What Is Ulcerative Colitis Know The Related Icd
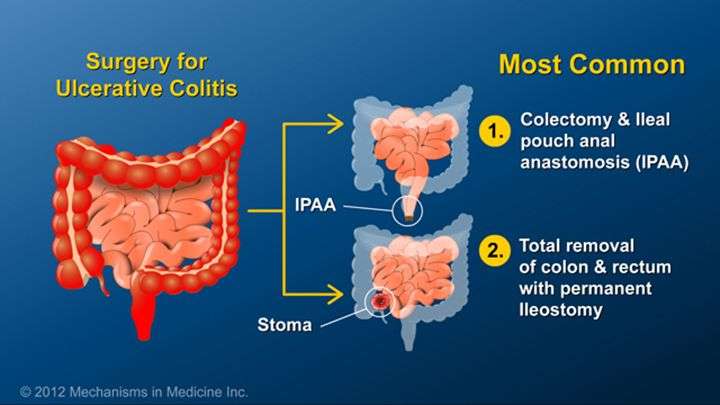
Ulcerative colitis refers to a chronic condition of the large intestine, which causes inflammation and ulcers in the lining of the large intestine or colon and rectum. This inflammatory bowel disease affects the gastrointestinal tract. Anyone with symptoms of ulcerative colitis should see a medical professional for an evaluation. Gastroenterologists and other specialists treating the condition can consider medical coding outsourcing to submit error-free claims with accurate diagnosis and procedure codes to get on-time reimbursement.
The most common symptoms of this condition are abdominal pain and bloody diarrhea with mucus. Other symptoms include loss of appetite, tiredness, weight loss, anemia, elevated temperature, dehydration or a constant urge to pass stools.
Similar to Crohns disease, this disease affects people of all ages, mostly between the ages of 15 and 35. While inflammation causes the bowel to move its contents rapidly and empty frequently, in severe cases ulcers may cause bleeding and discharge of mucus and pus. Long-term inflammation in the large intestine could even lead to colonic dysplasia or colorectal cancer. Factors that increase the risk of getting ulcerative colitis include age, ethnicity or family history. Food and stress can also trigger related symptoms.
Types and Specific Symptoms
Diagnosis
ICD-10 Codes to Report Ulcerative Colitis
Screening Colonoscopy For Non
When reporting a screening colonoscopy on a non-Medicare patient, report CPT® code 45378 and use the appropriate screening diagnosis code. As a result of the ACA, Patients covered by a group insurance policy that was purchased or renewed after September 2010 will have no co-pay or deductible, unless the plan applied for grandfathered status.
Clinical scenario three:
A 52-year-old patient calls the surgeons office and requests a screening colonoscopy. The patient has never had a screening colonoscopy. The patient has no history of polyps and none of the patients siblings, parents or children has a history of polyps or colon cancer. The patient is eligible for a screening colonoscopy. Reportable procedure and diagnoses include:
- 45378, Colonoscopy, flexible, proximal to splenic flexure diagnostic, with or without collection of specimen by brushing or washing, with or without colon decompression
- Z12.11, Encounter for screening for malignant neoplasm of colon
Diagnosis Code Ordering Is Important For A Screening Procedure Turned Diagnostic
When the intent of a visit is screening, and findings result in a diagnostic or therapeutic service, the ordering of the diagnosis codes can affect how payers process the claim. There is considerable variation in how payers process claims, and the order of the diagnosis code may affect whether the patient has outof-pocket expense for the procedure. The appropriate screening diagnosis code should be placed in the first position of the claim form and the finding or condition diagnosis in the second position. It is important to verify a payers reporting preference to avoid payment denials.
There are two sets of procedure codes that describe colonoscopy services. Additionally, there are different preventive service modifiers for Medicare and other third-party payers. The order of diagnosis coding can affect how a payer processes the claim and whether there is an out-of-pocket expense for the patient. Mastering the coding for each payer may result in lower claims processing costs, quicker payments, and fewer patient complaints.
Clinical scenario five:
At a routine screening, a patient is found to have an adenomatous polyp. The surgeon recommends that the patient return for a surveillance colonoscopy in three years. (The USPSTF recommendations do not address frequency of this repeat surveillance. The American Cancer Society does have recommendations.
