What Is Being Tested
Calprotectin is a protein released by a type of white blood cell called a neutrophil. When there is inflammation in the gastrointestinal tract, neutrophils move to the area and release calprotectin, resulting in an increased level in the stool. This test measures the level of calprotectin in stool as a way to detect inflammation in the intestines.
Intestinal inflammation is associated with inflammatory bowel disease and with some bacterial GI infections, but it is not associated with many other disorders that affect bowel function and cause similar symptoms. Calprotectin can be used to help distinguish between inflammatory and non-inflammatory conditions.
IBD is a group of chronic disorders characterized by inflamed and damaged tissues in the lining of the intestinal tract. The cause of IBD is not known, but these diseases are thought to be due to an autoimmune process that has been triggered by a genetic predisposition, a viral illness, and/or an environmental factor. The most common inflammatory bowel diseases are Crohn disease and ulcerative colitis .
Why Was This Study Needed
Around 10% of presenting problems to GPs involve gastrointestinal symptoms. Most young adults who present with symptoms such as changed bowel habit and pain have a functional bowel disorder, such as irritable bowel syndrome, which does not require invasive investigation.
However, symptoms of IBD and functional bowel disorder can be similar, making it challenging to minimise the burden of unnecessary further investigation without missing the minority who do have IBD and may come to considerable harm without timely investigation.
Currently, where GPs suspect cancer or IBD, patients are referred for urgent investigation. However, there is often considerable diagnostic uncertainty between IBD and functional bowel disorders, and a test to reduce this uncertainty may avoid patients being referred for unnecessary invasive testing. Other research has previously demonstrated the usefulness of calprotectin testing to rule out IBD in patients who do not have concerning or severe symptoms this study included some patients with concerning symptoms such as bleeding, but otherwise considered at low risk of having cancer.
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohns or Colitis. All events are open to members of Crohns & Colitis UK.
You May Like: Can Stomach Ulcers Cause Diarrhea
Screening Of Pediatric Ibd Stool Using An Aptamer
An overview of the study flow is depicted in Fig. . For the initial aptamer-based screen of stool proteins, 24 stool samples were interrogated for 1129 proteins, as detailed in the methods section. Of the 1129 proteins assayed using the aptamer-based screen, significant upregulation of multiple proteins was seen in IBD stool compared to healthy controls, as shown in the volcano plot . Of the proteins that were significantly elevated in IBD vs HC, 48 stool proteins were found to be elevated in both CD and UC stool when compared to healthy control stool . Of these 48 stool proteins, only 3 survived multiple testing corrections , presumably because of the small sample size. Two proteins were elevated in the stool of CD patients but not UC when compared to healthy controls, while 18 proteins were elevated in the stool of UC patients when compared to healthy controls while not being elevated in CD stools compared to the healthy controls .
Fig. 1: An overview of the study showing the discovery of panels of stool proteins arising from an initial aptamer-based screen.Fig. 2: Aptamer-based screening of pediatric IBD stool samples for 1129 proteins.
What Are The Implications
The study supports NICE guidance that calprotectin testing could be a useful tool to support GPs to rule out IBD in many patients, even if they do have bleeding. Designers of referral pathways may consider how to integrate calprotectin testing in order to reduce referrals for invasive diagnostic investigation.
The study authors recommend that, although not definitive in themselves, calprotectin tests may be useful as part of locally-agreed referral pathways that include: good oversight, close coordination with secondary care, ongoing training, and audit.
The authors also recommend an 8-week safety net review of non-referred patients with negative test results to ensure that patients with false negative result are not lost to follow up.
Read Also: What Age Do You Get Ulcerative Colitis
Combination Of Several Stool Markers
Most studies suggest that the combination of calprotectin with additional stool markers such as neopterin, lactoferrin or S100A12 does not result in higher diagnostic accuracy. However, in the study by Schroeder and colleagues the combination of PMN elastase with calprotectin and lactoferrin was associated with a higher sensitivity, specificity, PPV and NPV compared with PMN elastase alone . There are currently not sufficient data to support the clinical use of more than one stool test at the same time. Using more than one stool test in clinical practice would lead to higher costs without a corresponding increase in diagnostic performance.
