What You Need To Know About Ulcerative Colitis And Colorectal Cancer
Posted by Minnesota Oncology Physicians on October 4, 2021
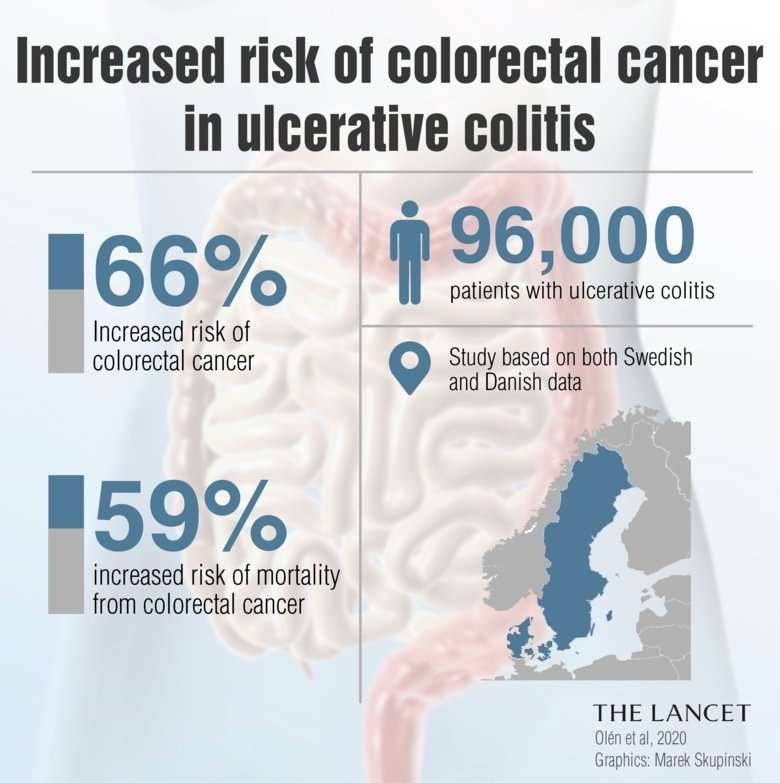
There is a significant link between ulcerative colitis and colorectal cancer. If you have UC, your risk of developing colorectal cancer is six times greater. And the longer you have had ulcerative colitis, the higher your risk for colon or rectal cancer becomes. Why are these two conditions of the intestines connected?
Are There Pancolitis Complications To Be Aware Of
The most alarming short-term complication of pancolitis is a rare condition called toxic megacolon.5 Thats when your colon becomes dilated due to inflammation and eventually perforates , which can be fatal, Dr. Schwimmer says. When toxic megacolon is discovered, he says, it means the person needs surgery immediately.
One bright spot, Dr. Schwimmer says, is that toxic megacolon happens less these days because people are more aware of ulcerative colitis symptoms, and modern medications work much better to control inflammation.
A longer-term consequence of pancolitis is an increased risk of colon cancer. Still, the risk is pretty lowabout 2% for someone who has had ulcerative colitis symptoms for at least 10 years, according to an older study published in the World Journal of Gastroenterology.6 The more colon tissue you have that is inflamed, the higher your cancer risk becomes. Since pancolitis affects the whole colon, it means more opportunity for inflammation. Thats why its extremely important for people with IBD to be screened for colon cancer according to their doctors recommendation.
How Is Ulcerative Colitis Diagnosed
The usual test is for a doctor to look inside the colon and the rectum by passing a special telescope up through the back passage into the rectum and colon. These are a short sigmoidoscope or a longer flexible colonoscope. See the separate leaflets called Sigmoidoscopy and Colonoscopy for more details.
The appearance of the inside lining of the rectum and colon may suggest ulcerative colitis. Small samples are taken from the lining of the rectum and colon and looked at under the microscope. The typical pattern of the cells seen with the microscope may confirm the diagnosis. Also, various blood tests are usually done to check for anaemia and to assess your general well-being.