Don’t Miss: What Causes Ulcers On The Feet
Differentiating Crohns From Colitis
Ulcerative colitis is another form of inflammatory bowel disease, but it bears distinct differences to Crohns. It is also a chronic disease, but inflammation only occurs in the innermost lining, or mucosal surface, of the large intestine. Symptoms can be similar to Crohns, but may include tenesmus .To properly code ulcerative colitis, the physician must document the location and severity of the inflammation:Location of the affected area:
- Pancolitis
- Proctosigmoiditis .
Severity:
- Other
- Unspecified complications
ICD-10-CM instructs us to Use additional code to identify manifestations such as: pyoderma gangrenosum with codes from category K51 Ulcerative colitis.
What Is Bowel Obstruction Caused By
Bowel obstruction usually occurs when the lumen of the intestine is either obstructed by fecal matter or other debris/foreign bodies, or is compressed by external forces such as tumors or adhesions. These are called a mechanical cause of the obstruction. When there is a condition in which the bowel does not work correctly, but there is no structural problem causing it, it is called ileus. We are going to talk about mechanical bowel obstruction in this coding tip.
Recommended Reading: Ulcerative Colitis Flare Up Length
Screening Colonoscopy For Medicare Patients
Report a screening colonoscopy for a Medicare patient using G0105 and G0121 .
Medicare beneficiaries without high risk factors are eligible for screening colonoscopy every ten years. Beneficiaries at high risk for developing colorectal cancer are eligible once every 24 months. Medicare considers an individual at high risk for developing colorectal cancer as one who has one or more of the following:
- A close relative who has had colorectal cancer or an adenomatous polyp.
- A family history of familial adenomatous polyposis.
- A family history of hereditary nonpolyposis colorectal cancer.
- A personal history of adenomatous polyps.
- A personal history of colorectal cancer.
- Inflammatory bowel disease, including Crohns Disease, and ulcerative colitis.
To report screening colonoscopy on a patient not considered high risk for colorectal cancer, use HCPCS code G0121 and diagnosis code Z12.11 . To report screening on a Medicare beneficiary at high risk for colorectal cancer, use HCPCS G0105 and the appropriate diagnosis code that necessitates the more frequent screening.
Clinical scenario two:
A Medicare patient with a history of Crohns disease presents for a screening colonoscopy. Her most recent screening colonoscopy was 25 months ago. No abnormalities are found. Reportable procedures and diagnoses include:
|
Common ICD-10 diagnosis codes indicating high risk |
|
Z85.038 |
| with band ligation |
Appendix A: Examples Of Conventional Therapy Options For Cd
Mild to moderate disease induction of remission:
Mild to moderate disease maintenance of remission:
Moderate to severe disease induction of remission:
Moderate to severe disease maintenance of remission:
Perianal and fistulizing disease induction of remission:
Metronidazole ± ciprofloxacin, tacrolimus
Perianal and fistulizing disease maintenance of remission
Don’t Miss: Ulcer In My Stomach Symptoms
American Hospital Association Disclaimer
The American Hospital Association has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
Ama Disclaimer Of Warranties And Liabilities
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Don’t Miss: What To Do When Ulcerative Colitis Flares
What Is The Difference Between A Screening Test And A Diagnostic Colonoscopy
A screening test is a test provided to a patient in the absence of signs or symptoms based on the patients age, gender, medical history and family history according to medical guidelines. It is defined by the population on which the test is performed, not the results or findings of the test. A diagnostic test is done in response to a sign or symptom, to investigate and diagnosis a condition. A patient with rectal bleeding and anemia who is has a colonscopy is having a diagnostic colonoscopy.
As such, screening describes a colonoscopy that is routinely performed on an asymptomatic person for the purpose of testing for the presence of colorectal cancer or colorectal polyps. Whether a polyp or cancer is ultimately found does not change the screening intent of that procedure.