Colorectal Cancer Risk In Ibd
Colorectal cancer risk and IBD
Patients with IBD appear to be at notably increased risk of colorectal cancer compared to the general population , with one recent study demonstrating a 7% colorectal cancer risk after 30 years of disease . Patients with at least 8 years disease duration and colonic involvement are at increased risk of colorectal cancer . Patients at risk of colorectal cancer should be enrolled in a dysplasia surveillance plan as this appears to reduce the risk of colorectal cancer. Surveillance typically includes colonoscopy every 1-3 years, depending on individual patient risk .
Risk factors and surveillance intervals
In patients at high risk, consider ~1 year surveillance intervals. High risk features include: primary sclerosing cholangitis , prior history of dysplasia or colonic strictures, or strong family hx of colorectal cancer . Patients with low to moderate risk may be surveyed every 2-3 years. Moderate risk features include: extensive colitis with moderate inflammatory burden, family hx of CRC in first degree relative > age 50 and possibly extensive inflammatory polyps or pseudopolyps
Surveillance Protocols
Management of Endoscopic lesions
Any visible polyps or lesions should be endoscopically resected if feasible and the specimen should be sent in a separately labeled jar. If a lesion has indistinct borders or is not amenable to resection, biopsy sample should be taken and sent in a separate jar.
Management of Dysplasia
Also Check: Ulcerative Colitis Weakness And Fatigue
Causes Symptoms And Diagnosing Tests For Ulcerative Colitis
Ulcerative colitis is a chronic, recurring disease where the large intestine is inflamed. It is one of the most common types of inflammatory bowel disease after Crohns disease. This disease can happen to anyone, irrespective of gender and age.
Blood tests and stool samples helps diagnosis, but the important tests are the ulcerative colitis tests, which are the internal examination of the bowel and its biopsy. Treatment would involve taking medication or surgery. Recent studies suggest that ulcerative colitis can be cured, not limited to just control of the disease.
What Causes Ulcerative Colitis In A Child
Healthcare providers don’t know what causes this condition. It may be triggered by a virus or bacteria. This interacts with your childs immune system and causes an inflammatory reaction in the intestinal wall.
Children with ulcerative colitis often have problems with their immune system. It’s not clear if these issues are a cause or a result of the disease.
Theres no known cure for this condition. But there are medical treatments and surgery if needed.
You May Like: Difference Between Ulcerative Colitis And Diverticulitis
How To Reduce Your Risk
Here are a few other things you can do to lower your chances of developing colorectal cancer and improve your odds of finding it early if you develop it:
- Ask your doctor about taking medications such as sulfasalazine , vedolizumab , or mesalamine . These drugs help manage UC, and they may help lower your risk for colorectal cancer.
- Take your medications as your doctor prescribed to keep your UC inflammation well managed.
- See your gastroenterologist for check-ups at least once a year.
- Let your doctor know if any of your family members had colorectal cancer or have recently been diagnosed.
- Eat more fruits, vegetables, and whole grains such as brown rice or wheat bread.
- Limit red meat, such as burgers, steaks, and pork. Also limit processed meats, such as hot dogs, bacon, and sausage. Theyve been linked to colorectal cancer risk.
- Avoid alcohol or limit yourself to no more than one drink a day.
- Try to walk, ride a bike, or do other exercises on most days of the week.
Along with getting regular screenings, look for these symptoms of colorectal cancer and report them to your doctor right away:
- a change in your bowel movements
- blood in your stool
Posted by Minnesota Oncology Physicians on October 4, 2021
Recommended Reading: Whats The Difference Between Colitis And Ulcerative Colitis
Endoscopy Of The Large Intestine
Doctors order endoscopy of the large intestine with biopsies to diagnose ulcerative colitis and rule out other digestive conditions. Doctors also use endoscopy to find out how severe ulcerative colitis is and how much of the large intestine is affected.