Special X-ray tests such as a barium enema are not often done these days, as the above tests are usual to confirm the diagnosis and assess the disease severity.
A stool sample is commonly done during each flare-up and sent to the laboratory to test for bacteria and other infecting germs. Although no germ has been proven initially to cause ulcerative colitis, infection with various known germs can trigger a flare-up of symptoms. If a germ is found, then treatment of this may be needed in addition to any other treatment for a flare-up .
Recommended Reading: How Do They Treat Ulcerative Colitis
Inflammation And Tumorigenesis In Ibd
The innate and adaptive immune system cells play an important role in the onset of IBD-CRC. Crosstalk between these cell types occurs mainly through a network of cytokines that drive and maintain inflammation and contribute to tumorigenesis via oxidative stress, epithelial cell proliferation, and angiogenesis . In Table 1 is reported a brief summary of the effects of different inflammation-related molecules in IBD-CRC.
TABLE 1. cytokines and/or pro-inflammatory molecules in IBD-CRC.
Among these molecules, the macrophage migration inhibitory factor , a pleiotropic cytokine that drives cellular proliferation and regulates the migration and activation state of immune cells, seems to be relevant. The pathophysiological role of MIF in a wide range of inflammatory diseases, among which IBD, was already demonstrated . Increased MIF in macrophages in a CRC mouse model was demonstrated, and loss of MIF expression protects mice during tumor initiation . In cancer cells from CRC patients and in an acute colitis-CRC mouse model, a tumor-specific elevation of MIF expression was demonstrated . The heat shock protein 90 chaperone machinery stabilizes and protects MIF from degradation and supports tumor progression via macrophage recruitment and angiogenesis.
In the context of inflammation and CRC, the most investigated pathways are the nuclear factor light-chain enhancer and IL-6/signal transducer and activator of transcription 3 and STAT6 signaling pathways .
What Are The Types Of Ulcerative Colitis
Ulcerative proctitis: Inflammation limited to the area close to the anus . Symptoms are usually mild, and rectal bleeding may be the only sign.
- Proctosigmoiditis: Inflammation involves the lower end of the colon
- Left-sided colitis: Inflammation extends from the rectum up through the sigmoid and descending colon
- Pancolitis: Involves the entire colon
- Acute severe ulcerative colitis : This rare form of colitis affects the entire colon and causes severe pain, profuse diarrhea, bleeding, fever, and inability to eat.
The severity of UC can be graded as follows:
- Mild: Bleeding per rectum and fewer than four bowel motions per day
- Moderate: Bleeding per rectum with more than four bowel motions per day
- Severe: Bleeding per rectum more than four bowel motions per day and systemic illness with protein loss from the body
Also Check: Ulcer Cause Blood In Stool
How Can We Decrease The Risk Of Crc In Ibd
The positive association between UC and CRC raises several practical questions. The causes behind the changing trends in UC-related CRC epidemiology are complex. One key element may be the early diagnosis and treatment of precancerous lesions by colonoscopic surveillance or sometimes prophylactic colectomy, while the third option is primary chemoprevention. Nowadays, prophylactic colectomy is obsolete. Nonetheless, the high colectomy rate, especially in Scandinavian countries has been associated with lower CRC risks. There are however, obvious changes in the patient management, also in Scandinavia. In the new population-based cohorts, a decrease in the colectomy rate can be observed.
Extent And Duration Of Ibd
The extent of colonic inflammation is a risk factor for CRC. UC patients with extensive disease have a greater risk of developing CRC than do UC patients with only proctitis or proctosigmoiditis . IBD duration is one of the most important risk factors for CRC among IBD patients. CRC risk is significantly increased after 8 years of IBD and continues to increase in subsequent years .
Don’t Miss: Does Ulcer Pain Come And Go
How Ulcerative Colitis Affects Your Risk For Developing Colorectal Cancer
Categories:Colorectal Cancer,Gastrointestinal Cancers
Did you know theres a significant link between ulcerative colitis and colorectal cancer? Ulcerative colitis patients have a six times greater risk of developing colorectal cancer than those of average risk. But, that being said, only about 5% of people with severe ulcerative colitis will end up developing this type of cancer. Plus, there are ways you can lower your risk.