Read more about diagnosis coding for screening colonoscopy
As part of the Affordable Care Act , Medicare and third-party payers are required to cover services given an A or B rating by the U.S. Preventive Services Task Force without a co-pay or deductible. That is, the patient has no patient due amount. However, diagnostic colonoscopy is a test performed as a result of an abnormal finding, sign or symptom. Medicare does not waive the co-pay and deductible when the intent of the visit is to perform a diagnostic colonoscopy. Medicare waives the deductible but not the co-pay when a procedure scheduled as a screening is converted to a diagnostic or therapeutic procedure.
Ulcerative Proctitis Without Complications
- 2016201720182019202020212022Billable/Specific Code
- K51.20 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM K51.20 became effective on October 1, 2021.
- This is the American ICD-10-CM version of K51.20 – other international versions of ICD-10 K51.20 may differ.
- Applicable To annotations, or
Also Check: Is Kimchi Good For Ulcerative Colitis
Fucosyltransferase 2 Gene Variant Testing
The authors stated that this meta-analysis had several drawbacks. First, these researchers included relevant articles published only in English and Chinese, so language bias may exist in this study. Second, most of the studies were conducted in Chinese populations, and there were few studies in the white subgroup analyses, which could have led to insufficient statistic power to detect weak relationships. Third, the onset of IBD is affected by risk factors such as age, sex, genetic variants, and exposure to environmental factors and their interactions. However, only gene polymorphisms were considered in this study. The effects of gene-gene and gene-environment interactions on the initiation and development of the disease need to be further studied.
The Prognosis Is Good
Some 40 years later, my sister leads a full life with Crohns. She isnt in perfect health, but shes learned to manage her disease and a house full of boys.
Resources
Prajapati, D.N., Kim, J.P., Spinelli, K.S., Sudakoff, G., Stewart, E.T., Komorowski, R.A., Telford, G.L. and Binion, D.G. , Case report: Popcorn dystrophic ileal calcification in a patient with Crohns disease. Inflammatory Bowel Disease, 9: 2527. doi: 10.1097/00054725-200301000-00004www.CrohnsAndColitis.com
Also Check: Boots To Prevent Pressure Ulcers
Diseases Of The Digestive Systemtype 2 Excludes
- 2016201720182019202020212022Non-Billable/Non-Specific Code
Type 1 Excludes
- Hemolytic anemia associated with ulcerative colitis
- Hemolytic anemia, with ulcerative colitis
- Mild chronic ulcerative colitis
- 385 Inflammatory bowel disease with mcc
- 386 Inflammatory bowel disease with cc
- 387 Inflammatory bowel disease without cc/mcc
- : New code
- 2017
Nod2/card15 Genotyping For Crohn’s Disease
Nucleotide-binding oligomerization domain proteins are cytosolic proteins that include principal regulators of apoptosis such as the apoptotic protease activating factor 1. NOD proteins have also been described as intra-cellular activators of the caspase and nuclear factor-kappaB signaling pathways. In particular, NOD1, NOD2, cryopyrin, and ICE protease-activating factor have been implicated in protective immune responses against pathogens. Moreover, a large number of NOD proteins contain leucine-rich repeats , hence referred to as NOD-LRR proteins, which include human NOD2, cryopyrin, and MHC class II trans-activator , as well as mouse neuronal apoptosis inhibitory protein 5. NOD2 participates in the signaling events triggered by host recognition of specific motifs in bacterial peptidoglycan and, upon activation, induces the production of pro-inflammatory mediators. Neuronal apoptosis inhibitory protein 5 is needed in macrophages to restrict intra-cellular growth of Legionella pneumophila, whereas CIITA plays a critical role in antigen presentation and development of antigen-specific T lymphocytes. Thus, NOD-LRR proteins appear to be involved in a diverse array of processes needed for host immune reactions against pathogens .
Recommended Reading: Carbohydrate Diet For Ulcerative Colitis
How To Report Screening Colonoscopy That Becomes Therapeutic
How do I report a screening colonoscopy that became therapeutic?
It is not uncommon to remove one or more polyps at the time of a screening colonoscopy. Because the procedure was initiated as a screening, the screening diagnosis is primary and the polyp is secondary. The endoscopist reports the appropriate code for the diagnostic or therapeutic procedure performed, e.g. CPT code 4537945392.