During an endoscopy, doctors use an endoscopea long, flexible, narrow tube with a light and a tiny camera on one endto view the lining of the large intestine. Doctors obtain biopsies by passing an instrument through the endoscope to take small pieces of tissue from the lining of your rectum and colon. A pathologist will examine the tissue under a microscope.
Two types of endoscopy used to diagnose ulcerative colitis are
- colonoscopy, in which a doctor uses a type of endoscope called a colonoscope to view the lining of your rectum and your entire colon
- flexible sigmoidoscopy, in which a doctor uses a type of endoscope called a sigmoidoscope to view the lining of your rectum and lower colon
You May Like: Is Olive Oil Good For Ulcerative Colitis
Elisa Validation Of Stool Protein Biomarkers
In total, 33 proteins were initially selected from the aptamer-based screen for ELISA validation in a cross-sectional cohort. After initial testing for optimal sample dilution to use, 20 protein biomarkers were assayed using commercially available ELISA assays, following manufacturer instructions. Vendor, catalog number, and stool sample dilution for these ELISA kits are listed in Supplementary Table . The absolute levels of stool protein biomarkers were determined using standard curves run on each ELISA plate, and the data were normalized by stool weight. ELISA assay protocols are detailed in our previous studies.
The Fecal Calprotectin Test Is Often Used To Differentiate Between Irritable Bowel Syndrome And Inflammatory Bowel Disease
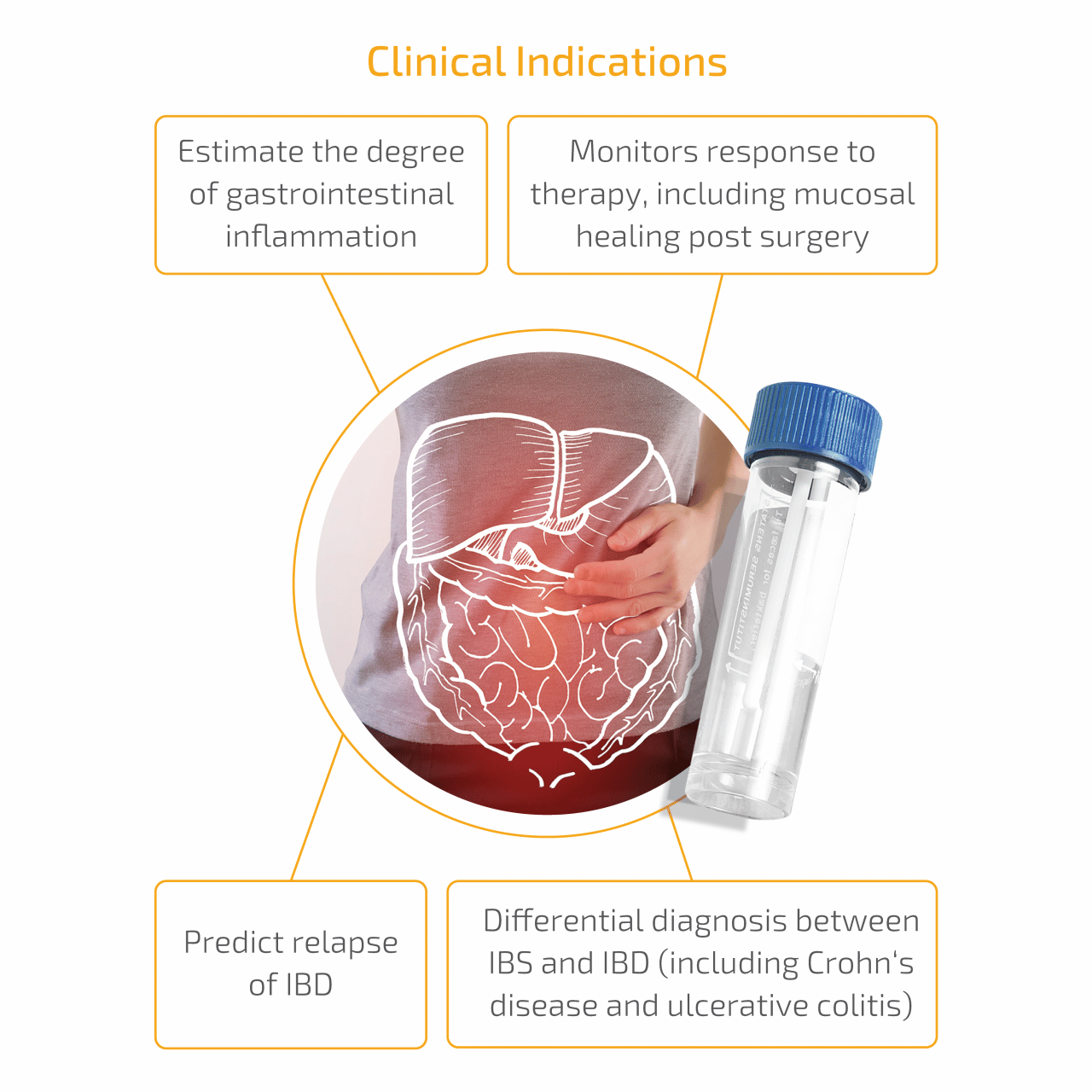