What Are The Causes Of Ulcerative Colitis
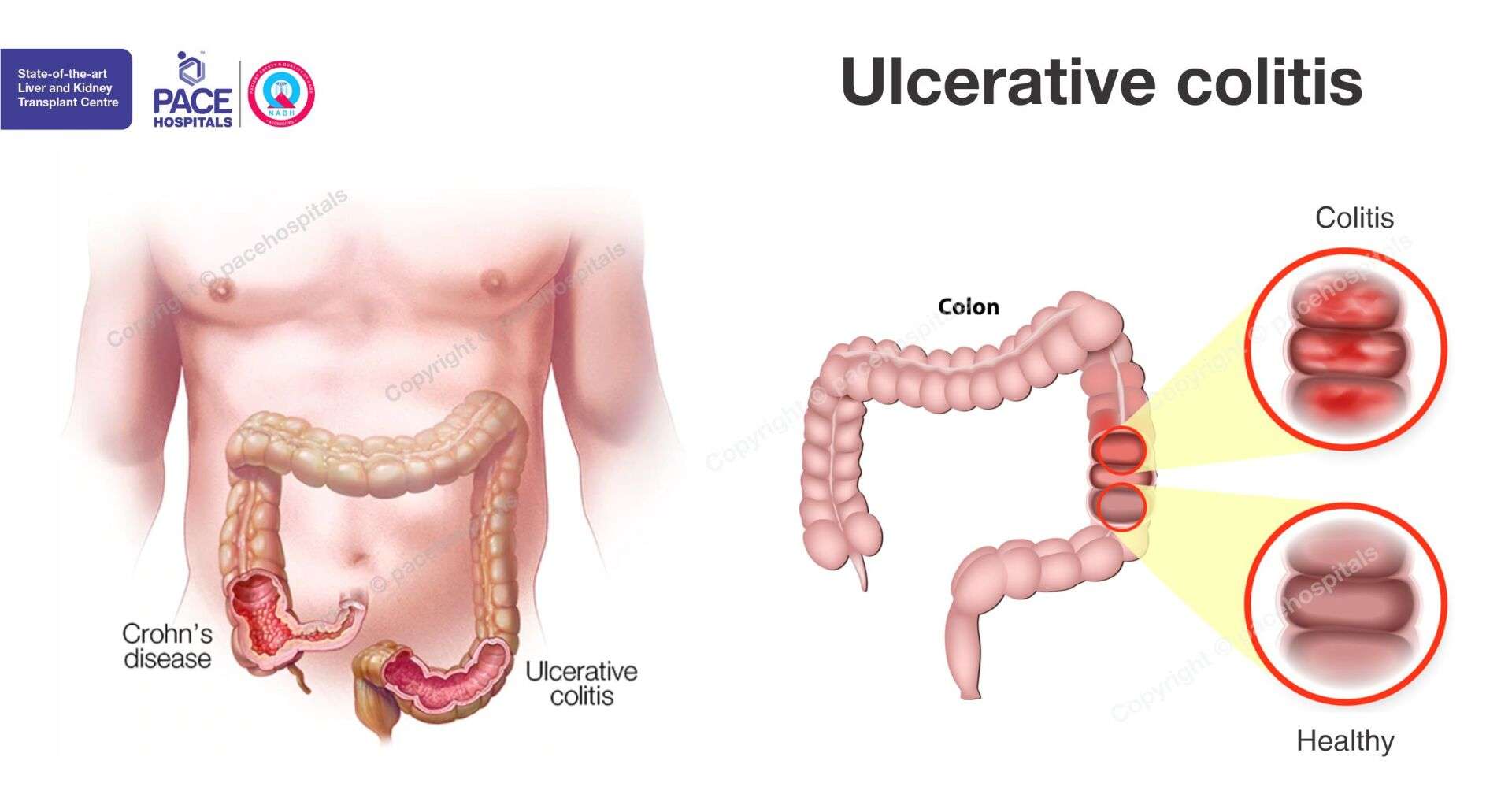
Ulcerative colitis is an inflammatory bowel disease affecting the inner lining of the large intestine leading to erosion and ulcers. It is a lifelong illness with no specific cause or cure. Patients have repeated cycles of flare-ups and remission with potential manifestations beyond the gut . There is a profound emotional and social impact on the affected patients.