What modifiers do I use to indicate that a screening procedure became therapeutic?
CMS developed the PT modifier to indicate that a colonoscopy that was scheduled as a screening was converted to a diagnostic or therapeutic procedure. The PT modifier is appended to the CPT code.
CPT developed modifier 33 for preventive services, when the primary purpose of the service is the delivery of an evidence-based service in accordance with a U.S. Preventive Services Task Force A or B rating in effect and other preventive services identified in preventive services mandates , the service may be identified by adding 33 to the procedure.
For example, if a physician performing a screening colonoscopy finds and removes a polyp with a snare, use CPT code 45385 and append modifier 33 to the CPT code.
Is diagnosis code ordering important for a screening procedure turned diagnostic?
What happens if, during the course of a screening colonoscopy a polyp or lesion is found and the physician performs a biopsy or polypectomy?
License For Use Of Current Dental Terminology
End User License Agreement:These materials contain Current Dental Terminology , copyright © 2021 American Dental Association . All rights reserved. CDT is a trademark of the ADA.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. By clicking below on the button labeled “I accept”, you hereby acknowledge that you have read, understood and agreed to all terms and conditions set forth in this agreement.
If you do not agree with all terms and conditions set forth herein, click below on the button labeled “I do not accept” and exit from this computer screen.
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
Read Also: Can Ulcers In The Colon Be Cancerous
Clear And Concise Documentation Aids Diagnosis Coding
I first heard the term Crohns disease when I was 12 years old. The surgeon who had just finished operating on my older sister was talking to my grandparents. She didnt have acute appendicitis, after all, he said. A section of her small intestine had calcified from chronic inflammation.That was the first of many hospitalizations and surgeries my sister endured to regain her health. Probably the hardest part for her was finding out she had an incurable disease she would have to cope with the rest of her life, and she was only 16.
Pharmacogenomic And Metabolic Assessment Of Thiopurine Therapy
The PRO-Predict series of tests were developed by Prometheus, Inc. with the intent of providing guidance in determining therapeutic direction and predicting therapeutic response in individual patients. PRO-Predict 6MP is for 6-MP/Azathioprine remission and toxicity monitoring, PRO-Predict TPMT is for 6-MP/azathioprine response stratification, and PRO-Predict TNF is for anti-TNF response stratification. However, there is insufficient scientific evidence in the current medical literature to support the routine use of these tests in clinical practice.
Although there is a potential to regulate azathioprine and mercaptopurine according to measurement of metabolites, the optimal mode of therapeutic monitoring remains to be established through prospective clinical trials demonstrating that clinical outcomes are improved through metabolite monitoring. Current evidence is largely limited to studies exploring correlations between metabolite levels and azathioprine and mercaptopurine toxicity and response. These studies have shown conflicting results in the strength of the relationship between metabolite levels, toxicity, and response. There are no well-designed prospective clinical studies demonstrating that azathioprine or mercaptopurine therapy based upon results of metabolite testing leads to improved clinical outcomes compared to therapy based upon clinical assessment and standard testing including routine blood counts and liver enzymes.
Read Also: How To Repair An Ulcer
Gastroenterology Billing And Coding: Just The Basics
3. Diagnostic studies: Medical necessity/indication for the testing must be documented in order to submit charges for diagnostic studies. The terms rule out and suspect dont completely give coders the reason why a physician suspects the patient might have a condition. Usually, abnormal lab tests, signs, and symptoms will often warrant the need for further investigation, and these are the most crucial indications for testing. Not only is this important for diagnostic studies but also for procedures. Make sure that the interpretation of the test results is clear along with a plan/recommendation.
- K50.10 Crohns disease of large intestine without complications.
- K50.111 Crohns disease of large intestine with rectal bleeding.
- K50.112 Crohns disease of large intestine with intestinal obstruction.
- K50.113 Crohns disease of large intestine with fistula.
- K50.114 Crohns disease of large intestine with abscess.
- K50.118 Crohns disease of large intestine with other complication.
- K50.119 Crohns disease of large intestine with unspecified complications.