IBS and IBD are two conditions with common symptoms such as diarrhea, abdominal bloating, and cramping, but are in fact quite different and have very different treatment options.
- IBS is a disorder affecting the intestine. IBS involves problems with motility and sensitivity , leading to abdominal pain, changes in bowel patterns and other symptoms. IBS is a functional gut disorder. Functional means that the affected area are impaired and not working the way they should, however there are no visible abnormalities that can be observed through testing. IBS symptoms are commonly controlled through diet, and lifestyle changes and in more severe cases, medication.
- IBD is at least two separate disorders that cause inflammation and ulceration of the small and large intestines. These two disorders are called ulcerative colitis and Crohns disease and symptoms can range from mild to debilitating, and even life-threatening. Since the disease is not curable, long-term treatment is often required.
Not only is the fecal calprotectin used to distinguish between IBD and non-inflammatory disorders such as IBS, but if you have already been diagnosed with IBD, it can be used to monitor your IBD. This includes:
- Assessing response to treatment,
- and even predicting flares!
You May Like: Ulcer Points On A Horse
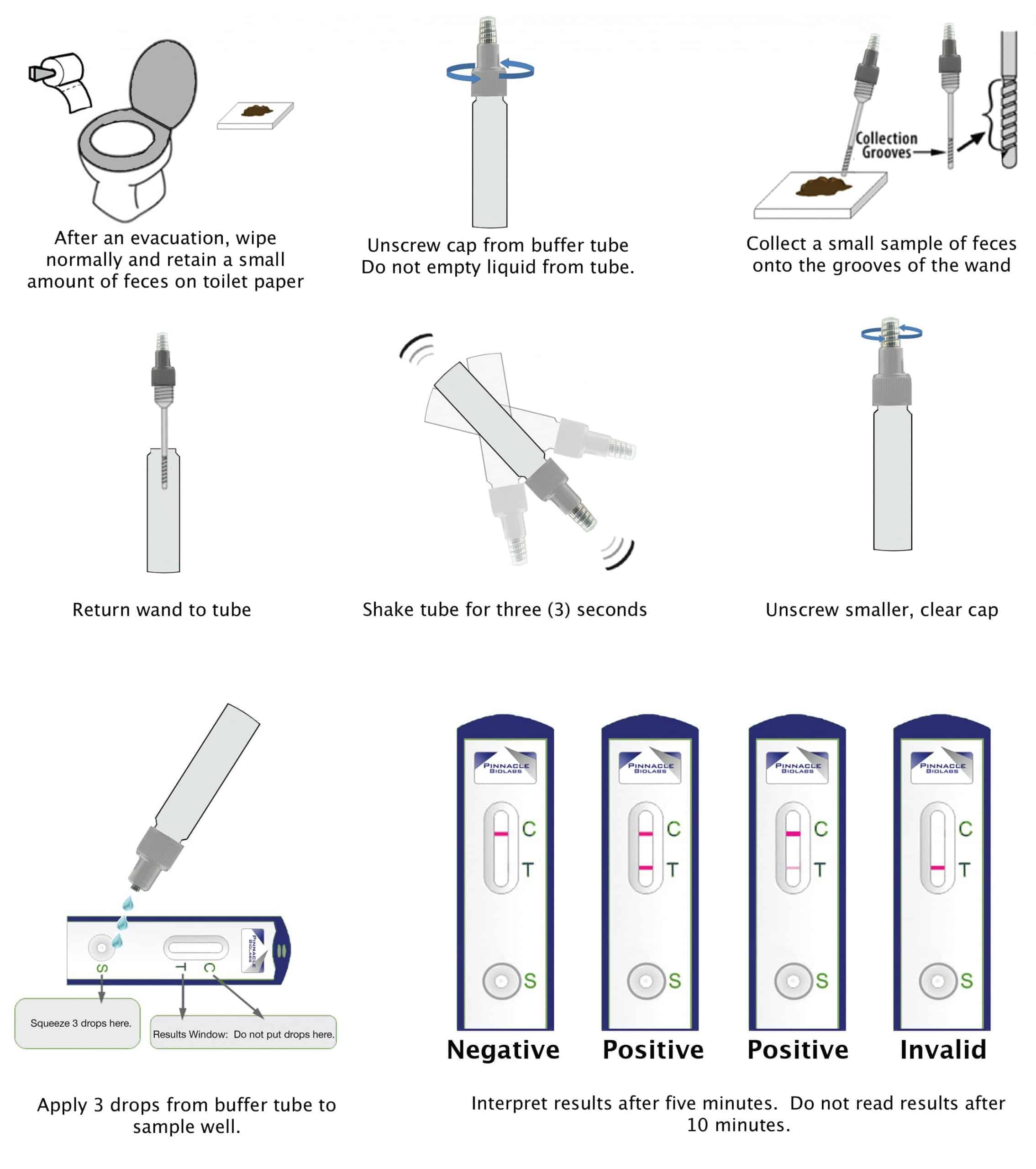
Why Have A Stool Test For Ibd
Although a stool test on its own cant diagnose IBD it can help give a picture of what might be going on in your body.
If you are experiencing IBD-type symptoms you may be asked to do a stool test to check to see if an infection is actually causing the symptoms.
Tests can also be done to see if you have increased levels of specific proteins, which can indicate inflammation in the body.
IBD can affect the digestive systems ability to absorb nutrients . A stool test can also be done to help give an indication if this is the case.
If you have IBD you may be asked to do stool tests as a way of monitoring and measuring the effectiveness of your treatment.
I Would Like To Start A Family Should I Be Worried About My Disease Or Medications That I Take
Most patients with Ulcerative Colitis or Crohns disease can expect to have a normal pregnancy and a healthy baby however there may be some risks. It is important for your discuss your pregnancy with the hospital IBD team. It is important not to stop any medication until you have spoken to your team. There is also some useful information sheets on the Crohns and Colitis UK website .
Also Check: How Do You Get Rid Of A Peptic Ulcer
How Does The Fecal Calprotectin Accurately Diagnose Or Monitor Ibd
After your stool is analyzed, your doctor will look at your test results and determine whether your levels of calprotectin are normal , borderline, or abnormal . A high level can indicate IBD, whereas a lower level can indicate a functional bowel disease such as IBS.
Lets take a closer look at the levels:
- Low or normal levels may indicate that that there is no inflammation, and you are in remission OR if you are having symptoms, that these symptoms are not caused by inflammation . Knowing this will help to exclude IBD, and avoid unnecessary referrals and colonoscopies.
- Moderate or borderline levels can indicate that some inflammation is present and could be due to treated inflammatory bowel disease or associated with the usage of nonsteroidal anti-inflammatory drugs , aspirin, or proton-pump inhibitors. For patients with moderate levels and clinical symptoms suggestive of IBD, retesting in 4 to 6 weeks may be needed.
- High or abnormal levels can suggest that you have active inflammation. High levels dont always explain the reason for inflammation so your doctor may order additional tests. An endoscopy may be indicated as a follow-up test to help determine the cause of inflammation, signs, and symptoms.
What Do I Do If I Flare In
There are some things that you can do to help manage your flare and you may have discussed some self-management techniques with the IBD team previously.Its likely that we may need to complete some tests to include blood tests and a faecal calprotectin stool sample. We would want you to contact us in the event of a flare so we can decide the best course of action. There is an advice line for all patients on 01625 661653. Messages can be left on this answerphone. Another way of contacting us is via email on . Please bear in mind that whilst we do try to answer enquiries in a timely manner, the nature of condition means that sometimes we have address the enquiries of the patients with the most pressing needs first.
Also Check: Whey Protein And Ulcerative Colitis
I Dont Like The Idea Of Using A Suppository Or Enema Is This Necessary
Rectal treatment, suppositories or enemas, are often used to treat inflammatory bowel disease particularly if your disease just affects the left side of the large bowel. The rectal treatments can be used alone or in combination with oral medication to treat your condition. They can be very effective in getting a high concentration of the drug exactly where it needs to be and can lead to faster resolution of your symptoms. Using them just before bedtime or after a hot shower , may make them easier to use. KY lubricating gel or some water can be applied to the applicator or suppository before insertion. If your bottom is sore your GP can prescribe some gel that has a local anaesthetic in it, such as instillagel.
What To Expect During A Colonoscopy
About 24 hours before a colonoscopy, you will be asked to clear your bowels with laxatives, enemas, or an all-liquid diet. Be sure to follow the fasting instructions given to you by your healthcare provider.
On the day of the procedure, you will be asked to change into a hospital gown and given a sedative and pain medication, either orally by pill or intravenously . In most cases, you will be awake during the procedure.
Once sedated, your doctor will ask you to lie on your left side, insert the colonoscope through the rectum and use the tool to take pictures. They will also remove any polyps and tissue samples.
The procedure usually takes about 30 minutes, and then you will moved to a recovery room to allow the sedative to wear off. Typically, you will be able to go home the same day.
Recommended Reading: How To Get Rid Of Stomach Ulcers
Initial Testing And Evaluation
Your doctor will conduct a physical exam and ask you questions about your general health, diet, family history, home environment, and your daily activities.
Your doctor may then recommend a series of diagnostic tests. In addition to diagnosing ulcerative colitis, these tests are also performed to rule out infection.
How Is Ulcerative Colitis Diagnosed
Colitis shares many symptoms with other common conditions, such as Crohns disease, irritable bowel syndrome, gastroenteritis and coeliac disease. Your doctor will examine you and take a detailed history of your symptoms to help rule these out.
There is no single test that can be used to diagnose UC, so a combination of tests is usually required:
- Blood tests help to rule out other medical conditions, and certain markers in the blood can indicate that inflammation is present.
- A stool sample may find other possible causes of diarrhoea and inflammation, such as an infection.
- A colonoscopy may be performed, where a thin, flexible tube that contains a tiny camera looks inside the bowel for ulcers, inflammation and bleeding.
- A biopsy may be taken from inside the bowel so a pathologist can examine it under a microscope to look for signs of disease.
Other types of imaging are sometimes used to help in the diagnosis and to help rule out other diseases.
Read Also: Mouth Ulcer Vitamin B Complex
Also Check: What Foods Do You Avoid If You Have An Ulcer