What are the causes of ulcerative colitis?
The exact cause of ulcerative colitis is unknown, and the possible causes are as follows:
- Genetics
- Immune reactions
Recommended Reading: Sample Meal Plan For Ulcerative Colitis
How Often To Screen
since your symptoms first appeared or you were diagnosed with UC.
People with UC are generally advised to have a colonoscopy . Some people may need to have this test more or less often based on factors such as:
- the age when they were diagnosed
- how much inflammation they have and how much of their colon it affects
- their family history of colorectal cancer
- whether they also have PSC
Being Overweight And Obese
Obesity is a cause of bowel cancer. It is estimated that 11 out of 100 bowel cancers in the UK are linked to being overweight or obese.
Obesity means being very overweight with a body mass index of 30 or higher. And being overweight is a BMI of between 25 and 30. The risk of bowel cancer is higher in people who are obese compared to those who have a healthy BMI.
Also Check: What Can I Eat When I Have Ulcerative Colitis
Future Research In Crc And Ibd
The microbiota plays an important role in the development of CRC, in recent years oncogenic gut microbiota biomarkers have been developed for screening, so far with promising results and is expected to be a less invasive diagnostic auxiliary tool . In addition to markers through bacteria, oncogenic markers have been analyzed in blood and fecal samples such as miRNA, tumor-associated antigens, the tumor specific M2 isoform of pyruvate kinase, tissue inhibitor of matrix metalloproteinase 1, which are molecules created by oncologic processes with a sensitivity greater than 90% . New endoscopic technologies have increased in recent years, confocal laser endomicroscopy is a new technique that allows live visualization during the endoscopic study of the gastrointestinal mucosa. With this new technique, details about the microscopic architecture can be obtained in real time, being able to detect microscopic inflammation and the presence of dysplasia . Therapies for the treatment of CRC through chemotherapy can trigger exacerbations and IBD activity in these patients, so new therapies such as organometallic compounds and metal complexes are being sought for their anti-inflammatory effect in other pathologies .
What Are The Symptoms During A Flare
- Diarrhoea. This varies from mild to severe. The diarrhoea may be mixed with mucus or pus. An urgency to get to the toilet is common. A feeling of wanting to go to the toilet but with nothing to pass is also common . Water is not absorbed so well in the inflamed colon, which makes the diarrhoea watery.
- Blood mixed with diarrhoea is common .
- Crampy pains in the tummy .
- Pain when passing stools.
Feeling generally unwell is typical if the flare-up affects a large amount of the colon and the rectum , or lasts for a long time. High temperature , tiredness, feeling sick , weight loss and anaemia may develop.
Also Check: Over The Counter For Ulcers
Reducing The Risk Of Cancer
People with UC are at greater risk of developing colorectal cancer, so it is important to take steps to manage this risk.
People with UC should see their doctor at least once per year for annual checkups and scans. At these appointments, they can discuss their condition and overall state of health.
Doctors may be able to help manage the risk of colorectal cancer in people with UC.
A Personal History Of Inflammatory Bowel Disease
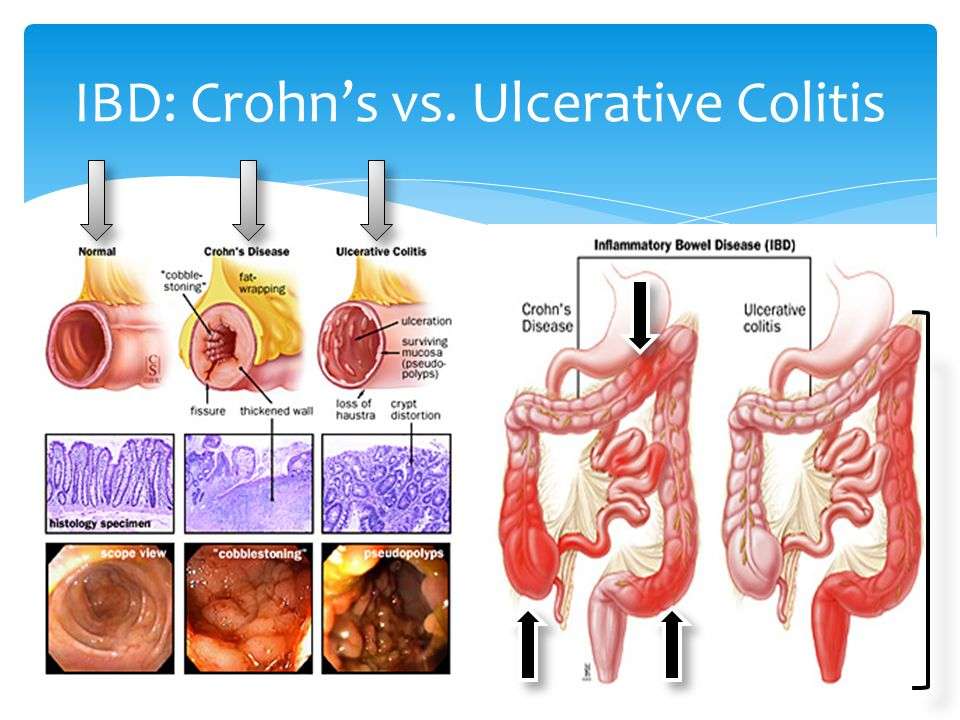
If you have inflammatory bowel disease , including either ulcerative colitis or Crohns disease, your risk of colorectal cancer is increased.
IBD is a condition in which the colon is inflamed over a long period of time. People who have had IBD for many years, especially if untreated, often develop dysplasia. Dysplasia is a term used to describe cells in the lining of the colon or rectum that look abnormal, but are not cancer cells. They can change into cancer over time.
If you have IBD, you may need to start getting screened for colorectal cancer when you are younger and be screened more often.
Inflammatory bowel disease is different from irritable bowel syndrome , which does not appear to increase your risk for colorectal cancer.
Also Check: How To Get Remission In Ulcerative Colitis
Why Regular Colorectal Cancer Screenings Are So Important
Colorectal cancer is curable, especially in the early stages. The best chance of complete remission comes with finding polyps early that need to be removed before they turn into cancer. This makes the entire process easier on you, less invasive, reduces the chance of it spreading to other organs, and is less expensive than late-stage cancer treatment.
To find colorectal cancer early, you need to stick with a regular cancer screening schedule. If you have ulcerative colitis or other medical conditions that put you at risk for colorectal cancer, your primary care doctor may recommend starting cancer screenings younger than the average age of 45. Screening for colon and rectal cancer can be done with an at-home stool test using a test such as a colonoscopy or a sigmoidoscopy. The right test for you, based on the severity of the UC, will be determined by your physician.
Signs And Symptoms To Look Out For
Knowing the signs to look out for can help. However, many signs and symptoms of colorectal cancer also happen to be signs of inflammatory bowel diseases.
For instance, blood in the stool is a sign of colorectal cancer as well as a symptom of UC. It is easy to confuse the potential signs of cancer with those of a normal UC flare-up. For this reason, it is important to regularly check in with a doctor to discuss and monitor the progression of the condition.
Anyone with UC who experiences the following changes or symptoms should speak with a doctor:
Also Check: Snack Ideas For Ulcerative Colitis
How Colitis May Affect Your Cancer Risk
Signs and symptoms of colon cancer can be tougher to discern in ulcerative colitis patients. Blood in the stool, for example, which is a warning sign of cancer, may also happen as a result of a flare-up of the condition. The cancer itself is different, too, says Dr. Chang. Cancer in UC patients looks more like lesions, and less like masses or tumors, she says. But certain factors can increase your likelihood of developing cancer, including:
- The Severity of the Condition The longer you have uncontrolled inflammation, the more likely you are to develop dysplasia. Put another way, its not just having ulcerative colitis that ups your cancer risk its having uncontrolled UC that puts you in the danger zone.
- How Much of Your Colon is Affected If just the 5 to 10 centimeters of colon closest to the rectum is affected a condition called ulcerative proctitis your risk is similar to that of the normal population. If your entire colon is affected, your risk rises.
What Are The Treatment Options For A Flare
When you first develop ulcerative colitis it is usual to take medication for a few weeks until symptoms clear. A course of medication is then usually taken each time symptoms flare up. The medicine advised may depend on the severity of the symptoms and the main site of the inflammation in the colon and the rectum .
Topical treatments applied locally by an enema or suppository are widely used for treating ulcerative colitis, particularly aminosalicylate and steroid medicines – see below. They are a treatment option if ulcerative colitis affects only the lower part of the bowel .
Medication options include the following:
You May Like: What Is A Good Diet For Ulcers
Getting Screened For Cancer
Because your risk for colorectal cancer increases over time if you have UC, its important to receive regular screenings for colorectal cancer.
People with UC should talk to their doctors about getting a colonoscopy, the main test used to detect this cancer.
Getting regular colonoscopies can help lower your risk for developing colorectal cancer or dying from colorectal cancer.
For people with IBDs who underwent regular screenings, the odds of developing colorectal cancer dropped by 42 percent. The odds of dying from the cancer dropped by 64 percent.
Does Pancolitis Affect Children
Children can develop ulcerative colitis, including pancolitis. In fact, theres reason to believe that rates of IBD in children are actually increasing, according to a 2015 study published in JAMA Pediatrics.7 Researchers hypothesize that formula feeding, high amounts of dietary fat, and exposure to antibiotics early in life may all play a role in these rising rates.
Treatments for pancolitis are the same for children as they are for adults, and revolve around controlling ulcerative colitis inflammation. Dr. Bechtold explains that in many cases, the same medications can be used, just at a lower dosage. Kids with ulcerative colitis do need to be watched carefully, though, as colon inflammation can impact how nutrients are absorbed which can impair growth, according to a 2012 study published in the World Journal of Gastroenterology.8
The good news is no matter your age, people with pancolitis can go into long-term remission with the help of a dynamic, ongoing treatment plan, says Dr. Scwhimmer. The hope is always that the medications will keep inflammation down and the risk of cancer down as well.
You May Like: What To Take For Stomach Ulcer Pain
How Is Pancolitis Connected To Ulcerative Colitis
To understand pancolitis as it relates to ulcerative colitis, we have to see where it lands on the spectrum of disease, David Schwimmer, MD, a gastroenterologist in Sarasota, Florida, tells SELF. Ulcerative colitis is a general diagnostic term for chronic, inflammatory bowel disease affecting your colon. Heres a quick breakdown of the different types, according to the Mayo Clinic:
- Ulcerative proctitis: This is the mildest form of ulcerative colitis, which Dr. Schwimmer explains is inflammation that only affects your rectum, the few inches closest to your anus. Rectal bleeding may be the only symptom you experience.
- Proctosigmoiditis: This is inflammation that affects both the rectum and the sigmoid colon, which is the lower end of the colon. This is where you may start to get those classic symptoms of ulcerative colitis, like bloody diarrhea, abdominal cramps, and an urge that you have to go now.
- Left-sided colitis: In this scenario, the inflammation affects everything from the rectum to the descending colon on the left side of your body. In addition to the previously mentioned symptoms, you may feel pain specifically on the left side of your abdomen.
- Pancolitis: This is where the inflammation impacts your entire colon lining, and in addition to having more severe symptoms, you may also have fatigue and unintentional weight loss.