a breach in the intestinal barrier.
Dr. Gregory Sonnenberg
Dr. Sonnenberg and his laboratory have found in recent studies that ILC3s play a key role in protecting the gut from harmful inflammationand are depleted in human patients who have IBD or colon cancer. In the new study, the team sought a more precise understanding of how ILC3s fight against IBDs inflammatory effects.
Dr. Lei Zhou
The History Of Inflammatory Bowel Disease
1 December 20211 December 2021
On 8th June 1956, he experienced yet again severe abdominal pain. As his symptoms intensified and his blood pressure decreased, the morning cabinet meeting was canceled, and the 34th US president transmitted to the hospital for surgery. Dwight D. Eisenhower was experiencing the effects from his Crohns disease, a form of inflammatory bowel disease .
In IBD, the immune system is dysregulated. It attacks the inner tissue of the stomach, colon, and other digestive organs, damaging these body parts and impairing their functionality. Strong stomach pain, diarrhea, ulcers and in some cases colon cancer are among the consequences that follow.
Just like this illness impacted Eisenhowers personal and professional life, IBD limits the everyday life of 6.5 million people, worldwide. Most of them suffer from Crohns disease or ulcerative colitis, the two main types of IBD. While they affect different body parts Crohns disease can occur anywhere from mouth to anus, ulcerative colitis is restricted to the colon they both cause recurring inflammation of the affected organs.
When IBD flares up, it can be difficult or even impossible to go about a normal day. During such relapses, the symptoms often tie IBD patients to their homes, calling in sick for work and cancelling dinner parties. Although their symptoms will subside in remission, they may still struggle with exhaustion and anxiety.
Recommended Reading: Low Dose Naltrexone Ulcerative Colitis
Genetic Background Of Ulcerative Colitis
Increasing evidence suggests the importance of genetic susceptibility in the aetiology of IBD .
Both ulcerative colitis and Crohn’s disease have a complex genetic basis, with multiple associated genes and great heterogeneity, but the genetic influence is much better recognised currently in Crohn’s disease than in ulcerative colitis. Moreover, the disease phenotype is further modified considerably by gene interaction and by the influence of several external factors.
In the past decade, more than 10 genomewide screening and various linkage studies have delineated at least nine IBD susceptibility loci . Many independent studies have shown that the NOD2/CARD15 polymorphism is not linked to ulcerative colitis, whereas Crohn’s disease susceptibility is increased in European and American Caucasian carriers of the NOD2/CARD15 polymorphism.26
What About Network Meta
Principles of network meta-analysis.9
After the quality of the evidence is assessed, recommendations are developed and graded to differentiate those based on strong evidence from those based on weak evidence.5 This information is intended to provide the user with an estimate of the groups confidence that following the recommendation will produce the desired health outcome.7 As with levels of evidence, many classification schemes have been developed for grading recommendations. The GRADE approach is commonly used to grade the strength of recommendations and has been adopted as the standard by many guideline developers and organizations, including the AGA and the ACG.4,11,12 The GRADE approach typically scores the strength of recommendations as either strong or weak, also known as conditional or discretionary.2,6 While the GRADE approach acknowledges that expertise is required to interpret any form of evidence, it considers that opinion is an interpretation ofrather than a form ofevidence.6
Once recommendations are developed and graded, the guidelines are then made available for public policy evaluation. This step is critical, Dr Feagan pointed out, because there is no point in having guidelines if they cant be implemented. Lastly, the guidelines are submitted for peer review and published.
You May Like: Natural Remedies For Leg Ulcers
What Are The Symptoms Of Ulcerative Colitis With Constipation
Thereâs no agreed-upon definition for UC with constipation. But a group of experts came up with a set of guidelines to better pinpoint it. In general, youâll need to have at least two of the following symptoms for at least 3 days a month during the prior 3 months:
- Bloating
- A sensation that you canât get all your stool out
Constipation may also cause:
- A sick feeling in your stomach
- Fatigue
The above symptoms can lead to other health issues, especially if you strain really hard when you poop. You may get:
- Tears or sores in the lining of your anus
- Swollen blood vessels around your anus
- Hard stool that gets stuck in your rectum
Providing Education Support & Advocacy To The Ibd Community
Suzanne also helped develop the advocacy vision for the Foundation. She formed the government advocacy committee to help increase the National Institutes of Health and National Institute for Diabetes, Digestive, and Kidney Diseases inflammatory bowel disease research portfolio. She also co-founded the Digestive Disease National Coalition with Irwin, and was recognized for her advocacy work on behalf of patients by Congress following her passing in 2013. The Foundations advocacy efforts have grown significantly over the years, including:
- Working with federal legislators, establishing the first-ever Congressional Crohns & Colitis Caucus with more than 68 Members of Congress who work to advance policies that help patients
- Receiving designation by the U.S. Senate for Crohns & Colitis Awareness Week
- Organizing the participation of more than 100 IBD advocates at our annual Day on the Hill
The Rosenthal and Modell families also cared greatly about ensuring that patients and caregivers have access to educational and support resources to help them through their disease journeys. Over the past five decades, the Foundations education and support programs have grown tremendously:
- About Us
Also Check: What Does Asacol Do For Ulcerative Colitis
How Are Ulcerative Colitis And Crohn’s Disease Similar
- Both diseases often develop in teenagers and young adults although the disease can occur at any age
- Ulcerative colitis and Crohn’s disease affect men and women equally
- The symptoms of ulcerative colitis and Crohn’s disease are very similar
-
The causes of both UC and Crohn’s disease are not known and both diseases have similar types of contributing factors such as environmental, genetic and an inappropriate response by the body’s immune system
Mental And Emotional Health
Stress doesnt cause IBD. But living with IBD can be stressful, and that can affect you physically. You may be able to reduce the effects of stress by:
suggests that psychological interventions may be helpful for some people with IBD. These may include:
- behavioral or self-management therapy
- mindfulness-based therapies
More research is needed to assess the effectiveness of these therapies as they relate to IBD. But if youre feeling stressed out or overwhelmed, you might want to consider seeking help from a qualified therapist. It may also be helpful to join a support group for people with IBD.
Also Check: What Is A Duodenal Ulcer And How Is It Caused
Lifestyle Changes And Behavioral Treatments To Ease Constipation
There arenât specific guidelines to manage UC with constipation. But you can take steps to boost your bowel movements, including:
Change your diet. Your doctor might urge you to eat more fruits, vegetables, and whole grains. But keep track of how you feel after you eat plant-based foods. Too much fiber can make your poop bulky. That can be a good thing. But it might worsen constipation in some people with UC.
Always check with your doctor before you make any big changes to your diet. But some things that may help UC with constipation include:
- Adding soluble fiber
- Reducing your dietary fiber until symptoms get better
- Trying a low-FODMAP diet
- Avoiding dairy foods
Stay hydrated. Extra fluid can soften your stool so itâs easier to pass. Youâve probably heard that you should aim for 8 cups of water a day. But there isnât a perfect number that works for everyone. Drink when you feel thirsty. And pay attention to the color of your urine. It should be clear or light yellow.
Get moving. Regular physical activity can urge your stool to move along. Talk to your doctor about activities that are safe during or after a flare. Some examples of UC-friendly exercises might include:
- Fast walking
- Elliptical
- Rowing
Try biofeedback. This is a kind of therapy to retrain the muscles that help you poop. A pelvic floor therapist or physical therapist can let you know if this kind of treatment might be right for you.
You might want to ask your doctor or therapist about the following: